- What kind of disease is candidiasis?
- Symptoms
- Causes
- Treatment
- Therapy methods
- Preventive measures
Many parents are aware of such a common problem in children as thrush, which is characterized by the appearance of a white coating on the tissues of the oral cavity. In medicine, this pathological condition is called “candidiasis” and refers to fungal diseases. Candidiasis most often develops in a child’s mouth in the first year of life. The symptoms of thrush are very disturbing for the baby, but timely treatment allows you to get rid of the fungus quickly and without consequences.
What kind of disease is candidiasis?
According to statistics, about 30% of infants experience candidiasis. The causative agent of the disease is Candida fungus. These specific microorganisms are normally present in the body of every person, even in the absence of health problems, but only in small quantities.
Oral candidiasis in children is much more common, since the immune system of children is not yet formed and is not able to resist pathogenic microorganisms and the effects of negative external factors.
With weakened immunity and the concomitant influence of provoking factors, the fungus begins to actively multiply, affecting the mucous membranes. Without therapeutic treatment, candidiasis is eliminated in exceptional cases. Much more often, if thrush is not treated, complications arise, and the infection itself spreads throughout the body.
To prevent your baby from getting thrush
To prevent thrush from reaching the baby’s mucous membranes, special precautions must be taken:
- Regularly care for your child’s mucous membranes, monitor their condition when the baby is sick, and especially when he suffers from infectious diseases;
- If your child is prescribed antibacterial drugs, be sure to remember to use special means to protect the microflora;
- If candidiasis occurs during pregnancy in an expectant mother, it is necessary to urgently consult a doctor and undergo treatment. In addition, on the eve of birth, maternity hospitals carry out special prophylaxis for newborns with an increased risk of candidiasis. Thrush is especially susceptible to infants whose mothers suffer from chronic candidiasis and those who have foci of infection already in the immediate vicinity of birth. Mothers with inflammatory gynecological diseases or difficult childbirth can also transmit the risk of fungal infection to the newborn.
Symptoms
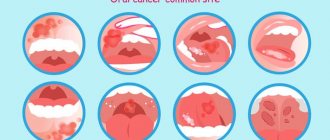
Oral candidiasis in children can have different forms of manifestation and severity of symptoms: mild, moderate and severe. As a rule, each form corresponds to the stage of development of the disease. If therapy is not carried out in a timely manner, the signs of fungal infection become more intense and the number of symptoms increases.
In mild forms of the disease, a red rash appears on the oral mucosa, which is covered with a white coating on top. At the next stage, the child experiences swelling of the tissues and the formation of localized white spots with a coating of curd consistency. Gradually these spots merge into a larger affected area. When plaque is removed, bleeding ulcers open. If thrush starts, the fungus spreads to the entire oral cavity, including the lips, tongue and throat. All fabrics are completely covered with a curd coating.
Common symptoms of candidiasis in children include:
- burning and itching sensation in the mouth;
- discomfort and pain when eating;
- frequent regurgitation in babies;
- formation of cracks in the corners of the lips;
- temperature increase.
Children in the first two years of life report their condition by refusing to eat, constant whims and crying for no reason. It is not difficult to see the signs of candidiasis, so if a child has a sharp rise in temperature or refuses to eat, pediatricians and dentists recommend checking the oral cavity for the presence of white plaque. If you suspect thrush, it is not advisable to delay a visit to a specialist, since the fungal infection progresses quickly.
Prevention
Everyone who gives birth should know how important hygienic cleaning of the child’s oral cavity is. This procedure cannot be ignored. It can prevent many dental diseases. Therefore, do not miss visits to the dentist! Only a doctor can notice problems at an early stage. Treatment started on time will be faster and easier.
Compliance with preventive measures minimizes the risk of pathology. During the period of bearing a child, the expectant mother needs to take care of her health, pay close attention to oral hygiene procedures, and not introduce into the diet those foods that create a favorable atmosphere for the activation of fungi. Prevents problems:
- Refusal of artificial feeding, transition to breastfeeding;
- Before feeding the baby, the breasts should be treated with a solution of baking soda;
- Pacifiers, pacifiers, and bottles should be sterilized;
- After the baby has eaten, you need to give him boiled warm water to drink, which will wash away the remaining milk from the mucous membrane.
