Installation of implants is a surgical operation that is performed under anesthesia. Most often, local anesthesia is used, that is, eliminating the sensitivity of tissue in the area of the upcoming invasive manipulation. Since the anesthetic lasts for several hours, numbness after implantation is quite normal. It may be associated with swelling, which often accompanies the installation of artificial roots in the jaw. As a rule, the numbness goes away as soon as the effect of the drug wears off. But if sensory impairment persists several days after surgery, this may indicate the development of one of the complications.
Why does numbness in the upper or lower jaw persist after implant installation?
Often, after placing an implant, temporary complications arise in the form of loss of sensitivity, aching pain, bleeding and redness of the gums, swelling - all this is a normal reaction to surgery. Usually paresthesia goes away without a trace after 3-5 hours, all other symptoms - after 4-6 days.
There is no need to delay a visit to the doctor if numbness lasts more than five hours . It can occur either due to the effect of anesthesia or due to:
- poor preparation for surgery, incorrect selection of implants, the site of their integration;
- injuries of the mandibular trigeminal nerve.
Symptoms and causes
The scientific name of this pathology is paresthesia. The main symptoms by which one can suspect the onset of the disease are: a burning sensation, the appearance of goosebumps and slight tingling in the soft tissues, numbness of part of the dentition or the entire jaw at once. This condition can be caused by many reasons. It is important to understand that numbness is not always a sign of a developing disease, but it is still worth seeing a doctor.
The main factors that provoke the loss of usual sensitivity: inflammatory processes in the root system, for example, periodontitis, severe injuries to the jaw, problems with the temporomandibular joint and malocclusion, disruption of the work algorithm during installation of implants, poor-quality dental treatment, stress and tension, violation integrity of nerves, etc.
Less common causes today are allergic reactions (to medications used by the dentist or to a sudden change in air temperature) and a significant outflow of blood from the head.
Anesthesia during surgery
Numbness prevents you from feeling pain during surgery. Achieved by administering anesthetic drugs. If sensitivity returns and the procedure has not yet come to an end, the drug is added to prolong the effect of local anesthesia.
In rare cases, a substance used for pain relief or improperly administered anesthesia can cause longer-term numbness - up to six months.
Alarms
The first signs of NAS damage are discomfort in the innervation zone (lower lip, cheek and gums in the lower jaw). There are 3 types of manifestations of the disease:
- anesthesia (absolute loss of sensation);
- dysesthesia (discomfort in the form of “pins and needles”, pain in the area of the affected NAS);
- paresthesia (decreased sensitivity: the patient does not feel pain when pricked with a needle).
Often, when removing figure eights, the lingual nerve is damaged. Sometimes this happens during implantation. Signs of the disease:
- uncontrolled tongue biting;
- violation of diction;
- decreased performance of taste buds;
- increased salivation.
Note: up to 90% of lingual nerve injuries do not require drug treatment. The pathology disappears on its own after 1.5-2 months.
Numbness from damage to the mandibular nerve
Symptoms
The following signs may indicate that the trigeminal nerve of the lower jaw is damaged during tooth implantation:
- prolonged numbness, which is accompanied by slight tingling;
- violation of facial expressions;
- difficulty swallowing;
- Difficulties in hygiene;
- painful sensations;
- increased salivation.
Sometimes nasal congestion may occur. The listed symptoms should be a reason to urgently consult a doctor.
Why is this happening?
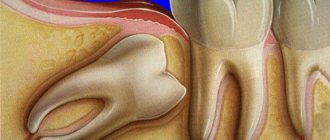
The trigeminal nerve may be damaged during dental implantation under the following circumstances:
- injured by a needle during the administration of anesthesia;
- pressed by an implant that is too long during screwing in;
- damaged by a drill while preparing a bed for an artificial root.
If the damage is minor, the tissue will go numb until the nerve fibers are restored. Sometimes this period lasts quite a long time - from 2 to 6 months.
Only a doctor can determine whether it is necessary to wait for spontaneous healing or whether surgical intervention is necessary to restore the integrity of the nerve fibers.
Expert opinion.
Victor Aleksandrovich, implant surgeon: “In dental implantology, cases of long-term numbness are rare. In my practice, such a situation arose only once. The patient had a numb lip on the left side for three weeks after implantation. We took an x-ray, which showed that the nerve fibers were not affected, but the implant was located very close, 1 mm from them. Neuromultivitis was chosen for treatment. Already on the 10th day, sensitivity began to return. The final recovery took three weeks.”
Stages of damage
There is a classification of jaw nerve injury:
- Neuropraxia is the mildest degree, manifested by partial loss of sensitivity, which lasts for several days.
- Axonotmesis is a deeper injury accompanied by pain. Paresthesia lasts for a month.
- Neurotmesis is a significant injury. A scar forms on the injured area as it heals. There are no sensations for 2 months.
When is a doctor needed?
Does tooth numbness persist after implantation? Are you worried about tingling in your mouth? These are some of the main signs of nerve damage, which requires urgent attention to a specialist. You should also consult your doctor if you have the following problems:
- intense pain when chewing and talking,
- decreased sensitivity of lips and tongue,
- difficulty swallowing,
- bleeding gums,
- increased salivation,
- violation of facial expressions,
- feeling of implant mobility.
The dentist will determine the cause of the problems and help eliminate them. If a nerve is damaged, it is necessary to act promptly. If measures are not taken promptly, numbness may persist for several months.
What to do, how to treat
Treatment of paresthesia due to unsuccessful implantation can be prescribed by the implantologist who performed the operation, dentist, neurologist, or physiotherapist.
Before moving on to restorative therapy, a diagnosis must be carried out, during which the nature and extent of the damage is established. The treatment is carried out comprehensively, aimed at restoring the conductivity and sensitivity of nerve fibers .
