An odontoparodontogram is a diagram - a drawing containing information about each dental unit. The drawing is intended to form a holistic picture of the current state of the dentofacial apparatus and identify various pathologies.
The technique was first put forward in 1953 by scientist and dentist V.Yu Kurdlyansky. The professor was of the opinion that in the normal condition of the teeth, only half of the tissues are used for full functioning, while the rest is in reserve.
The periodontium normally withstands a certain load until the threshold of pain sensitivity is overcome. These indicators form the basis of Kurdlyansky’s scheme.
Legend
Simplicity of graphical registration is ensured by the use of symbols. The periodontogram is compiled on the basis of data obtained after radiography and laboratory tests. Schematic designation of the graph:
- N – no pathologies detected;
- O – no bone formation;
- ¼ – 1 degree of atrophy;
- ½ – stage 2 defect;
- ¾ – 3rd stage.
In the second and third degrees of atrophy, a tooth located in soft tissues must be removed.
The value of periodontal endurance is conventionally designated by a coefficient - the ratio of load and pressure per unit.
With increasing atrophy and increased mobility of dental elements, the coefficient of resistance to stress decreases. The values of reserve tooth tissues vary depending on the degree of periodontal damage.
Odontoperiodontogram data
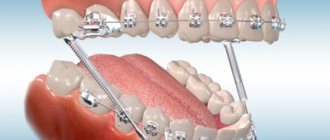
The method is based on the fact that the periodontium has a certain endurance, which decreases when it is destroyed. Previously, a gnathodynamometer was used to determine endurance. With its help, pressure was applied to the tooth until painful sensations appeared. In modern periodontology, computer examination is used to obtain accurate data. To simplify calculations in the ondontoparodontogram according to Kurlyandsky, coefficients defined for each tooth are used.
Data obtained during a clinical examination of the depth of the periodontal pocket and periodontal endurance are entered into the odontoperiodontogram table according to Kurlyandsky. Based on these data, the coefficient is calculated and the reserve and degree of functional deficiency of the tooth are identified.
Requirements for filling
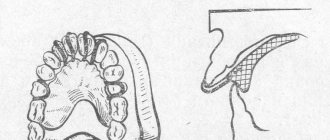
Kurdlyansky's drawing is designed in the form of a table of cells with five parallel rows. The central row indicates the numbering of the teeth. The second line from the top displays the condition of the HF periodontium. The top line contains information about the HF reference apparatus.
The bottom lines containing data on the structure of the periodontium and elements of the LF are filled in identically. Information is entered into the table sequentially, starting from the lower jaw (right - left) and moving to the upper jaw (left - right).
After entering information about each tooth, the jaw indicators are summed up. Having received the total data, the value of the power ratios of the dentition below and above is determined.
Using the force ratio coefficient, the specialist identifies dominant groups of units and weak areas.
Based on the information in the drawing, the need to equalize the power relationship of the dentition or individual groups through orthopedic treatment is determined.
Evaluation Features
To simplify the graphical recording of information, all data has symbols. A periodontogram is compiled during X-ray diagnostics and laboratory and clinical procedures. Schematic labeling of the graph:
- N – without pathologies;
- O – no bone formation;
- ¼ – 1 (initial) degree of atrophy;
- ½ – stage 2 pathology;
- ¾ – 3rd stage.
At the fourth degree of atrophy (or III, tending to IV), the tooth located in the soft tissues must be removed.
The endurance of dental periodontium is conventionally designated by a coefficient representing the ratio of load and pressure on the teeth.
With the increasing stage of atrophy and increasing tooth mobility, the coefficient of resistance to all kinds of stress decreases, in particular during eating. The reserve tissues present in each tooth change their indicators in accordance with the degree of periodontal damage.
Practical meaning
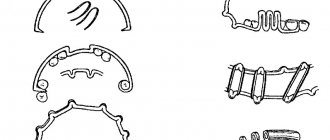
The scheme is used when selecting an individual orthopedic device. Prosthetic products come in various types: removable, fixed, bridge-like. The dentist selects the appropriate model depending on the condition of the units and the patient’s wishes.
A periodontogram is necessary to calculate individual elements requiring prosthetics. The endurance indicator of the tissues of the supporting dental apparatus affects the possibility of choosing a specific model.
For bridge prosthetics, the sum of the coefficients is equal (in units):
- 4.75 and above (chewing teeth);
- 3.5 (front group on LF);
- 3-3.5 (HF incisors).