Causes
The main reason for the development of candidiasis of the oral mucosa in children is weakened immunity. If a baby is born premature, the likelihood of developing thrush is very high. Children who are breastfed or have congenital pathologies are also often exposed to fungal infections.
Provoking factors include:
- the presence of vaginal candidiasis in the mother during pregnancy (the child can become infected when passing through the birth canal);
- insufficient hygiene of the female breast during breastfeeding (the fungus is often localized specifically on the nipples due to the environment favorable for it);
- poor handling of the child’s initial things (bottles, pacifiers, etc.);
- parents’ habit of licking nipples (even if the adult has no signs of thrush, there may be a fungus in the mouth that can be passed on to the child);
- long-term use of drugs from the “antibiotics” group (medicines help reduce one’s own immunity);
- frequent regurgitation in infants (after regurgitation, an increased acidic environment will remain inside the oral cavity, favorable for fungus);
- excessive and frequent dry mouth (lack of saliva as a protective agent against the activity of pathological microorganisms).
Infection with Candida fungus in children over 2 years of age can occur as a result of consuming unwashed foods, raw milk or running water. If a child over 3 years of age suddenly shows signs of thrush, they should be examined not only for a fungal infection, but also for other possible diseases that may be accompanied by a “decay” of the immune system.
Features of the oral cavity
The mucous membrane of a healthy child's mouth is bright pink due to the large number of blood vessels. As she grows older, her shade fades.
The epithelial layer is distinguished by tenderness and vulnerability, as well as some dryness due to the not very active work of the salivary glands (up to 3-4 months).
The baby's mouth is ideally suited for sucking. A wide tongue, a fold on the gums formed by the mucous membrane, pads on the inside of the lips, a “suction cup” on the upper lip - all this provides a tight grip on the bottle or nipple and facilitates the process of obtaining food.
What features or problems can be detected by looking into a baby’s mouth? Main options:
- white bumps on the palate;
- abnormal appearance or position of the tongue;
- white plaque on the inside of the mouth.
Treatment
Fungal diseases in children can be treated by a pediatrician, an infectious disease specialist or a dermatologist. If we are talking about the treatment of oral thrush, then therapy can also be carried out by a dentist.
The diagnosis of candidiasis is determined in most cases based on an examination of the oral cavity performed by a specialist. If there is any doubt, the doctor refers the patient for additional examinations. More often, to confirm the disease, a laboratory test is used to test a smear taken from the mouth for the presence of fungus.
Treatment of thrush in children requires an integrated approach. If the disease is not advanced, then local therapy is carried out in combination with measures to strengthen the immune system. In severe cases, oral candidiasis in children is treated with systemic drugs, local agents and compliance with preventive recommendations.
Treatment of white plaque on the palate of a child
The white spots will disappear if the cause of the problem is eliminated. If you regurgitate frequently, for example, you should change your feeding method and sterilize your utensils. A small area of fungal infection is treated with topical preparations. Severe forms of the disease are treated medicinally using complex drugs. Fungal diseases are dealt with:
- Clotrimazole;
- Candide;
- Pimafucin;
- Fluconazole;
- Diflucan;
A sterile gauze ball is moistened with the solution. They gently wipe the oral cavity several times a day. The duration of therapy depends on the complexity of the situation. Treatment usually lasts 7-10 days. Irrigation or lubrication is also prescribed. To boost the body’s defenses, doctors recommend vitamin complexes and probiotics for children. This will restore the natural microflora in the intestines.
Therapy methods
Treatment of candidiasis begins with treatment of the oral cavity. The first procedure is performed by a specialist at the appointment. Antiseptic agents are used to remove plaque. The doctor may then apply an antifungal agent.
The parent should closely monitor the dentist’s actions, since in the future they will have to treat the oral cavity themselves at home. The necessary medications will be prescribed by a specialist. Local antifungal agents are dangerous in case of overdose, especially for children, so you must strictly follow your doctor’s recommendations.
In advanced cases, medications are prescribed in the form of solutions, drops or tablets. There are few drugs available to treat candidiasis in children. Replacing them with adult counterparts is also dangerous. The dosage must be strictly observed.
A mandatory addition to the main therapy is maintaining good hygiene, good sleep, proper nutrition and taking measures to strengthen the immune system (eating healthy foods, taking pharmaceutical vitamins if necessary, walking, etc.).