If the patient consults a doctor immediately, drug therapy in combination with physiotherapeutic procedures is very effective. In other cases, surgery is required.
Prevention
Unfortunately, modern dentistry has not come up with any special preventive measures aimed at reducing the risk of dental numbness. This is explained by the fact that the main causes of pathology are usually severe trauma and mechanical damage to the nerve during surgical procedures. However, it is still possible to minimize the risk of the disease; to do this, you should adhere to several rules.
If you need to undergo treatment or install an implant in place of a missing tooth, you need to choose a truly experienced specialist. After surgery, it is very important to give the body time to fully recover, so do not neglect rest. It is also not recommended to stay outside for a long time, especially in severe frost or gusty winds.
Teeth numbness is a rather unpleasant syndrome that can cause a lot of inconvenience to its owner. In most cases, the pathological process requires specialist supervision, as it does not go away on its own. If the problem is not properly addressed, numbness can develop into a more serious dental disease.
previous post
How to overcome your fear of dentists?
next entry
Complications during implant healing
The most serious complications are possible during the fusion of the implant surface with the jaw bone. Among them are the inflammatory process around the titanium analogue of the tooth root and its rejection.
Peri-implantitis
Inflammation of the tissues surrounding a dental implant is called peri-implantitis. The disease occurs due to infection in the space between the gum and the body of the implant. This is possible if the wall of the paranasal sinus is damaged, the postoperative wound is improperly closed, there is inflammation in the adjacent tooth, or inaccuracy in the manufacture of the crown. But the most common reason is a banal lack of oral hygiene by the patient. Inflammation is accompanied by the formation of swelling, bleeding, and pain. If there is no treatment at the initial stage, the disease becomes chronic. Then the infection “eats away” the jaw bone, and the implant becomes mobile. In this case, it is necessary to remove the artificial tooth and treat the hole. Peri-implantitis is a fairly rare phenomenon, occurring in 1–2% of cases*.
Implant failure
Failure of the jaw bone to accept a titanium rod implanted into it is characterized as rejection. The causes may be infectious processes around the implant (peri-implantitis), surgical trauma, lack of bone tissue, smoking immediately after surgery, exacerbation of chronic diseases, and, extremely rarely, an allergy to titanium. The onset of the rejection process can be identified by signs such as implant mobility and pain in the surgical area. In such cases, the artificial root is removed from the hole and a complex of vitamins is prescribed to strengthen the bones. Re-implantation is possible after 1 – 2 months. With a competent doctor’s approach and the patient’s compliance with all instructions, the chance of encountering this unpleasant problem is less than 1%*.
Paresthesia of the inferior alveolar nerve is characterized by loss of sensation in the area of the chin, lower lip and corner of the mouth on one side and occurs, as a rule, as a result of its injury during surgery, as well as partial or complete compression by the implant.
Unfortunately, even with all the necessary diagnostic and surgical equipment and extensive practical experience, this unpleasant complication cannot be completely excluded.
The main diagnosis of paresthesia → is the patient’s complaints! Sighting, orthopantomographic images and even computed tomography do not always allow a correct interpretation of the situation. I have repeatedly encountered clinical cases where the image showed the imposition of an implant on the projection of the mandibular canal, but there was no trace of paresthesia. Conversely, there are pronounced phenomena of numbness, and according to all x-ray data from the implant to the nerve there was at least 2–3 mm!
If nerve damage is detected directly during surgery and is associated with a long implant length, it is necessary to take an implant 2–3 mm shorter and cover the perforation with CollapAn before installing it.
Therefore, as soon as the patient expresses complaints of a corresponding nature, it is necessary to immediately proceed to action! Don’t waste your time, the faster and more actively you start treatment procedures, the faster you will get results!
So what should you do if a patient complains of paresthesia?
- facial massage for 10–14 days;
- physiotherapy (D'arsonval, UHF, etc.);
- neuromultivitis (first two weeks, 1 tablet 2 times a day,
- then another 2-3 weeks, 1 tablet per day);
- Traumeel-S (1 tablet 3 times a day for 3–4 weeks);
- Traumeel ointment (2-3 times a day for 3-4 weeks);
- Bryaconeel (1 tablet 3 times a day under the tongue for 3–4 weeks).
Remember that restoring nerve sensitivity is a long process! This treatment regimen can be safely extended to 2–3 months.
As practice shows, with the timely start of the described therapeutic actions, already within the first month the area of paresthesia is noticeably reduced, and after some time, patients stop paying attention to this phenomenon.
4.6.-1 Note the topography of the mandibular canal and the pronounced “knees” in the mesial direction. With such a bone height, even after augmentation, there remains a high probability of developing paresthesia after implantation.
4.6.-2 The implant “closes” the mandibular canal. In fact, this is just an overlay. There is no nerve damage and no paresthesia. The picture was taken 8 years after the operation due to the patient’s desire to install an implant in the area of tooth 16.
4.6.-3 In this case, the image shows only a point contact between the implant and the nerve, but there is paresthesia and is also accompanied by periodic pain symptoms.
4.6.-4 This CT scan shows partial compression of the inferior alveolar nerve by the implant in all projections, but the patient has no complaints.
4.6.-5 Two implants were installed in one operation. There was paresthesia on the right, but not on the left. Treatment was started on the 8th day after surgery. The phenomena of paresthesia completely disappeared only after 14 months.
4.6.-6 In this case, 2 implants were installed in the area of 46 and 47 teeth. Despite the patient's complaints, the decision to remove implant 47 was made only 2.5 months after the operation. By this time, the implant had already been integrated and, when removed, “pulled” the neurovascular trunk with it.