Kurdlyansky's scheme demonstrates effectiveness in:
- determining the optimal length of the splinting structure;
- installation of the optimal number of support units for bridge prosthetics;
- determining the number of clasps for a removable model;
- selection of locking fixation for the structure.
Table of odontoperiodontogram according to Kurlyandsky: diagram, features and important nuances
This scheme was first introduced into dental practice by Dr. Kurlyandsky in 1953. According to the specialist, in a normal state, the periodontium uses half of its resource, and another 50% of the reserve allows it to withstand loads. Currently, odontoparodontogram is also in great demand among dentists. Based on the research, a table is compiled that contains data on periodontal endurance - the limit when a tooth can withstand pressure without accompanying pain. To make it more comfortable for the dentist to work, separate coefficients have been introduced for each dental unit.
The odontoperiodontogram table according to Kurlyandsky is compiled on the basis of the following types of information:
- laboratory research;
- radiography;
- functional testing;
- clinical periodontal studies
In total, the graph consists of five lines. The specialist makes records gradually, starting with the first tooth in the lower jaw and ending with the left one in this row. The upper jaw is examined according to the same principle - starting with the outer left tooth (wisdom), and ending with the right outer wisdom tooth.
The first row contains information about the condition of the periodontium of the upper jaw, and the second row contains data about the soft tissues of the upper jaw. The third line contains a formula with graphic designations of each tooth in Arabic numerals.
The drawing shows the following symbols:
- Sign O – missing tooth;
- Sign N – normal dental unit;
- More than ¾ - degree IV tissue atrophy;
- ¾ — tissue atrophy of the third degree is observed;
- ½ - second level atrophy;
- ¼ - atrophic processes of the first degree.
After the dentist has filled out the table, you can determine the exact number of healthy supporting teeth that are important for further jaw prosthetics. After summing up the periodontal endurance coefficients of supporting dental units, the dentist will be able to accurately select a prosthesis in this particular case.
The gradation of the sum of the coefficients looks like this:
- for the anterior teeth of the upper jaw - more than 3 units;
- for the front teeth of the lower jaw - at least 3.5 units;
- for chewing units of the lower jaw - more than 4.75 units.
Thus, an odontoperiodontogram is performed to compare the functionality of the teeth of the lower jaw with the resources of the teeth of the upper jaw. But based on the data obtained, it is possible to select an ideally suitable prosthesis design - a classic “bridge” or a removable one.
The scheme is also relevant if the patient suffers from periodontal disease, and this problem can interfere with the normal functioning of the prosthesis. Based on the odontoparodontogram data, the dentist determines the length of the splinting structure and the exact number of supporting teeth. The data is transmitted to a dental laboratory, where a specialist produces a product for this specific request.
It is important! An odontoparodontogram allows you to determine the exact number of clasps for a removable structure, as well as select any other clasp for the prosthetic structure.
How is the table filled out?
Data about each tooth and supporting part are entered into the diagram. This information is derived from:
- X-rays of the jaw and teeth;
- visual examination of the patient;
- laboratory and clinical tests;
- patient's medical history.
The data allows you to identify:
- type of prosthetics;
- length and features of the splinting system;
- if the study is not performed for the first time, its results help determine the dynamics of treatment.
The accuracy of determining the prosthetic method and the success of treatment depend on how accurately and correctly the diagram is filled out.
The table consists of the following main rows:
- N – means that no pathologies were found in this area;
- O – means that there is no bone formation in this area;
- more than ¾ - pathology of the highest degree (fourth);
- ¼ — tissue depletion of the 1st degree;
- ½ — atrophic changes of the 2nd degree;
- ¾ - pathology of the third degree out of four possible.
After filling out the schematic drawing, the specialist summarizes the results that characterize the condition of the lower and upper jaws, determining the power potential of the dentition.
Only a professional dentist with extensive experience in this field can correctly compile and decipher an odonto-periodontogram. The 100 Teeth network of clinics employs specialists who daily compile odonto-periodontogram tables and, based on them, recommend treatment to patients.
By filling out the table, a specialist can determine the exact number of supporting structures needed to install a bridge system.
Examples of coefficient sums for installing a bridge on a patient:
- at least 3 units. – for the frontal group of teeth in the upper jaw;
- not less than 3.5 units. – for the frontal teeth of the lower jaw;
- not less than 4.8 units. – for chewing, in the lower and upper jaws.
