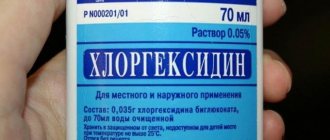
Chlorhexidine is an effective antiseptic drug used in traditional medicine. It is used in gynecology, dermatology, and also in dentistry to combat various types of bacteria. Available in solution form, Chlorhexidine is often used for gum inflammation.
How to rinse your mouth with Chlorhexidine for gum inflammation
What is Chlorhexidine used for?
An aqueous solution is prescribed to be taken in the following cases:
- cervical erosion;
- for the prevention of syphilis, genital herpes and other vaginal diseases;
- disinfection of dentures, disinfection of wounds;
- various diseases of the oral cavity.
An alcohol solution is used to treat hands and medical devices before surgery. The solution is also used to treat the working surface of medical equipment.
Vaginal suppositories are effective for the following conditions:
- in order to prevent infections that can be transmitted as a result of unprotected sexual intercourse;
- bacterial vaginosis;
- prevention of inflammation and infections before surgery, childbirth or abortion.
What is more effective against coronavirus – chlorhexidine, miramistin or hydrogen peroxide
Chlorhexidine and Miramistin are antiseptics that many consider to be analogues. In fact, these drugs differ in the active substance: for Chlorhexidine it is chlorhexidine bigluconate (a salt of gluconic acid), and for Miramistin it is benzyldimethyl [3-(myristoylamino)propyl] ammonium chloride monohydrate.
As a result of experiments to determine the MIC (minimum inhibitory concentrations) of various antiseptics against test cultures of human coronaviruses in vitro, it was found that Miramistin is 5 times more effective than chlorhexidine (Table 1).
But it is not advisable to use Miramistin instead of chlorhexidine - it is 20 - 30 times more expensive. In addition, it is not intended for use on hands.
Hydrogen peroxide is an antiseptic for external use, known for its powerful oxidizing properties. It destroys the lipid membranes of cells, so it is suitable for fighting coronavirus.
Hydrogen peroxide is a cheap and effective antiseptic against the COVID-19 virus. Unlike chlorhexidine, it has a short-term effect rather than a prolonged one (up to 4 hours). It is very aggressive towards the skin, so it can only be used to disinfect objects with surfaces made of non-porous materials.
A three percent solution of hydrogen peroxide can be used to disinfect surfaces and prepare skin disinfectants with your own hands.
How to use Chlorhexidine in gynecology
The product is actively used to prevent sexually transmitted diseases. No later than 2 hours after unprotected intercourse, you need to take the solution. Men will need to insert 2 ml into the urinary canal, and women will need to insert 2 ml into the urinary canal and another 5-7 ml into the vagina. It is recommended to wipe the skin around the genitals with the solution. The instructions say that after using the drug you need to wait 2 hours before urinating. Otherwise, the effect of use will be less.
For preventive purposes, vaginal suppositories can be used.
Before using the product for thrush and other gynecological pathologies, you should consult a specialist in advance.
A complete overview of the useful product: scope, rules of use and main indications
Even simple tooth extraction inevitably leads to tissue trauma. Therefore, after the procedure, it is very important to follow the doctor’s recommendations to prevent infection of the open wound, inflammation of surrounding tissues and the development of other complications. One of the main aspects of prevention during the rehabilitation period is maintaining hygiene with regular antiseptic treatment of the oral cavity. For this purpose, specialists usually prescribe antibacterial solutions for rinses and mouth baths, for example, Chlorhexidine. Further in the article, read about the indications for use of the product, its pros and cons, precautions, as well as how to properly rinse your mouth with Chlorhexidine after tooth extraction.
Contraindications and adverse reactions
Taking the drug is contraindicated in the following cases:
- increased susceptibility to the components included in the composition;
- patients with dermatitis;
- simultaneous use with other antiseptics, for example, hydrogen peroxide;
- in ophthalmology for washing the eyes.
It is better to refrain from using the product to disinfect the surgical field before or after surgery on the central nervous system and auditory canal.
In pediatrics, the drug is used with great caution.