How to treat oral thrush in infants
Treatment of oral thrush in an infant is not a complicated process, but it requires the systematic implementation of certain procedures several times a day until the child recovers. If you find a mild degree of thrush in your baby, but at the moment you cannot call a doctor (for example, on a day off), then you can use traditional methods of eliminating thrush. If the degree of damage to the mucous membrane has already reached serious forms, it is better not to risk it and call an ambulance.
Traditional methods for eliminating thrush:
- using a soda solution: prepare a solution (dissolve 1 teaspoon of soda in a glass of warm boiled water), then wrap a sterile bandage around your finger, moisten the winding in the solution and very carefully wipe the areas of fungal infections; Do not rub them under any circumstances, because under the plaque there may be bleeding plaques, through which you risk allowing bacteria to enter the baby’s body; such light rubbing can be done 4 times a day until you have the opportunity to visit a doctor;
- use of honey solution: prepare a solution (dissolve 1 tsp honey in 2 tsp warm boiled water); however, please note that it is unacceptable to use a honey solution if a child is allergic to bee products; if the child tolerates honey well, then treatment with the solution can be carried out similarly to treatment with soda; You can also treat your baby’s pacifiers and toys, which he likes to put in his mouth, with any of these solutions;
- for candidiasis of the nipples, treat them with any of the above solutions;
- You can use other natural antiseptics for rinsing and treating the oral cavity - for example, herbal infusions; you can prepare a decoction of chamomile, green tea, calendula, taking 1 tsp. dry herbs for 1 cup of boiling water; Sage, elecampane, yarrow, burdock, and oak bark also have antiseptic properties, but it is also necessary to understand that any of the herbal preparations can cause an allergic reaction;
- sometimes the contents of aloe vera stems are used as antiseptics, lubricating the affected areas with this juice;
- Among the natural oils that can be used to lubricate the oral cavity, rosehip, flax or peach oils can be used after rinsing or treating plaque.
Skin candidiasis
The disease in infants is often mistaken for allergic dermatitis. The disease occurs with a frequency of 10 to 24% and usually manifests itself at 2 to 3 weeks of a child’s life. Its distinctive feature is the predominance of the erythematous form of inflammation.
Skin candidiasis in children can be congenital or acquired. It occurs in erythematous or vesicular forms. It has several variants of the course - damage to large folds and candidiasis diaper dermatitis.
Congenital candidal dermatitis in children appears more often on the second day of life. With cephalic presentation, the skin of the upper part of the body is affected: face, head, upper back. The mucous membranes are not affected.
Acquired candidal dermatitis in children begins with large folds and always occurs with thrush in the mouth. In the absence of adequate treatment, the infectious process spreads to the smooth skin of the thighs, abdomen and back. In advanced cases, the entire skin is affected. The disease should be distinguished from bacterial diaper rash, which is characterized by weeping, which is not characteristic of skin candidiasis and the absence of peripheral foci of screening and other dermatomycosis in newborns.
Diagnosis of mycosis is based on the detection of pseudomycelium and budding candida cells by microscopy and/or isolation of pathogen cultures.
The vesicular form is characterized by the appearance of a significant number of flabby and small bubbles against the background of hyperemia.
The erythematous variant of inflammation is characterized by the appearance on the skin of smooth, shiny, moist, tense areas of a dark red color. Dark red color of the lesions, distinct borders, scalloped edges, varnish shine, a moist rather than weeping surface, a narrow border of desquamated epithelium along the periphery, the presence of dropout foci (erosions and fresh blisters) along the periphery, absence of dryness and itching even in cases of widespread lesions are the distinctive features of skin candidiasis in children.
Rice. 12. Erythematous form of skin candidiasis in infants (diaper dermatitis).
Rice. 13. Vesicular form of skin candidiasis in a child.
Candidal dermatitis of large folds
Damage to the skin of large folds begins with redness and swelling, against which small blisters and pockets of screening appear along the periphery. Candidal dermatitis is often mistaken for diaper rash. Clear lesions with scalloped edges, a tense, smooth and shiny surface and the presence of desquamated epithelium (epidermal corolla) along the edge of the white border are its distinctive features.
Rice. 14. Erythematous form of candidal dermatitis.
Candidiasis diaper dermatitis
The disease often develops in children who carry candidiasis in the intestines. On the skin, as a result of massive fusion of vesicles and lesions, erythematous plaques with a fringed, clearly defined edge appear, along the periphery there are foci of screening.
