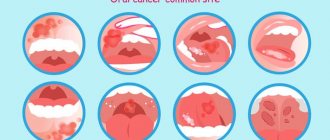
Stomatitis in a child is a very common phenomenon caused by an inflammatory process of the oral mucosa, which also occurs in newborns. We can say that raising a child and not knowing what stomatitis looks like in children is almost impossible. Quite often, the symptoms of the disease initially resemble those of a respiratory infection with a characteristic fever, stuffy nose and poor appetite. But after a short time, parents notice the appearance of blisters and ulcers on the gums, cheeks and inner lips, which can be caused by various pathogens. The child behaves anxiously, capriciously, sleeps poorly... Even for an adult, it is very difficult to endure the painful sensations that arise from stomatitis, not to mention children, who cannot always clearly explain what is tormenting them. Parents, of course, are concerned about the question of what causes stomatitis in children and whether the occurrence of such a disease can be prevented. Let's try to understand this thoroughly.
Types of stomatitis
Everyone is more accustomed to saying “stomatitis”, but it would be more correct to say “stomatitis”, since this is a generalizing concept for a whole group of diseases. Depending on the causes of stomatitis, it can be divided into several types, each of which has a number of characteristics.
Viral or herpetic stomatitis in children
One of the most common types of stomatitis in children is caused by the herpes simplex virus. Typically, a child becomes infected through airborne droplets. In addition, the virus is transmitted through dishes, toys, and household items. Most often, herpetic stomatitis appears in a child between the ages of one and four years. The disease begins with a cold, accompanied by lethargy and increased body temperature. Sometimes there is a runny nose and cough. Around the second day, small round or oval erosions of a light yellow color with a bright red border appear on the lips, tongue and inside of the cheeks. Swelling appears, the gums begin to bleed, and the child refuses to eat.
Traumatic stomatitis in a child
The disease is caused by mechanical trauma to the oral cavity. For example, burns from hot food, a too hard nipple, the habit of chewing a pencil. In addition, traumatic stomatitis often occurs in children with malocclusion due to frequent biting of the cheeks and tongue.
Candidal stomatitis
Appears in children under one year of age. The cause is Candida fungi. The main symptom is the appearance of a white coating in the baby’s mouth. It should be noted that this should not be confused with regular flowering after feeding. A cause for concern is if plaque persists and the baby refuses to eat.
Drug or allergic stomatitis in children
Caused by certain allergies or reactions to medications. If this type of disease is suspected, it is necessary to identify and remove the allergen, otherwise there is a risk of unpleasant consequences, including anaphylactic shock.
Each type of stomatitis is characterized by a certain childhood age. Young children often have candidiasis or fungus (thrush). At the age of “I want to know everything” in a child of 3-4 years, stomatitis is usually infectious in nature, when the infection is transmitted through dirty hands or objects. From one to four years, an acute herpetic form of the disease is often observed.
Causes of stomatitis in children
In childhood stomatitis, the mucous membrane of the oral cavity is affected: small, white or yellowish, fluid-filled pimples appear on its surface. In some cases, ulcers form.
Stomatitis is predominantly a childhood disease, although it can also occur in adults. The rash affects the inside of the cheeks, tongue and gums. The disease causes a lot of inconvenience: pimples hurt and itch, and their appearance is accompanied by a burning sensation in the mouth.
Among the main reasons for the development of stomatitis are:
- poor oral hygiene;
- mucosal injuries;
- diseases of the gastrointestinal tract;
- burns of the oral cavity;
- pathogenic bacteria that enter the oral cavity with dirty hands, toys, etc.
What can streptoderma be confused with?
Pyoderma
With pyoderma, the sebaceous and sweat glands are damaged. The rash appears in certain areas of the skin - parts of the body, scalp.
Herpetic rash
Herpes is characterized by the presence of blisters with constant inflammatory processes. They burst and provoke development.
Thrush or candidiasis
Candidiasis is characterized by erythematous papules or reddened, wet plaques. In the pathology under consideration, the lesion, as a rule, occurs in the mucous membranes or fold areas.
Manifestations of allergies
An allergic rash continues to occur as long as the influence is the causative agent of the allergy.
