To develop the correct treatment tactics, it is necessary to make a correct diagnosis: this guarantees half of its success. To diagnose sinusitis, certain standards have been created, including, among other things, radiography of the nasal sinuses. This is an ordinary x-ray - a picture familiar to everyone.
The advantages of this type of research are obvious:
- diagnostic efficiency;
- relative safety;
- painlessness;
- simplicity of the procedure;
- lack of intervention in the body using surgical and endoscopic instruments;
- low cost;
- accessibility, which is important for residents of remote areas who are deprived of the opportunity to undergo high-tech examinations, for example, computed tomography or magnetic resonance imaging.
Location and functions of the maxillary sinuses
The maxillary sinus is also called the maxillary sinus. It is a paired paranasal sinus of the nasal cavity. It is located almost throughout the entire space of the maxillary bone, inside the upper jaw. The sinuses consist of the nasal, facial and orbital, posterior and inferior walls.
The maxillary sinuses are lined from the inside with a mucous membrane, which is represented by ciliated epithelium.
There are few nerves and blood vessels in this area. Therefore, inflammatory diseases of the paranasal sinuses remain undiagnosed for a long time, as they occur without severe pain. Pain usually appears during the height of the disease.
Functions of the maxillary sinuses:
- Humidification of inhaled air.
- Participation in the formation of voice.
- Regulation of intracranial pressure.
- Lightening the weight of the skull bones.
- Air filtration and protection against pathogenic microorganisms.
X-ray: where to start
During the examination, the specialist will make a preliminary diagnosis of “sinusitis” and send you for an x-ray to clarify suspicions.
An x-ray is a collection of images of the anatomical structures of the body obtained by x-ray irradiation. An X-ray image, like any negative image, consists exclusively of black and white shades. This is due to the fact that each tissue in the human body has its own degree of absorption of gamma radiation. The more tissue absorbs, the brighter and more intense it is visible in the image.
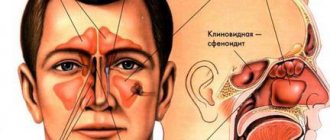
To diagnose certain diseases, it is extremely necessary to perform fluoroscopy in the optimally correct position, since only in this projection the areas required for inspection become visible. For example, there are several sinuses in the skull:
- frontal (frontal) sinus,
- wedge-shaped (main),
- maxillary (maxillary),
- lattice labyrinth.
In order for the nasal sinuses to be as visible as possible in the image, it is necessary to shoot in the following projections:
- axial – mainly used to assess the condition of the skull base, rocky part of the temporal bone and visualization of the main sinuses,
- lateral – important for examining the frontal, determining the size of the sphenoid and maxillary sinuses, the condition of the anterior parts of the facial bones and the base of the skull,
- nasofrontal – optimal for studying the frontal sinuses, cells of the ethmoidal labyrinth and orbits,
- The most clear way to trace the pneumatization of the maxillary sinus is to position the patient with the chin and nose resting on the X-ray machine stand (nasochin position).
For correct diagnosis, it is very important that the image has good contrast and sharpness and does not have any extraneous shadows or artifacts. All this together will make it much easier for the doctor to make the correct diagnosis.
To read: Suprax - an effective cephalosporin for sinusitis
As a rule, complete darkening of the maxillary sinuses indicates that a large amount of pus has accumulated inside them due to an extensive inflammatory process caused by harmful microorganisms.
What is called subtotal darkening of the maxillary sinuses?
Subtotal darkening of the maxillary sinuses is a radiological sign that indicates an inflammatory process in the organ. Darkening is also observed with the development of pathological changes in the mucous membrane.
Sometimes darkening may indicate the development of tumors in the sinus area. They can be either benign or malignant. The development of cysts is often detected using x-rays.
But most often, darkening on an x-ray indicates an accumulation of pus. Its detection indicates a disease such as sinusitis.
Inhomogeneous darkening of the lung without clear contours, what is it?
A previously healthy woman developed a dry cough after receiving an influenza vaccination. Due to the fact that the cough did not change during antibacterial therapy, the therapist prescribed a chest x-ray. What pathological changes are detected in the image, and with what diseases should a differential diagnosis be carried out in this case?
a) Original picture
. An area of darkening in the left lung.
b) Interpretation
. The radiograph reveals an area of darkening in the left pulmonary field, located near the border of the heart. This is a round formation with clear boundaries and a uniform structure. The location of the formation near the border of the heart suggests its localization in one of the lingular segments. Single, round lung lesions like this are called "coin-shaped lesions." Differential diagnosis is carried out between many diseases.