Typically, the infectious process involves the perianal area, inguinal folds, perineum and lower abdominal wall. In boys, the skin of the penis and scrotum is affected, in girls - the vagina and labia.
Rice. 15. Erythematous form of skin candidiasis in infants.
Treatment of skin candidiasis in children
To treat the disease in newborns, antifungal drugs are used in the form of creams and ointments: Ketoconazole, Isoconazole, Clotrimazole, Econazole, Sertaconazole. At the same time, oral thrush and intestinal candidiasis are treated. For congenital candidiasis and severe condition of the newborn, Fluconazole is used orally or intravenously. If there is no effect, Amphotericin is prescribed.
Rice. 16. Skin candidiasis in a child (inflammation of the periungual ridges).
Candidiasis of the intestines and other digestive organs
After Candida damage to the skin and visible mucous membranes, candidiasis of the gastrointestinal tract in infants ranks third. Carriage of microorganisms is quite common when the pathogens do not cause disease. Good immunity inhibits the development of the infectious process. But under certain circumstances, weakened children may develop candidal esophagitis (inflammation of the esophagus), gastroduodenitis (inflammation of the stomach and duodenum), enteritis (inflammation of the small intestine), enterocolitis (inflammation of the small and large intestines).
Factors contributing to the development of gastrointestinal candidiasis
The following factors contribute to the development of intestinal candidiasis:
- An imbalance between Candida colonization in the intestines and defense mechanisms that prevent excessive growth of microorganisms.
- The presence of physiological intestinal dysbiosis.
- Features of the structure of the mucous membrane in newborns. Failure of its protective and secretory functions.
- Long-term antibiotic therapy leads to the death of “good” bacteria and excessive growth of opportunistic flora, including fungi.
Signs and symptoms of candidal esophagitis
The disease may be asymptomatic or have nonspecific manifestations. Classic typical manifestations of candidal esophagitis are recorded extremely rarely. The infectious process develops in children born to mothers with vaginal candidiasis on the second day of life. Lack of appetite, refusal to breastfeed, excessive regurgitation containing whitish lumps, vomiting and rapid increase in dehydration are the main symptoms of the disease. Toxicosis is slightly expressed.
The basis of diagnosis is fibroesophagogastroscopy and culture of vomit on nutritional media in order to identify fungi of the genus Candida.
Rice. 10. Microscopy reveals pseudomycelium of Candida b and budding cells (photo on the left); when inoculating the vomit, an increase in colonies of pathogens is noted (photo on the right).
Signs and symptoms of intestinal candidiasis
Intestinal candidiasis in children occurs with symptoms such as lack of appetite (sometimes infants completely refuse to eat), regurgitation and vomiting, pain, bloating and rumbling in the abdomen, and loose stools. The vomit contains greenish or whitish mucus, and the stool contains yellowish-greenish mucus and white lumps. The smell of stool is normal. Symptoms of toxicosis are mild or absent. Microscopy of vomit and feces reveals fungal mycelium and budding pathogen cells. Candida is isolated from feces in crops in quantities of more than 10 4–5 CFU/ml.
In more than half of infants, intestinal candidiasis is combined with lesions of the skin around the anus, buttocks and visible mucous membranes.
Rice. 11. Often in infants, intestinal candidiasis affects the skin around the anus and buttocks.
Treatment of candidiasis of the gastrointestinal tract
In the non-invasive form of candidiasis, fungal cells do not form pseudomycelium and do not germinate the intestinal mucous layer. They multiply intensively in the lumen of the organ, disrupting cavity and parietal digestion. Treatment in this case is carried out with antifungal drugs that are not absorbed from the intestinal lumen - Nystatin.
In the invasive form of intestinal candidiasis, candida germinates the epithelial layer and penetrates beyond the basement membrane. The pathogens then enter the lymphatic system and bloodstream and spread throughout the body. In this case, Flucanazole, Ketoconazole and Intraconazole are effective.
The drugs are completely absorbed in the upper gastrointestinal tract.
If treatment is ineffective in children in intensive care units, Amphotericin B is used intravenously to treat candidiasis. For intestinal candidiasis in newborns, the drug is rarely used due to its high toxicity.
To correct the composition of intestinal microflora, probiotics are used. Immunocorrectors are used according to indications.