Symptoms of stomatitis
Signs of stomatitis in a child have a number of features characteristic of a particular type of disease.
Herpetic stomatitis in children is considered very common and usually manifests itself as follows:
- in the initial stage, the disease is confused with a cold due to increased body temperature, often runny nose and cough;
- the inflammatory process begins abruptly, manifested by headaches and pain in the mouth and muscles due to intoxication of the body;
- submandibular lymph nodes are enlarged and painful;
- feature - the formation of small bubbles filled with liquid.
Upon visual examination, redness of the gum tissue around the teeth, swelling of the mucous membrane and numerous vesicular rashes covered with a yellowish or whitish coating are noted. Candidal stomatitis in children can be clinically acute or mild. In this case, signs of stomatitis in a child appear as follows:
- very rarely an increase in temperature is recorded;
- in the oral cavity there are affected areas covered with a coating of cottage cheese;
- children behave restlessly, are capricious, refuse to eat;
- Locally similar stomatitis in children (or thrush, as it is often called) occurs on the tongue, cheeks, gums and inner lips).
Aphthous stomatitis in children is the most common form of the disease, but also difficult to treat due to the difficulty of identifying the specific pathogen. Similar stomatitis in children, the symptoms of which are more common in schoolchildren than in the younger age group, is characterized by the following symptoms:
- rash of single ulcers (feed) on the mucous membrane (on the cheeks, in the area of the tongue and the inside of the lips);
- Initially, such stomatitis in children in the mouth is manifested by characteristic redness, itching, burning, and an increase in temperature is also noted.
In this case, the ulcers do not look like blisters, but are whitish ulcers with a bright red outline around them. Then the ulcers are usually covered with a cloudy film, which can break through and cause a secondary infection, after which the baby’s condition will only worsen. Parents should know that stomatitis in a child is not a single type of infection with specific symptoms.
Each form of this inflammatory process has its own specific symptoms and causes. That is why, despite a number of individual similar points (temperature during stomatitis in a child, signs of inflammation of the mucous membrane, enlarged lymph nodes), the problem of treating stomatitis in a child is solved differently, taking into account the form of the disease.
general information
Streptodermia refers to a pathology caused by streptococci. If we talk about the external manifestations of the disease, blisters and purulent rashes that itch appear on the skin.
Streptoderma in children can occur in two different forms: acute and chronic. Acute is characterized by pronounced symptoms, and chronic - by periodicity.
According to the degree of damage, the disease is classified into superficial, deep and intertriginous. Each form has a specific feature.
Diagnosis of the disease
The pathology of stomatitis is diagnosed by infectious disease specialists, pediatricians, and pediatric dentists. The diagnosis is made on the basis of clinical and epidemiological data.
Based on materials from smears, scrapings, and blood, the following studies are carried out:
- virological;
- bacteriological;
- immunological;
- cytological.
Diagnostics such as polymerase chain reaction and enzyme immunoassay are performed. In some cases, the child has a blood test for the presence of sugar, and a consultation with an endocrinologist, allergist and other specialists is carried out.
Correctly conducted diagnostic examinations will help establish the correct diagnosis and prescribe effective treatment so that the situation does not worsen.
Possible complications.
More often, the disease passes without dangerous consequences for the patient. But with weak immunity, especially in young children, severe herpes sore throat can lead to serious complications caused by the spread of the virus to other organs:
- serous meningitis
- heart pain, myocarditis
- pyelonephritis
- encephalitis
- conjunctivitis.
To exclude the development of serous meningitis, you need to consult a neurologist; if you have heart complaints, you need to contact a pediatric cardiologist. If there are changes in the general urine test, you must make an appointment with a pediatric nephrologist.
With proper and effective treatment of herpes sore throat complicated by meningitis, the prognosis is usually favorable. But at the same time, the treatment of the youngest patients requires careful attention. With myocarditis the situation is more severe. Any complications of herpetic sore throat require the intervention of specialists!
Treatment of stomatitis in children
After a medical diagnosis of stomatitis in children under one year of age, a specialist prescribes highly effective drugs to combat the existing type of disease. Experts recommend that parents, at the first suspicion of stomatitis in a child, increase the amount the child drinks to irrigate the oral mucosa and remove toxins from the body. Clean drinking water without gas, fruit drinks or compotes that are not too sweet or sour; herbal teas are perfect for this. During this period, it is worth refusing to drink the child from concentrated juices and drinks with gas in order to avoid irritation of the mucous membrane.
After this, the specialist begins medical manipulations to cure stomatitis in the child.
Anesthesia
The first step is to numb the mucous membranes so that the child can eat and drink properly and generally reduce the child's stress level. Choline preparations with salicylate or lidocaine are commonly used as pain relievers in children. For this purpose, medications to facilitate teething, for example Kamistad or Dentinox gel, are suitable. Gel products are preferable for children because they are almost instantly absorbed into the mucosal tissue. Prepare with lidocaine in the form of a spray should not be used in children under one year of age - this may lead to bronchospasm.
Direct treatment of stomatitis
After anesthesia, you can begin treating your baby’s stomatitis. Firstly, all rashes and wounds must be treated with a special preparation, depending on the type of disease. Antiviral drugs are used for herpetic stomatitis, antibiotics and antiseptic drugs for bacterial stomatitis, antifungal drugs for candidal stomatitis. Not only the affected area, but also adjacent areas must be treated - this will stop the spread of the pathogenic process.
An important condition for eliminating infection is thorough and timely oral hygiene. The surface of the child's tongue and teeth should be brushed twice a day; experts recommend rinsing the mouth after every meal or drink. For young children, hygiene procedures are carried out using a piece of gauze or a silicone fingertip.
Treatment of allergic stomatitis
If a specialist has identified the presence of allergic stomatitis or severe swelling of the oral cavity is observed, then the drugs Fenistil, Suprastin, Diphenhydramine are used.
Treatment of viral stomatitis
For herpetic stomatitis, antiviral agents should be used in the form of ointments containing acyclovir - Gerpevir, Virolex, Acik, Viferon, oxolinic ointment.
For relapses of viral stomatitis, experts recommend a general strengthening of the immune system with the help of Immunal, Interferon, Viferon in suppositories. The duration of treatment and dosage of the drug is determined by the doctor. Often, medical experts recommend using the drug Cholisal in gel form. Perfectly relieves swelling, inflammation, pain, fever, eliminates pathogenic microflora. The drug does not contain sugar, has no taste and has a light anise aroma. To treat stomatitis in a child under one year old, it is necessary to rub a strip of gelatin preparation no more than 0.5 centimeters long into the palate, gums and inner surface of the cheeks, teeth, 2-3 times a day after brushing the teeth.
Treatment of candidal stomatitis
For candidal stomatitis, the doctor uses antifungal drugs in the form of an ointment, for example, Clotrimazole, Candida, Candizol, and often prescribes soda rinses.
This helps create an alkaline environment in the oral cavity, harmful to pathogenic fungal microflora. Procedures with soda are especially effective in the treatment of candidal stomatitis in children under the age of one year, because at this age most drugs are contraindicated. To treat the oral cavity, you need to dilute a teaspoon of soda in a glass of warm boiled water, then wrap a piece of gauze around a clean finger and wipe the palate, inner surface of the cheeks, gums and sublingual space of the child, periodically dipping your finger into the solution. The procedure should be done after every child eats or drinks. Older children can rinse their mouths with baking soda themselves.
Treatment of aphthous stomatitis
With aphthous stomatitis, the first priority is to unload the affected area and speed up the healing of the poop. An aqueous solution of blue (methylene blue) has long been used for this purpose. It is not recommended to use a blue alcohol solution for this, since the ethyl alcohol in its composition will cause poisoning or burn the baby’s mucous membrane.
Wounds are treated with a blue cotton swab 3-6 times a day.
Treatment of traumatic stomatitis
According to experts, traumatic stomatitis most often occurs in children 1-2 years old. This type of disease is accompanied by bacterial microflora, so the use of medicinal and antiseptic agents will be required. For children under 2 years of age, use Cholisal, Solcoseryl, Actovegin gel, and also wipe the oral cavity with a solution of chlorhexidine or soda.
Treatment of bacterial stomatitis
For the treatment of bacterial stomatitis, drugs such as Tantum Verde, Orasept and Hexoral in the form of a spray, Doctor Theiss and Septolete in the form of lozenges and many others are effective. Experts do not recommend using lozenges to treat children under 6 years of age due to the risk of asphyxia, and sprays are suitable for treating bacterial stomatitis in children over one year of age. Antiseptic rinses and gel preparations with metronidazole are also effective.
Among solutions with an antiseptic effect, the drug Miramistin is especially recommended, as it promotes the regeneration of the affected mucous membrane and eliminates most pathogens. The aerosol can is convenient for treating children under one year of age. To do this, you need to make 3 injections and rinse your mouth with them for several minutes 3-4 times a day. Babies under the age of one year are treated with gauze soaked in the drug.
Caring for a child with stomatitis
Parental involvement in treatment and proper care of children is not only important, but also necessary. With stomatitis, it is necessary to strictly follow the treatment plan, which is often very labor-intensive, so the result depends on parental care and control. The oral cavity is a kind of epicenter of pain, so it is not surprising that the child is very temperamental. Therefore, it is important for parents to be patient and persistent.
Most mothers and fathers are concerned about what to feed their child with stomatitis. Firstly, you need to eat only soft, warm and pasty foods, such as purees. The main thing is that the food is high in calories and not heavy, because the child’s immunity is already weakened. After eating, be sure to rinse your mouth so as not to provoke the development of stomatitis and not to add an additional infection. Spicy, sour, sweet and citrus foods should be excluded from the child's diet.
For stomatitis in children, it is necessary to relieve pain. This is done with the help of various medications to avoid food refusal and poor sleep. Also, for stomatitis in children, adequate oral treatment is very important. Your doctor should recommend how to handle your child and rinse his mouth.
Symptoms
If streptoderma occurs, what is the treatment? Before we know the treatment options, let's find out the symptoms. The disease in children occurs in extremely severe forms:
- temperature up to 39C,
- poisoning,
- large lymph nodes.
The texture of the skin may vary depending on the form of the pathology:
- Superficial. Initially, red spots form on the skin. After a couple of days they turn into blisters with a certain liquid inside. The blisters grow up to two cm in diameter, after which they rupture. Yellow crusts form in this area. After this, the skin in this area heals, and the pathology develops further.
- Dry streptoderma . This form usually occurs in boys. Light and pink spots up to 5 cm in diameter form on the skin. They are found everywhere on the body. After they disappear, scars may remain.
- Streptococcal infection. The pathology extends specifically to the corners of the lips; it is encountered when there is a deficiency of vitamin B. Small cracks form on the skin, causing discomfort. After some time, they form into pustules that become crusty. The child has difficulty consuming food, as it causes pain.
- Felon. In a situation where streptococcus spreads to the area around the nails, panaritium develops. Oddly enough, this disease is more often encountered by children at an early age who bite their nails.
- Streptococcal diaper rash. This form of pathology is typical for breastfed children. Blisters form in the folds of the skin.
Understanding how streptoderma begins to develop in children, treatment which requires timely contact with a dermatologist and the implementation of therapeutic actions, not a minute can be lost. If you constantly put off going to the doctor, the pathology can develop into a chronic form, and it will be almost impossible to achieve a final cure.
streptoderma, treatment
Prevention of stomatitis in children
Irritative stomatitis can be prevented with good oral hygiene, regular dental check-ups and proper nutrition. Because many adults and children carry the herpes virus and can transmit it even without symptoms, there is no practical way to prevent herpetic stomatitis. However, parents may discourage their child from kissing, eating, or playing in close contact with people who have an active herpes infection.
Ulcers can be minimized by teaching children to avoid injury, even minor trauma to the mouth. If our doctor determines that a child has a nutritional deficiency, parents can make sure the child is taking appropriate supplements and eating recommended foods. It won’t hurt to visit the dentist once every six months if we have previously discovered stomatitis in the child. Regular visits to our clinic will help prevent serious complications and detect the disease in time.