Most often, such a shadow is detected in primary lung cancer or a secondary form (metastasis) when the primary tumor is localized in another organ. Other possible conditions include benign tumors (such as hamartoma), a rheumatoid nodule, or an infectious lesion. If a “coin-shaped mass” is detected in the lungs, it is necessary to identify the presence of areas of calcification, since in this case the mass is most likely benign. It is also important to carefully consider the structure of the shadow itself.
The presence of an air bronchogram (i.e., lumens of the bronchi) makes one think about the infectious nature of the lesion, and the detection of an area of clearing against the background of a shadow suggests the formation of a cavity (cavity). In this case, neither clearing nor air bronchograms are detected against the background of the shadow.
Unfortunately, this patient had a single metastasis of adenocarcinoma in the lung. Upon detailed questioning, it was determined that she had been experiencing intestinal dysfunction for some time. The primary tumor was found in the colon.
Finally _
. The “coin-shaped formation” in the lung is caused by metastasis of adenocarcinoma of the colon.
Editor: Iskander Milevski. Publication date: 29.8.2021
Source
Possible causes and symptoms of blackouts in adults and children
The reasons for darkening can be very diverse.
As a rule, the following reasons are distinguished:
- Exposure to pathogenic microorganisms and the development of inflammation.
- Accumulation of pus.
- Inflammatory diseases of the paranasal sinuses.
- Sinus cysts.
- Tumors of the paranasal sinuses.
- Fluid accumulation.
Sinusitis
Subtotal darkening of the maxillary sinuses is observed with sinusitis. Sinusitis is an inflammation of the paranasal sinuses. It usually occurs against the background of long-term rhinitis or sinusitis. May have an acute or chronic course.
Symptoms of sinusitis:
- Prolonged nasal discharge, a characteristic feature of which is a change in color to greenish (purulent discharge). Possibly mixed with blood. The discharge is thick and does not drain well from the nasal cavity.
- Nasal congestion and change in sense of smell. The sense of smell decreases or disappears completely.
- Expanding headache. Localized in the frontal lobe of the skull.
- Bursting pain in the nasal sinuses, radiating to the upper jaw.
- Increased body temperature.
In children, sinusitis is more acute than in adults; a more severe fever is possible (increase in body temperature to 39-40°), intense pain in the head, and lacrimation. And also, a combination of sinusitis and otitis is often observed in young children. Inflammation of the middle ear occurs against the background of prolonged inflammation in the sinuses due to the anatomically short auditory tube in a child.
Sinusitis
Sinusitis is an inflammation of the mucous membrane of the paranasal sinuses. It can have an acute and chronic course.
The cause of sinusitis is bacterial and viral infection, incompletely treated rhinitis, and allergic reactions.
Most often, sinusitis occurs in children. This is due to the immaturity of the immune system and frequent viral diseases. In addition, sinusitis can occur in children under 1 year old, with improper rinsing of the nasal passages, as well as with excessive instillation of vasoconstrictor drops.
Sinusitis is most often acute.
You can suspect it if the following symptoms are present:
- Thick discharge from the nose, difficult to separate, yellow in color.
- Nasal congestion.
- Sore throat.
- Nasality in the voice.
- Increased body temperature.
- Headache.
Pain map for acute sinusitis
Sinusitis can be suspected if rhinitis does not go away after 7-10 days.
Frontit
Frontitis is an inflammation of the frontal sinuses. The cause of inflammation is acute viral infections, complications of sinusitis, sinusitis and rhinitis. Predisposing factors may also include a deviated nasal septum, the presence of adenoids and chronic foci of infection in the body.
Inflammation develops acutely. Body temperature rises above 38.5 degrees. A pronounced pain syndrome develops in the area of the brow ridges, which intensifies with pressure. There is also lacrimation, photophobia, eye pain, nasal congestion and purulent discharge from the nasal passages.
Frontal sinusitis is a serious disease that requires medical attention. With the development of this pathology, complications may develop in the form of brain damage (meningitis).
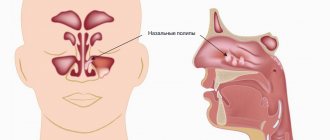
Cyst
A cyst is a round-shaped formation filled with exudate. Its detection is usually accidental, since its development is not accompanied by any pathognomonic symptoms.
Sometimes patients may complain of a foreign body sensation in the sinus area, pressure in the frontal region, fluid discharge from the nasal passages and a slight deterioration in nasal breathing.
Tumor
Tumors of the paranasal sinuses can be benign or malignant.
Malignant tumors are divided into the following types:
- Epitheliomas.
- Sarcomas.
Symptoms of tumors at the initial stage of development of the tumor process are invisible.
But as it progresses, the following clinical symptoms may appear:
- Pain in the sinus area.
- Headache.
- Enlargement of regional lymph nodes.
- Increased body temperature.
- Discharge from the nasal passages.
- Nasal congestion.
Benign tumors are also often localized in the maxillary sinuses. Their course may also be unnoticeable until the tumor reaches a large size. Typically, polyps or bone tumors that have grown from the bones of the skull into the sinus area are localized in the sinuses.
The symptoms are:
- Pain in the sinus area.
- Headache.
- Nasal congestion.
- Mucous discharge from the nose.
Inhomogeneous darkening of the lung without clear contours, what is it?
The amount of shadowing of the lungs
, as well as enlightenment, it is more expedient to express it in linear units - millimeters and centimeters.
Shadows in the pulmonary fields are divided into foci, foci or infiltrates, subtotal and total shadows. Processes
that are localized within a lobule of pulmonary parenchyma and cause shading of no more than 1 cm in diameter should be called focal shading.
Focal shadows
in turn, they are divided into large (from 0.5 to 1 cm), medium (from 0.3 to 0.5 cm) and small lesions (up to 0.3 cm in diameter).
Small focal shadows, especially of tuberculous origin, which are less than 2-3 mm in size, when they are not calcified and are usually not visible when examined on a screen, are determined only on high-quality radiographs. Small-focal dissemination during transillumination can be judged by an indirect sign: diffuse shading with poor visibility of the pulmonary pattern, as well as some ripples revealed when turning (A. E. Prozorov). Mid-focal shadows
are determined not only on photographs, but are also revealed by transillumination.
X-ray of the chest organs in an atypical projection (in the position of lordosis).
On the right, in the lower pulmonary field, in the medial and middle zones, a clearly defined, homogeneous shading is determined, having a triangular shape, with its base adjacent to the shadow of the heart. Right-sided interlobar pleurisy. Large focal shadow formations
Most of them are compactions of the lung tissue, often of the type of infiltrative-pneumonic reactions of both tuberculous and inflammatory origin, as well as of a tumor nature.
Shadows
, the dimensions of which are more than 1 cm in diameter, are called shading foci or infiltrates. These are the most frequently detected shadow formations in the pulmonary fields, which can be caused by very diverse patho-morphological changes both in the lung tissue itself and in organs and systems located in the chest cavity or associated with the chest wall.
Total shading
. In this case, the pulmonary field is darkened by an intense shadow throughout. Total shading is most often based on total atelectasis, total pleurisy, congenital underdevelopment of the lung, or a removed entire lung. Such shading is usually one-sided.
Subtotal shading
. As the name implies, with this type, the image will reveal shading covering at least 2/3 of the entire light lung field. The anatomical and morphological substrate of these shadow formations is most often inflammatory processes of the lung tissue: effusions in the pleural cavity, atelectasis, pneumosclerosis, widespread adhesive changes in the pleura, diaphragmatic hernia. Sometimes subtotal shading is two-sided.
Source
Is it necessary to take an x-ray?
If you suspect the development of a pathological process in the sinus cavity, radiography is necessary. Advanced pathology can lead to serious complications.
It is especially important to take an x-ray if the patient complains of a constant bursting headache, prolonged nasal discharge and increased body temperature.
Preparing and performing radiography
Radiography of the paranasal sinuses does not require special preparation. This diagnostic procedure is carried out in two positions: lying or standing. During the procedure, the patient presses his chin close to the device, then, at the command of the radiologist, holds his breath for 30 seconds. The procedure itself takes no more than 1-2 minutes.
In children, this procedure is practically not used. X-rays are performed in children strictly for urgent reasons.
How often can an x-ray be taken for sinusitis, when can it be repeated?
The standard for diagnosis and treatment of sinusitis requires two x-ray examinations: before and after therapy. In certain cases, a second study is carried out two weeks after the start of treatment.
Radiography involves the patient receiving a certain dose of radiation, so it is not recommended to carry it out frequently. The optimal number of examinations is three times a year.
If there is a need for several diagnostic procedures, it is better to replace them with ultrasound or magnetic resonance imaging of the sinuses. It is better to refuse repeated computed tomography because it is a high-tech type of x-ray examination.
Interpretation of the radiograph
The presence of exudate in the nasal sinuses indicates the presence of an acute inflammatory process, and thickening of the walls of the nasal sinuses and narrowing of their lumen may indicate chronic inflammation.
Subtotal darkening of the maxillary sinuses
A horizontal fluid level may indicate inflammatory diseases of the maxillary sinuses (sinusitis).
Subtotal darkening with an upper horizontal level in the area of the maxillary sinuses may indicate sinusitis.
If the darkening is localized in the frontal sinuses, then this indicates the development of frontal sinusitis.
To diagnose tumors, radiography with a contrast agent is performed. This helps to better see the location of the tumor and its size. When contrast is introduced, tumor formations “absorb” the pigment and become more visible.
Conclusion
The outstanding ancient physician Hippocrates taught: “Eliminate the cause and the disease will go away.” The use of radiography for the diagnosis of sinusitis fully meets this requirement.
- It is effective, accessible and simple.
- The method has established itself as the main one in the diagnosis of this disease.
- The study makes it possible to establish not only the presence of the disease, but also to evaluate the effectiveness of the treatment. For a more detailed examination, the doctor may also prescribe a CT scan of the maxillary sinuses.
- Reading the image is easy.
- X-rays can be repeated throughout the year.
Other diagnostic methods
If you suspect the presence of a pathological process in the paranasal sinuses, it is necessary to conduct a number of additional studies:
- Clinical blood test. It is carried out to assess the general condition of the body, and in the transcript of the analysis you can see whether there is an inflammatory process in the body.
- CT scan of the sinuses. It is carried out when the X-ray image is unclear, as well as when a malignant process is suspected.
- MRI. Helps evaluate not only the condition of bone structures, but also nerves, blood vessels and soft tissues.
MRI shows fluid around the lung, what should I do?
If an MRI shows fluid around the lung, it may be a pleural effusion. More often, pathology develops in the following cases:
Less commonly, excess fluid around the lung is associated with tumors (central, peripheral cancer, metastases from other organs to the pleura and lymph nodes), and systemic connective tissue diseases. With ascites, sweating through the diaphragm is possible. Damage to blood vessels during trauma leads to accumulation of blood or lymph in the pleural cavity.
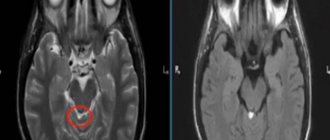
Pleural empyema (accumulation of pus) on the left on MR images of the lungs in the axial projection: a – T1-weighted image; b – T2-weighted image
When an MRI detects fluid around or near the lung, the next diagnostic step is a puncture. The procedure is performed under local anesthesia. A thin needle is inserted into the chest and fluid is withdrawn for laboratory analysis. Treatment tactics are developed depending on the results.
MRI for tuberculosis MRI of the chest prices in St. Petersburg MRI after stenting of cardiac vessels MRI of the chest organs in St. Petersburg MRI of the sternum prices in St. Petersburg
Source
Treatment for incomplete darkening of the maxillary sinuses
Treatment of inflammation of the sinuses is complex and includes symptomatic therapy, anti-inflammatory and antibacterial drugs.
For the treatment of children, antibacterial drugs are prescribed with caution. The most preferred antibiotics for treatment in childhood are penicillins and cephalosporins.
Vasoconstrictor drugs based on xylometazoline (Nazivin) are prescribed with caution in childhood . Such drugs should not be used in a child for longer than 5 days. You should also strictly adhere to the dosage.
Medicines
| Group of drugs | Name | Dosage, route of administration, course of treatment |
| Antibiotics | Amoxiclav or Cefepime | Intramuscularly or orally 2 times a day for 10-14 days. |
| Antimicrobial nasal drops | Protargol | 1-2 drops in each nasal passage, no more than 7 days. |
| Vasoconstrictor sprays or nasal drops | Tizin, Nazivin | 1 spray into each nasal passage. No more than 7 days. |
| Herbal anti-inflammatory drops for oral administration | Sinupret (for children UmkaLor) | The dosage is calculated based on the patient's age. The course of treatment is from 2 to 3 weeks. |
| Antihistamines | Citrine | 1 tablet 1 time per day. The course of treatment is 14 days. |
| Hypertonic solutions | Aquamaris, Aqualor | In the form of a spray for adults, in the form of drops for children. Washing is carried out 4-5 times a day. |
| Antipyretic drugs (at temperatures above 38.5) | Ibuprofen, paracetamol | In age dosage, but not more than 6 tablets per day |
Surgery
Subtotal darkening of the maxillary sinuses in many cases responds quite effectively to conservative therapy, but if there is no effect, surgical intervention may be required.
For sinusitis, it may be necessary to “puncture” the maxillary sinus. This manipulation is necessary to remove accumulated pus from the sinus.
To do this, the otolaryngologist performs a puncture in the projection of the maxillary sinus with a special instrument. After which the purulent contents are drained. The doctor then rinses the sinuses with an antiseptic solution to prevent further inflammation.
The operation takes about 30 minutes. and does not require putting the patient under anesthesia. If cysts and neoplasms were identified during the examination of the sinuses, then in this case they are removed surgically under general anesthesia.
If a tumor is found, in addition to removing it, a biopsy is performed to find out the type of tumor. After receiving the results, the doctor chooses the further method of treatment.
Nasal drops
Without their use, the treatment of the disease in question is not complete.
Therefore, now it’s worth talking about which nasal drops for sinusitis are the most effective. During an exacerbation, drugs such as Nazivin, Xymelin, Galazolin and Naphthyzin help cope with unpleasant symptoms.
To provide a local effect on the bacterial flora, Polydex and Isofra sprays are used.
Homeopathic remedies “Sinupret” and “Euphorbium Compositum” are very helpful in liquefying and subsequently removing viscous mucus.
In especially severe cases, the use of hormonal drugs is indicated. The most effective nasal drops for sinusitis from this group are Avamis and Nasonex, available in the form of nasal suspensions.
Folk remedies
Subtotal darkening of the maxillary sinuses can be treated using traditional methods. Medicines based on medicinal plants are also used in the treatment of inflammatory diseases of the upper respiratory tract. For this purpose, saline solutions, drops, and compresses are used.
The only contraindication is an allergic reaction to the components of the drug.
For young children under 1 year of age, traditional treatment methods should be used with caution so as not to provoke the development of an allergic reaction.
Mustard oil
Rhinitis and sinusitis can be treated with mustard oil. To do this, the oil must be slightly heated, but the temperature must be comfortable so that when the oil is instilled into the nose, the mucous membrane does not burn.
Place 3-4 drops of oil into each nasal passage 2 times a day. The oil has anti-inflammatory and antiviral effects, and also reduces swelling of the nasal mucosa.
Garlic
Garlic has antibacterial properties and can be used to make drops for the common cold. To do this, you need to take 2 cloves of garlic, pass through a press, place in gauze (folded in several layers) and squeeze out the resulting juice.
Then add 3-4 tbsp to the garlic juice. l. water or 2 tbsp. l. olive oil. This must be done so that garlic juice does not lead to a burn of the mucous membrane.
For the first use, 1 drop is instilled into each nasal passage. If no allergic reaction subsequently occurs, then you can instill 2-3 drops into each nasal passage for 7 days.
Such drops are prohibited for use by children. Since the mucous membrane in children has a more immature structure compared to adults. Instillation of such drops may cause burns.
In addition to drops, garlic can be used as an air disinfectant. To do this, the garlic is first peeled and cut into small pieces. Garlic is laid out on plates and placed at different ends of the room. Since garlic is a natural antiseptic, its action will deactivate viruses and bacteria that are released by a sick person.
Propolis solution
To treat sinusitis, use a propolis solution. To do this, take a 10% alcohol solution of propolis. Before use, dilute a small amount with water so as not to irritate the mucous membrane. You need to instill 1-2 drops into each nasal passage for 7 days.
Due to the alcohol content, this method of treatment is contraindicated for children.
Aloe juice
Aloe is used not only to treat inflammatory diseases, but also to prevent viral infections.
For this purpose, drops can be prepared from aloe juice. To do this, take aloe juice and mix it with water in a 3:1 ratio. If such drops are indicated for a small child, then the proportion is 5:1. You need to instill 2-3 drops into each nasal passage for 10 days.
Black radish
Any compresses are prohibited in the phase of acute inflammation, as well as at elevated body temperature. A black radish compress is effective in reducing swelling of the mucous membrane.
To prepare such a compress, you need to take one radish, peel it and grate it. Then you need to mix with vegetable oil and heat slightly. Apply the prepared pulp to the sinus area for 10 minutes. You can use thin cloth or gauze for this purpose. The course of treatment with this remedy is no more than 7 days.
Sea salt
A hypertonic sea salt solution can be purchased at a pharmacy, or you can prepare it yourself at home.
For this purpose, you need to take ½ teaspoon of sea salt and dissolve its contents in a glass of warm water. Then you need to draw the required amount of solution into a sterile syringe and rinse each nasal passage one by one. It is recommended to rinse your nose with saline solution up to 5 times a day.
Children need to rinse their nasal passages by instillation. Until the age of 3, the nasal passages should not be washed with sprays or a syringe. Since a strong stream of solution can promote the advancement of microorganisms to the auditory tube. Since the auditory tube in children is short, this can cause otitis media.
If a subtotal darkening is observed on the x-ray of the maxillary sinuses, this means that a pathological process has begun in them. In some cases, a number of additional diagnostic procedures may be required to clarify the diagnosis.