Features of gnathodynamometry
As part of the odontoparodontogram, gnathodynamometry is performed - determining the strength of the masticatory muscles, the level of endurance of the supporting teeth when clenching the jaws using a special apparatus. These indicators are tested on a gnathodynamometer. At the moment the jaws are clenched, an indicator is recorded, which normally in an adult ranges from 15 to 35 kg in the area of the front teeth and from 45 to 75 kg in the area of the distant, chewing teeth. The level of endurance may vary, especially with gum disease (periodontal disease, periodontitis), or the absence of one or a number of teeth.
The main purpose of a properly performed odontoperiodontogram is to help the specialist make a thorough comparison of the functions of the teeth and gums of the lower jaw with the potential of the dental groups of the upper jaw. Based on the diagram data, it is possible to determine the optimal prosthesis design for a particular patient, the splinting system, and the number of supporting teeth.
Periodontal endurance coefficient (according to V. Yu. Kurlyandsky)
⇐ PreviousPage 10 of 41Next ⇒
To compile a periodontogram, it is necessary to obtain data on the condition of the bone tissue of the tooth sockets and the degree of its atrophy. The degree of atrophy of the sockets is shown by x-ray and clinical studies. Since atrophy of the tooth socket occurs unevenly, the degree of its destruction is determined by the area of greatest severity. In the clinic, this occurs by probing the pathological pocket with a conventional probe, the end of which is blunted or has a soldered metal ball to prevent damage to the mucous membrane of the gingival pocket. X-rays show atrophy of the sockets near each tooth.
There are four degrees of atrophy. With I degree, atrophy of the socket is observed by 1/4 of its length, with II - by 1/2, with III - by 3/4, with IV - complete atrophy of the socket (Table 30).
Table 25.
Periodontogram
In the above completed periodontogram, the dental formula is written horizontally in the middle column. The columns located above and below the dental formula indicate the degree of atrophy of the sockets of the corresponding teeth. The letter N means that no atrophy of the socket has been detected, the number 0 means the absence of a tooth or grade IV atrophy. The following columns include the corresponding endurance coefficients of the supporting apparatus of each tooth. On the right, these data are summarized. On the upper jaw, the periodontal endurance of the remaining teeth is 25.3 units, on the lower jaw - 17.7 units. Accordingly, the upper jaw has a more preserved periodontium. At the top and bottom of the table there are three more columns, which indicate the periodontal endurance of equally functioning groups of teeth. Thus, the periodontal endurance of the chewing teeth of the upper jaw is 9.3 units on the left, and 8.5 units of the lower teeth of the same name. The relationships in the anterior group of teeth are somewhat different: in the upper jaw, the total periodontal endurance is 6.7 units, and in the lower jaw - 4.5 units. This happened as a result of atrophy of the alveolar process and loss of some teeth.
According to the author, a periodontogram not only displays a detailed picture of periodontal damage, but also makes it possible to outline a prosthetic plan and prevent further destruction of the dentofacial apparatus. However, many clinicians in our country rightly objected to this interpretation of the role of the periodontogram (A.I. Betelman, E.I. Gavrilov, I.S. Rubinov). Their arguments basically boiled down to the following:
1. Periodontal endurance coefficients are derived from Haber data obtained more than 50 years ago. As is known, this method takes into account the endurance of the periodontium only to vertical load, which is not at all sufficient to characterize the shock-absorbing ability of the periodontium. Haber's data also raises doubts, since they endow the supporting apparatus of the teeth with very high total endurance (1408 kg).
2. Periodontal endurance coefficients, like any biological characteristics, have significant variability. They cannot be characterized by indirect quantities obtained through a small number of measurements. Thus, the initial data that served as the basis for calculating the periodontal endurance coefficient when compiling a periodontogram are incorrect. It is also erroneous that the decrease in periodontal endurance is directly proportional to the amount of socket atrophy. One of the characteristics of the tooth’s participation in the perception of chewing pressure is the size of the root surface and the width of the periodontal fissure. Tests (V.A. Naumov) have proven that the cervical third of the root has the largest area, and the apical third has the smallest area. An exception to this rule is the molars, the largest surface of which is the middle third, followed by the cervical, and then the apical. Thus, the ability of the periodontium to perceive chewing pressure at different levels of the root is not the same. It should also be taken into account that as the alveolar process atrophies, the outer part of the tooth is exposed, which further increases the load on the remaining part of the alveolus. All of the indicated disadvantages of the periodontogram do not give reason to consider it a sufficiently accurate method that could replace a thorough clinical examination of the patient.