Some patients may experience undesirable reactions such as:
- dry skin;
- allergic skin rashes;
- itching of the skin;
- light sensitivity.
With prolonged use of the product in dentistry, changes in taste may occur, tartar may appear, or teeth may become stained.
Infections caused by antibiotic-resistant microflora represent an ever-growing threat in both hospital and community settings. Nosocomial infections lead to a decrease in the effectiveness of therapy, an increase in the duration of hospitalization and an increase in mortality.
Chlorhexidine bigluconate was developed in Great Britain in 1950. It is the first internationally recognized antiseptic for skin and wounds. One of the advantages of chlorhexidine, in addition to its pronounced antimicrobial effect, is its ability to bind to various biological substrates while maintaining its antibacterial activity, and then be slowly released, which leads to the preservation of effective concentrations of the drug. To date, there are no reports of resistance to chlorhexidine, despite more than 60 years of active use of the drug in the clinic. Chlorhexidine gluconate remains important in the prevention of nosocomial infections.
Widespread use of antiseptic methods for the prevention and treatment of infections followed the publication of Joseph Lister's The Antiseptic Principle in Surgical Practice in 1867. At the same time, “Lister’s antiseptics” met ardent opponents, whose main argument was the toxicity of the antiseptic they used (carbolic acid). Despite the availability of numerous antiseptics, the question of the safety and effectiveness of this group of drugs remains constantly relevant. The “longevity” of chlorhexidine and the prospects for its further use as one of the most powerful antiseptics widely used in clinical practice is a pressing issue for clinicians.
A cationic detergent (detergent), later named chlorhexidine, was synthesized during the development of antimalarial drugs in 1947. This compound has bactericidal antimicrobial activity, especially against gram-positive microorganisms. Of the 10,040 compounds, the first to enter the market was chlorhexidine gluconate, registered in 1954 by Imperial Chemical Industries Co.LTD (UK) as “Gibitan” - the first internationally recognized antiseptic for the treatment of wound surfaces and skin. In 1957, only 3 years after entering the market, the indications for its use were expanded to include not only skin treatment, but also use in ophthalmology, urology, gynecology and otorhinolaryngology. In 1959, chlorhexidine began to be used to control bacterial plaque, leading to its widespread use in dentistry. Currently, in clinical practice, chlorhexidine is preferred not only when treating the skin (hands, surgical field), but also as an oral antiseptic, including for the prevention of nosocomial infection. The most commonly used concentrations are 0.2% and 0.12% solutions. In addition to its effect on plaque and gum condition (gingivitis), chlorhexidine is effective in the prevention and treatment of caries, secondary infections after dental procedures or implant placement. Chlorhexidine reduces the bacterial load and the risk of bacteremia after dental procedures. It is also used in the treatment of recurrent atrophic stomatitis and stomatitis associated with the installation of dentures, primarily in groups of patients with orthodontic appliances and immune disorders. One of the main advantages of chlorhexidine, in addition to its powerful antimicrobial effect, is its ability to retain its antimicrobial activity when bound to various substrates. At the same time, it is released slowly while maintaining an effective concentration. This property is known as substantiveness. Chlorhexidine is not susceptible to blood, pus, or saliva. Chlorhexidine is pharmaceutically incompatible with soap and detergents (for example, those containing lauryl sulfate), alkalis and other anionic compounds (colloids, gum arabic, carboxymethylcellulose), and iodine. Compatible with ethyl alcohol, benzalkonium chloride (contained in contraceptives for local use Pharmatex and Benatex). Ethanol enhances the effectiveness of the drug. The bactericidal effect increases with increasing temperature. At temperatures above 100°C, the drug partially decomposes. Used in a neutral environment; at pH 5-8 the difference in activity is small; at pH above 8 it precipitates. The use of hard water reduces bactericidal properties. Compatible with drugs containing a cationic group (benzalkonium chloride, cetrimonium bromide).
The unique combination of properties of chlorhexidine also determines the variety of dosage forms.
Chlorhexidine is available in the following forms: • 20% concentrated solution – intended for dilution before use, used in medical institutions; • 0.05% solution in plastic and glass bottles of 70 and 100 ml - used without dilution, including at home; • Vaginal suppositories (suppositories) “Heksikon” containing 0.016 g of chlorhexidine, 1 or 10 suppositories in a package; • Vaginal suppositories (suppositories) “Heksikon D” containing 0.008 g of chlorhexidine – intended for children, 10 suppositories per package; • Gel containing 0.5% chlorhexidine. Chlorhexidine is included in the following preparations: • Solutions for mouth rinsing for dental diseases and manipulations (tooth extraction, opening of abscesses, professional cleaning, etc.) – Elgidium, Amident, Eludril; • Gels for gums, intended for the treatment of dental diseases and pain relief in the oral cavity (for example, when getting used to dentures), one of the components of which is chlorhexidine - Dicloran Denta, Elugel, Metrohex, Parodium, Elgifluor, Dentamet, Metrogyl Denta; • Elgidium toothpaste; • Solutions with other antiseptics – Baktoderm (with benzalkonium chloride), Chlorhexidine alcohol spray – for the treatment of skin infections, Citeal (with hexamidine and chlorocresol) – for topical use in gynecology, dermatology; • Ointments Bepanten plus and Depantol (with panthenol - wound healing effect), Bemilon (with betamethasone - anti-inflammatory effect); • Vaginal suppositories Depantol (with panthenol) – used in gynecology after surgical interventions; • Chlorhexidine in combination with lidocaine for local anesthetic action in the Lidocaine-Asept spray and Instillagel and Kategel gels with lidocaine; • Lozenges for sore throat, stomatitis and other diseases of the oropharynx and oral cavity – Hexoral tabs, Anti-Angin formula, Sebidin.
What can be replaced - alternative options
"Chlogexidine" belongs to the class of inexpensive drugs, but it may not always be on hand or in the assortment of the pharmacy. Among analogues with identical active ingredients in their composition, experts identify the following medicines:
- “Instillagel” - along with chlorhexidine digluconate, the composition includes lidocaine, hydrochloride and auxiliary components. It has a pronounced bactericidal effect and gives an analgesic effect; it is often used as a local anesthetic during endoscopic examinations,
- "Baktosin" - the composition also contains a solution of cetrimide. The drug is available in liquid form and is prescribed as part of the treatment of purulent skin infections, as well as pathologies of the oral cavity and bacterial urological diseases,
- “Citeal” also contains chlorocresol and hexamidine diisothionate. Used for antiseptic treatment of skin and mucous membranes for bacterial and fungal infections.
There are other solutions, but they will already contain another active component. One of the most popular drugs belonging to this category is the drug Miramistin.
Action and effectiveness of the solution after tooth extraction
After removing a tooth from its socket, an open wound remains in the mouth, which quickly fills with blood. Next, a blood clot forms in it, which becomes a kind of protective barrier that prevents the penetration of bacteria and the spread of infection through injured tissue. When this clot does not fit too tightly to the socket, is damaged, falls out, or does not appear at all, the risk of developing serious complications - alveolitis, which can subsequently lead to osteomyelitis of the jaw and osteonecrosis, that is, gradual necrosis of bone structures, increases significantly.
The photo shows a blood clot after tooth extraction
The main reason for the development of this complication is insufficient oral hygiene during the rehabilitation period. Harmful microorganisms penetrate the alveoli and provoke inflammatory processes. To prevent this, after tooth extraction, the doctor prescribes oral baths using Chlorhexidine. The drug provides high-quality disinfection of all surfaces in the oral cavity, prevents the development and spread of pathological processes of an inflammatory nature.
How to properly prepare a solution for rinsing and mouth baths
Now pharmacies sell solutions that are ready for use - in a concentration of 0.05%. It is recommended to use one tablespoon of the product to treat oral tissues.
There are also solutions on sale at a concentration of 0.20% - they must be diluted before use. To do this, take 2.5 ml of concentrate (the exact volume can be measured using a regular syringe) and dilute it in a liter of water. The substance should be thoroughly mixed. If a burning sensation occurs while rinsing, you need to add a little more water. It is important to follow the recommended proportions so as not to cause soft tissue burns.