Static methods turned out to be unsuitable for determining the degree of impairment of chewing efficiency, not only because they do not accurately determine the role of each tooth in chewing and the perception of chewing pressure, but also for the reason that they do not take into account the type of bite, the intensity of chewing, the strength of chewing pressure, and the influence of saliva and the role of the tongue in the mechanism of bolus formation. Therefore, to take into account the influence of all the above factors, functional (chewing) tests were proposed, which make it possible to obtain a more accurate idea of the dysfunction of chewing.
The first functional test was developed by Christiansen. He proposed to determine chewing efficiency by examining the degree of crushing of food of the appropriate consistency and appropriate mass. The subject was given 5 g of hazelnut or coconut to chew. After 50 chewing movements, the food mass was dried and sifted through a sieve to determine the degree of crushing. Chewability was calculated by the residual weight on the sieve.
S.E. Gelman developed and simplified the chewing test technique. Instead of hazelnuts, he took almonds weighing 5 g and asked the patient to chew for 50 seconds. There are certain requirements for a product that can be used for chewing testing. The parts formed after chewing should not dissolve in saliva, shrink in volume after drying on a water dome and stick together. Almonds largely meet these requirements.
Functional chewing test technique
For mass research, it is advisable to have pre-prepared portions. The patient sits down at the table, a kidney-shaped tray and a glass of boiled water at room temperature are placed in front of him. He is asked to take the entire portion (5 g) of almonds into his mouth and begin chewing only after the command: “Begin!” Having heard the command, the subject evenly chews the almonds using his usual method. The beginning of chewing is noted on a stopwatch. After 50 seconds, the command is given: “Stop!”, after which the entire mass is spat out into the tray. Then they ask you to rinse your mouth several times and spit water into the tray. If chewing took place with removable dentures, then they are removed from the mouth and rinsed with water over the same tray.
It is very important that during the test there is no one in the laboratory except the laboratory assistant and the patient. It is necessary to briefly explain the essence of the test and its duration. To rinse, you need to take boiled water. It is imperative to disinfect the sample spit into the vessel by adding 5-10 drops of a 5% solution of sublimate to it.
The resulting sample is processed as follows. The mass is filtered through cheesecloth over an empty, clean vessel. After the liquid has drained, the gauze with the sediment is unrolled over a flat bath. Drying of the chewed mass is carried out in a water bath, since hot air in a dry-heat oven causes a change in the shape of the particles and their wrinkling.
The mass is considered dried if, when kneading between your fingers, it feels dry and crumbles easily. During drying, it is necessary to ensure that the water in the water bath does not boil away, as this can lead to overdrying of the sample. Then the mass is sifted through a metal sieve with holes with a diameter of 2.4 mm. Part of the mass remaining on the sieve is carefully poured onto a clean piece of glass and weighed to the nearest 0.01 g.
Example. The residue on the sieve is 0.5 g, which corresponds to some loss of chewing efficiency (x). The amount of loss of chewing efficiency is determined by solving a simple equation:
Conclusion: Loss of chewing efficiency - 10%.
Further development of the functional chewing test was carried out by I. S. Rubinov. He believed that chewing 5 g of almonds poses challenges to the masticatory apparatus that go beyond the norm. Therefore, he suggested that the patient chew 0.8 g of hazelnut, which is approximately equal to the mass of one almond. The test is carried out as follows. The subject is given 0.8 g of hazelnut and is asked to chew it until the swallowing reflex appears. As soon as the subject has a desire to swallow the chewed nut, he is asked to spit the contents of the oral cavity into a kidney-shaped tray. Further processing is carried out as with S.E. Gelman’s test. The time of chewing the nut is counted using a stopwatch. As a result of the functional test, two indicators are obtained: the percentage of food chewing (chewing ability) and chewing time.
Studies have shown that with an orthognathic bite and intact dentition, the nut kernel is completely chewed in 14 seconds. As teeth are lost, chewing time increases and the residue on the sieve also increases.
When analyzing the test result, you should always take into account the chewing time and the percentage of chewed food. Evaluating against just one indicator can lead to erroneous conclusions. For example, during a chewing test carried out in patients with complete loss of teeth immediately after the application of dentures, the mass turns out to be chewed by 80%. It would seem that with the help of prosthetics it is possible to almost completely compensate for the loss of teeth, but if you measure the chewing time, it will turn out to be 2-3 times longer than normal.
⇐ Previous10Next ⇒
Recommended pages:
Use the site search: