Find out more about nervous diseases starting with the letter “N”: Sleep disturbance; Narcolepsy; Hereditary cerebellar ataxia of Pierre-Marie; Spinal circulatory disorders; Trigeminal neuralgia; Neuralgia of the submandibular and sublingual nodes; Neuralgia of the glossopharyngeal node; Neuralgia of the ear ganglion; Neurasthenia; Neural amyotrophy of Charcot-Marie-Tooth; Acoustic neuroma; Neuroma; Optic neuritis; Pharyngeal neuritis; Neuritis of the facial nerve; Neuritis; Obsessive-compulsive neurosis; Pharyngeal neurosis; Neuroses; Neurosis-like stuttering; Femoral nerve neuropathy.
What is glossopharyngeal neuralgia?
If the cranial nerve is affected by a quarter on one side, and paroxysms of pain appear in the tonsils, soft palate, pharynx and ear, then the patient may have neuralgia of the glossopharyngeal nerve. With this pathology, a violation of the taste perception of the posterior third of the tongue, on the affected side, is detected. Hypersalivation and decreased reflex of the palate and pharynx are also noted. To make a diagnosis, an examination by a neurologist or dentist is required. CT and MRI of the brain are indicated as hardware diagnostic methods. In most cases, treatment is conservative, including:
- Anticonvulsants;
- Analgesics;
- Sleeping pills and sedatives;
- Vitamin therapy;
- Physiotherapy;
- General strengthening procedures.
2. Reasons
The most common causes of glossopharyngeal neuralgia known today are trauma, acute respiratory infections and chronic infectious and inflammatory foci (for example, in the tonsils), inflammation of the meninges (meningitis, arachnoiditis), poisoning (in particular, lead compounds), oncological processes, vascular pathology (aneurysms, thrombosis), endocrine disorders.
In some cases, the cause remains unclear (idiopathic neuralgia).
Visit our Neurology page
Structure of the glossopharyngeal nerve
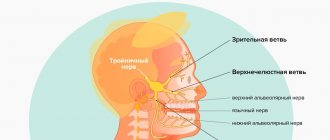
N. glossopharyngeus or glossopharyngeus nerve begins in the nuclei of the medulla oblongata. It is based on motor, sensory and autonomic parasympathetic fibers. Moreover, the sensory fibers begin in the sensory nucleus common to the vagus and glossopharyngeal nerves. They innervate the mucous membrane of the pharynx, soft palate, tongue, tonsils, and Eustachian tube. The sensation of taste in the anterior two-thirds of the tongue is provided by taste fibers emerging from the nucleus of the tractus solitarius. The taste fibers of the glossopharyngeal nerve are responsible for the taste sensations of the posterior third of the tongue and epiglottis.
The motor fibers originate in the nucleus ambiguus and innervate the stylopharyngeal muscle, which is necessary for raising the pharynx. Together with the vagus nerve, they form the reflex arcs of the pharyngeal and palatal reflexes.
Parasympathetic fibers originate in the salivary nucleus. Being part of the tympanic and lesser petrosal nuclei, they reach the autonomic ganglion, and with the branch of the trigeminal nerve they regulate salivation of the parotid gland.
Since the pathways and nuclei of the glossopharyngeal and vagus nerves are common, isolated pathology n. Glossopharyngeus. But more often symptoms of combined lesions are observed.
Causes of lingual nerve damage
The etiology of this phenomenon lies in the peculiarities of the topographic location of the lingual nerve and its adjacency to the surgical area, as well as the sensitivity of the nervous tissue to ischemia. Post-traumatic neuropathy of the lingual nerve, after complex extractions of impacted and dystopic third molars of the mandible, accompanied by complications, occurs in 2-7% of clinical cases [5].
A damaged lingual nerve is often caused by the following factors:
- Failure to observe anatomical landmarks by a doctor.
- Direct injury to the nerve with a needle at the time of partial or complete anesthesia, provided that it has low mobility in the tissues and is adjacent to bone structures.
- Injury from a deformed needle point.
- Neurotoxic effects of the anesthetic and hematoma: injury to the lingual nerve can occur during anesthesia due to the formation of a hematoma, as well as the chemical action of the components of the anesthetic solution.
- Endoneural administration of anesthetic [2].
Pathogenesis
There are cases of idiopathic Sicard syndrome. At the same time, it is almost impossible to establish the etiology of the disease. Provoking factors may be:
- Acute or chronic intoxication;
- Otitis;
- Pharyngitis;
- Tonsillitis;
- Sinusitis;
- Atherosclerosis;
- Viral infections incl. flu.
Secondary neuralgia occurs due to:
- Arachnoiditis, encephalitis and other infectious lesions of the posterior cranial fossa.
- TBI.
- Hyperthyroidism.
- Diabetes mellitus.
- Meningiomas, gliomas, medulloblastomas and other intracerebral tumors of the cerebellopontine ganglion.
- Compression and irritation of any part of the glossopharyngeal nerve.
- Nasopharyngeal tumors.
- Intracerebral hematomas;
- Carotid artery aneurysm;
- Hypertrophy of the styloid process.
- Overgrowth of osteophytes of the jugular foramen.
- Ossification of the styloid ligament.
In some cases, pathology may be the first symptom of cancer of the larynx or pharynx.
4.Treatment
Treatment for glossopharyngeal neuralgia is aimed primarily at relieving pain. Given its severity and specificity, in some cases it is necessary to prescribe both non-narcotic and narcotic analgesics; Antiparoxysmal and anti-inflammatory drugs, vitamin complexes, restorative therapy, and electrophysiotherapeutic methods are also used. In situations where the established cause of neuralgia is mechanical compression (compression) of the nerve, for example, with hyperplasia of structures adjacent to the nerve, neurosurgical intervention is performed.
Conservative treatment usually lasts quite a long time (up to several years), but in most cases it leads to the elimination or significant reduction of neuralgia.
Symptomatic picture
Clinical signs include painful paroxysms lasting from a few seconds to three minutes. A sharp acute pain originates at the root of the tongue and instantly spreads to the tonsils, soft palate, ear and pharynx. May radiate to the eye, neck and lower jaw. Pain can be triggered by coughing, chewing food, its temperature, yawning, swallowing and even talking. During paroxysm, dry mouth is noted, immediately after hypersalivation. But dryness is not a mandatory sign of diagnosis, because the secretory insufficiency of the parotid gland can be compensated by the remaining salivary glands.
Paresis of the levator pharyngeal muscle does not cause swallowing disorders. But difficulties in chewing and swallowing associated with impaired proprioceptive sensitivity, which is responsible for the position of the tongue, may be noted by patients.
The disease has a wave-like course, worsening in autumn and winter.
Sore throat: possible causes, diagnosis and treatment
Sore throat is a common complaint of patients when visiting an otolaryngologist, therapist, pediatrician and general practitioner. The causes of sore throat can be infectious and inflammatory diseases of bacterial and viral etiology, inflammatory processes in the pharynx, larynx and surrounding organs caused by non-infectious factors, and non-infectious pathology (
). Before proceeding with pharyngoscopy, it is necessary to carefully detail the patient’s complaints and collect an anamnesis. The patient can call a sore throat the unpleasant sensations of scratching, burning, soreness, rawness, the feeling of a “foreign body,” the intensity of which is conveniently assessed on a 10-point scale, where the maximum manifestation of pain is rated at 10 points, the minimum at 1 point.
It is important to determine what, in the patient’s opinion, preceded the onset of pain and what other symptoms it is accompanied by. If there is hyperthermia, then the inflammatory nature of the disease is most likely: pharyngitis, tonsillitis (tonsillitis) [16]. Refusal of food and water can provoke severe pain in aphthous stomatitis (Fig. 2), tonsillitis of the lingual tonsil, paratonsillar and retropharyngeal abscess, Ludwig's angina (phlegmon of the floor of the mouth). With these diseases, drooling is possible, and inflammation of the paramygdaloid tissue and tissues of the floor of the mouth leads to trismus of the masticatory muscles (inability to open the mouth), a forced position of the head tilted to the painful side.
The occurrence of such a condition requires immediate contact with a medical specialist to sanitize the area of inflammation. Epiglottitis, an inflammation of the epiglottis caused by Haemophilus influenzae (more common in young children), gives similar symptoms. Along with refusal to eat, salivation, pain and hyperthermic symptoms, epiglottitis is accompanied by voice disturbance (it becomes dull, hoarse) and difficulty breathing. There is a forced position of the patient in a sniffing position, as if holding porridge in the mouth, the mouth opens freely, but a rough examination of the pharynx with a spatula can lead to laryngospasm and death. Therefore, with the above symptoms, pharyngoscopy is performed carefully; during it, you can see a hyperemic, edematous epiglottis behind the root of the tongue.
Other causes of sore throat accompanied by sore throat and cough can be in children and young people: drainage of discharge from the nasopharynx due to adenoiditis or sinusitis; irritation of the respiratory tract by dry air, smoke, including active and passive smoking; childhood infectious diseases [9]. In adults, a common cause of such complaints, often with a feeling of a lump in the throat, a “foreign body,” is an exacerbation of chronic pharyngitis associated with pathology of the gastrointestinal tract: gastritis, esophagitis, gastroesophageal reflux, cholecystitis, gastric ulcer. Severe dysphagia, regurgitation and pain when swallowing can be caused by esophageal varices [14].
A carefully collected anamnesis allows us to find out the dynamics of complaints, the time of their appearance, the connection with a previous injury or medical examination (gastroscopy), foreign body entry, contact with an infectious patient, hypothermia (drinking cold beer, ice cream), occupational or household hazards (irritants, dust , hot air, taking concentrated solutions of vinegar, spices, medications: corticosteroids, antibiotics, diuretics, local decongestants and others). Sore throat can occur as a manifestation of sexually transmitted diseases: gonococcal pharyngitis, syphilis, chlamydia of the respiratory tract. Infection with the human immunodeficiency virus contributes to the formation of inflammatory viral, tumor and mycotic lesions of the mucous membranes [3].
Chronic pathology of the kidneys, endocrine system, blood, previous radiation and chemotherapy can lead to the formation of a chronic inflammatory and atrophic process in the pharynx. The first manifestation of hyperglycemia [5] may be thirst and dry mouth, accompanied by catarrhal changes in the pharynx. Similar complaints occur with Itsenko–Cushing syndrome [5]. In patients with hypothyroidism, swallowing is often impaired, speech becomes slurred due to swelling and dryness of the tongue and lips, and it is difficult to perform pharyngoscopy.
Non-infectious pathology of the organs of the neck and chest cavity - angina pectoris, myocardial infarction - can manifest itself as intense pain in the pharynx and behind the sternum. Long-lasting dysphagia and unpleasant sensations in the form of a lump or foreign body in the throat, which are not amenable to anti-inflammatory therapy, can cause [14] tumors of the larynx, laryngopharynx, thyroid gland, and pharyngoesophageal (Zencker) diverticula. Many days of fasting, dieting, dyspepsia and heavy menstruation lead to a deficiency of vitamins and minerals. Vitamin A deficiency [5] causes dryness and erosion of the mucous membranes.
Vitamin B2 deficiency produces a triad of symptoms: dermatitis, cheilitis and glossitis (bright red, smooth and shiny dry tongue), accompanied by burning and pain in the mouth when talking and eating. Vitamin C hypovitaminosis occurs with dietary deficiency of ascorbic acid, inflammatory processes in the intestines and is manifested by pain, hemorrhagic and ulcerative-necrotic manifestations in the oral cavity and in the area of the palatine tonsils, mobility and tooth loss. Similar changes in the oral cavity and pharynx give rise to blood diseases (leukemia). Against the background of iron loss (with hyperpolymenorrhea), Plammer-Vinson syndrome is formed, characterized by superficial glossitis, dysphagia, cracks in the corners of the mouth, nail dystrophy, seborrheic dermatitis of the face, blepharitis, conjunctivitis, and decreased vision at dusk. B12 deficiency anemia associated with impaired absorption of this vitamin in the stomach due to anacid gastritis, tapeworm infestation, or increased consumption in pregnant women, manifested by Möller-Gunter glossitis (bright red tongue with smoothed papillae) and atrophy of the pharyngeal mucosa, burning pain in the tongue, weakness, crawling sensation in the limbs. A blood test reveals macrocytes, megalocytes, hyperchromic anemia, leukopenia.
Diseases of the spine [2] (cervical osteochondrosis, tuberculous spondylitis, radiculitis) can cause pain in the pharynx. Neuralgia of the glossopharyngeal nerve manifests itself as intense pain in the pharynx, especially against the background of chronic stress in anxious and suspicious patients. Metabolic disorders, intoxication, and trauma contribute to its occurrence. Characterized by unilateral pain in the root of the tongue, tonsil, lasting several minutes, accompanied by dry throat and subsequent hypersalivation. The therapeutic effect is achieved by lubricating the root of the tongue and pharynx with local anesthetics. Neuralgia of the superior laryngeal nerve [1, 6] gives similar symptoms, but also includes a painful dry cough and spasm of the vocal folds during inspiration [6].
Pain in the pharynx can be caused by an odontogenic process: periodontitis, teething pathology, galvanism [4, 17]. Rarely, unilateral pain in the pharynx occurs, the cause of which is the long styloid process (Eagle syndrome), accessible to palpation in the area of the palatine tonsil [15].
Rare causes of pain in the pharynx are ulcerations on the mucous membrane of tuberculous etiology [14]. In this case, there is a prolonged cough, weight loss, and swollen lymph nodes.
A final diagnosis is possible based on oropharyngoscopy. The main differential diagnosis for pain in the pharynx is between its most common causes - acute (or exacerbation of chronic) pharyngitis and sore throats caused by streptococcal infection (group A beta-hemolytic streptococcus - GABHS).
Acute pharyngitis is a viral infection of the pharynx in 90% of cases. Its main symptoms are: increased body temperature, sore throat when the throat is empty, when eating, soreness and a dry cough that does not bring relief. Patients indicate the localization of unpleasant sensations on the back wall of the pharynx. In the pharynx (Fig. 3), hyperemia of all parts is detected: the posterior wall, arches, tonsils, and there may be vesicular rashes (herpes, enterovirus). Plaques are not typical, there is often a runny nose and other catarrhal phenomena - nasal congestion, sneezing. If a rash is detected on the skin and mucous membranes, it is necessary to exclude an infectious disease - measles, scarlet fever, rubella [8]. Adenoviral infection manifests itself in the form of conjunctivitis, enlarged lymph nodes, fever, runny nose, and there may be plaque in the throat.
The disease progresses in waves: on the 7th–10th day of illness, a repeated increase in body temperature and a return of symptoms are possible. Enterovirus infection (“summer flu”) manifests itself in the form of dyspeptic, myalgic, and meningeal syndromes. Pharyngoscopy reveals bubbles on the mucous membrane of the oropharynx. In making the diagnosis of viral pharyngitis, the following help: knowledge of the epidemiological situation, dynamic observation of the patient, a variety of clinical manifestations (abdominal pain, vomiting, eye damage, meningeal symptoms, myalgia), lymphocytosis in the blood with normal ESR, lack of effect from antibacterial therapy, serological data research, polymerase chain reaction and others.
Sore throat is a general infectious disease with local manifestations in the form of acute inflammation of one or more components of the lymphadenoid pharyngeal ring, most often the palatine tonsils (tonsillitis), pharyngeal tonsil (adenoiditis), lingual tonsil, lateral ridges of the pharynx and larynx.
The classification of acute tonsillitis (according to I.B. Soldatov, 1975) involves the division into primary tonsillitis: catarrhal, lacunar, follicular, ulcerative-membranous; and secondary: for acute infectious diseases (diphtheria, scarlet fever, measles, tularemia, typhoid fever, infectious mononucleosis) and diseases of the blood system (agranulocytosis, alimentary-toxic aleukia, leukemia). There are special forms of tonsillitis [10]: viral, fungal, syphilitic.
With catarrhal tonsillitis, there is hyperemia and enlargement of the palatine tonsils, regional lymphadenitis, no plaque, a blood test shows slight leukocytosis, increased ESR. Catarrhal sore throat often has to be differentiated from viral pharyngitis, in which there is a cough, there may be a runny nose, and there is no enlargement or tenderness of the lymph nodes.
Follicular tonsillitis is manifested by bright hyperemia and swelling of the tonsils, subepithelial rounded yellowish elevations (follicles).
With lacunar tonsillitis, white-yellow plaques appear at the mouths of the lacunae of the tonsils (Fig. 4), which can merge with each other and cover the entire surface without going beyond the tonsils, being removed without leaving a bleeding surface, rubbing between two spatulas, dissolving in the vessel with water.
It is important to determine the streptococcal etiology of acute tonsillitis. This can be done using the McIsaac screening scale [12], which includes symptoms and their assessment in points (
).
A patient’s symptoms with a score of 3 means the probability of streptococcal etiology is 30%, and a score of 4 means about 70%. If the clinical picture is determined to be 0–1 points, then systemic antibiotic therapy is not indicated. At 2–3 points, antibiotics are necessary only if the infection is bacteriologically confirmed. Antibiotics should be prescribed when symptoms of 4–5 points are detected.
Diphtheria of the pharynx occurs in the form of localized, widespread, toxic I, II, III degrees and hypertoxic forms. With it, gray plaques are detected on the surface of the tonsils, tightly fused with the underlying tissues, they may spread to the arches, the mucous membrane of the posterior pharyngeal wall, the uvula (Fig. 5), and when you try to remove them, the mucous membrane bleeds. Plaques do not rub down and do not dissolve in water. In the toxic form, the neck is noticeably thickened due to swelling of the subcutaneous fat, pressure is painless and does not leave pits.
Infectious mononucleosis is an acute infectious disease caused by the Epstein-Barr virus, characterized by fever, sore throat, enlarged lymph nodes, pharyngeal tonsil, liver, and spleen. Plaques on the tonsils, as in lacunar tonsillitis (Fig. 6), but can spread beyond them. A general blood test (the appearance of atypical mononuclear cells), serological research methods (enzyme-linked immunosorbent assay (ELISA), Paul-Bunnel-Davidson reaction) help in diagnosing the disease.
Fungal infections of the pharynx in the form of curdled films, easily removed when scraped with a spatula, are caused mainly by yeast-like fungi of the genus Candida (about 90% of cases); less commonly, there are mold fungi of the genus Aspergillus, Penicillium [7]. C. albicans permanently or temporarily lives on human mucous membranes, skin and intestines. Factors contributing to the development of mycoses are: treatment with broad-spectrum antibacterial drugs, cytostatics and corticosteroids, diabetes mellitus, blood diseases, tumors, gastrointestinal diseases, vitamin imbalance. Candidiasis of the oral cavity, pharynx and esophagus occurs in more than 90% of AIDS patients (Fig. 7) [3].
Diagnosis of sore throats should include throat and nasal swabs for diphtheria (BL). Express determination of streptococcal antigen using test strips from the surface of the tonsils makes it possible to justify antibacterial therapy. A general blood test facilitates the differential diagnosis of primary and secondary acute tonsillitis. Opinions on the question “Should I do a smear?” controversial. It is needed to confirm the GABHS etiology of the disease in doubtful cases [16].
Therapeutic tactics for pain in the pharynx can be presented in the form of a diagram ().
For the treatment of acute pharyngitis, a gentle diet, hot foot baths, warm compresses on the front surface of the neck, warm alkaline drink (mineral water, milk with honey), steam inhalations, and smoking cessation are recommended. The attitude towards gargling is ambiguous [16]. Fresh infusions of mint, chamomile, calendula, eucalyptus, sage, and caragana are effective for relieving sore throat. Antiseptics of artificial origin (dichlorobenzene, metacresol, hexethidine, benzalkonium, thymol, ambazone, chlorhexidine) are bactericidal in their mechanism of action, which can lead to suppression of the normal microflora of the oral cavity, so they should be used with caution in children under 6 years of age [9]. For the treatment of sore throat, the most important painkillers are those containing menthol, tetracaine, lidocaine or flurbiprofen. Children from 6 months of age can use the herbal preparation Tonsilgon, which has an antiseptic and analgesic effect, but does not contain either menthol or lidocaine.
Menthol preparations and any sprays cannot be used before 3 years of age due to the possible development of laryngospasm.
Local combination drugs (antiseptics and painkillers) in the form of finished dosage forms are the most popular for the treatment of sore throat. One of them is TheraFlu LAR, a universal and highly effective local drug with an antiseptic and analgesic effect. TheraFlu LAR contains benzoxonium chloride and lidocaine. Available in the form of a spray and tablets, the content of lidocaine in which is 0–75 mg and 1 mg, respectively.
Recent in vitro and in vivo studies confirm the broad antiseptic spectrum of benzoxonium chloride and its activity against the main pathogens of the most common diseases of the oral cavity and pharynx. At the same time, the balance of the bacterial flora in the mouth is not disturbed, even with prolonged use of benzoxonium chloride.
Benzoxonium chloride has:
- bactericidal effect against aerobic and anaerobic gram-positive and gram-negative bacteria;
- fungicidal effect against Candida albicans, Aspergillus spp. and yeast fungi;
- antiviral activity against membrane viruses, including herpes virus, influenza virus, parainfluenza viruses, the causative agent of vesicular stomatitis.
Lidocaine is a local anesthetic that reduces pain in the throat when swallowing.
Adults should take the drug 1 lozenge every 2–3 hours (no more than 10 tablets per day) or as a spray, 4 sprays 3–6 times a day. Children aged 4 years and older are prescribed 1 lozenge every 2-3 hours (no more than 6 tablets per day) or as a spray, 2-3 sprays 3-6 times a day. The required duration of treatment, as a rule, does not exceed five days. The drug is well tolerated by patients, side effects are recorded extremely rarely. Possible short-term local irritation of the mucous membrane, allergic reactions.
Indications for its use are: pharyngitis, laryngitis, catarrhal tonsillitis, stomatitis, ulcerative gingivitis. Contraindications to the use of TheraFlu LAR: pregnancy (first trimester), breastfeeding, hypersensitivity to lidocaine, children under 4 years of age. TheraFlu LAR can be used by people with diabetes, as it does not contain sugar. Thanks to the combined effect - antibacterial and analgesic, TeraFlu LAR can relieve all symptoms of viral pharyngitis and be used in the complex therapy of bacterial sore throats.
Systemic antibiotic therapy in the treatment of patients with “sore throat” is indicated mainly for acute tonsillitis (angina) of suspected or established streptococcal etiology (GABHS) and is carried out with penicillins, and if they are intolerant, with macrolides; cefuroxime (Axetin) is effective. Clindamycin and lincomycin are reserve drugs [11]. Epiglottitis caused by Haemophilus influenzae is effectively treated with protected penicillins.
Literature
- Alimetov Kh. A. Secondary neuropathy of the upper laryngeal nerve / M materials of the anniversary All-Russian. scientific-practical conf. with international participation “Modern aspects and prospects for the development of otorhinolaryngology. M., September 29–30, 2005. P. 46.
- Alimetov Kh. A. Spondylogenic pharyngeal dyskinesia / Materials of the anniversary All-Russian. scientific-practical conf. with international participation “Modern aspects and prospects for the development of otorhinolaryngology. M., September 29–30, 2005. P. 22.
- Bessarab T.P., Yushchuk N.D., Anyutin R.G., Potekaev S.N. HIV infection in otorhinolaryngological practice // Attending Doctor, 2000. No. 1. P. 26–30.
- Inflammatory diseases of the mucous membrane of the pharynx, oral cavity and periodontium. Scientific review. Solvay pharma, 2002. P. 2.
- Diseases of the mucous membrane of the oral cavity and lips / Ed. E. V. Borovsky, A. L. Mashkilleyson. 1984. 400 p.
- Karpova O. Yu. Clinic, diagnosis and treatment of laryngoneurosis / Materials of the anniversary All-Russian. scientific-practical conf. with international participation “Modern aspects and prospects for the development of otorhinolaryngology. M., September 29–30, 2005. P. 53.
- Kunelskaya V. Ya., Kasimov K. On the issue of the clinic, diagnosis and treatment of candidal tonsillitis in children // Vestn. otorhinolaryngology. 1980. No. 4. P. 50–52.
- Nisevich N. I., Uchaikin V. F. Infectious diseases in children. M.: Medicine, 1985. 298 p.
- Acute respiratory diseases in children: treatment and prevention. Scientific and practical program of the Union of Pediatricians of Russia / Ed. A. A. Baranova. M., 2008.
- Otorhinolaryngology: national guide / Ed. V. T. Palchuna. M.: GEOTAR-Media, 2008. 960 p.
- Rational antimicrobial pharmacotherapy: Hand. for practicing doctors. Under general ed. V. P. Yakovleva, S. V. Yakovleva. M.: Litterra, 2003. 108 p.
- Sidorenko S.V., Guchev I.A. Tonsillopharyngitis: issues of diagnosis and antibacterial therapy // Consilium medicum. Infections and antimicrobial therapy. 2004. 4: 36–38.
- Folomeeva O. M., Amirdzhanova V. N., Yakusheva E. O. et al. Incidence of rheumatic diseases in the Russian population (analysis over 10 years) // Ter. Archive. 2002. No. 5. P. 5–11.
- Shevrygin B.V., Mchedlidze T.P. Handbook of otorhinolaryngology. M.: Triada-X, 1998. 448 p.
- Shulga I. A., Zaitsev N. V., Zaitseva V. S. Variants of the structure of the stylohyoid complex / Materials of the Anniversary All-Russian. scientific-practical conf. with international participation “Modern aspects and prospects for the development of otorhinolaryngology. M., September 29–30, 2005. P. 75.
- Etiopathogenetic therapy of diseases of the upper respiratory tract and ear: Methodological recommendations. Compiled by S.V. Ryazantsev, Kotserovets V.I. St. Petersburg: National Register, 2008. 100 p.
- Yakovleva V.I. Diagnosis and treatment of neurogenic diseases of the maxillofacial region: Textbook. manual for institutes and faculties. improved doctors. Minsk: Vysh. school, 1989. 102 p.
M. V. Subbotina , Candidate of Medical Sciences Irkutsk State Medical University , Irkutsk
Contact information about the author for correspondence
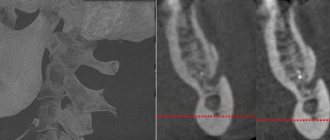
Diagnostic methods
The diagnosis is made by a neurologist, who, if necessary, can involve an otolaryngologist and dentist. During the examination, the doctor determines analgesia, that is, the absence of pain sensitivity at the base of the tongue, upper parts of the pharynx, and tonsils. Taste sensitivity is also studied, for which a taste solution is applied to symmetrical areas of the tongue. The diagnosis is confirmed by isolated unilateral taste disorder in the posterior third of the tongue. Bilateral disruption is typical for diseases of the oral mucosa, such as chronic stomatitis.
The pharyngeal reflex needs to be checked. To do this, touch the back wall of the throat with a paper tube, which provokes a swallowing movement and occasionally a cough. Normally, touching the soft palate should be accompanied by a lifting of the palate and uvula. Sicard syndrome is characterized by the absence of reflexes on one side. But a similar symptomatic picture can occur with damage to the vagus nerve. If the pharynx and pharynx are strewn with herpetic rashes, the doctor can diagnose ganglionitis of the ganglionitis of the glossopharyngeal nerve nodes, which differs in almost identical n. Glossopharyngeus clinical picture.
To establish the root cause of symptomatic neuritis, neuroimaging diagnostics is needed:
- MRI or CT scan of the brain;
- Electroencephalogram;
- Echo-EG;
- Ophthalmoscopy with consultation with an ophthalmologist.
It is necessary to distinguish between neuralgia of the glossopharyngeal nerve and diseases that cause painful paroxysms of the face and head. These include:
- Neuralgia of the ear ganglion;
- Trigeminal neuralgia;
- Oppenheimer's syndrome;
- Glossalgia;
- Ganglionitis of the pterygopalatine ganglion;
- Retropharyngeal abscess;
- Tumors of the pharynx.
Development factors
There are two forms of neuralgia:
- primary idiopathic glossopharyngeal;
- secondary (Sicart syndrome).
As a rule, neuralgia is a concomitant disease with various pathologies, for example:
- atherosclerosis with damage to the circulatory system;
- infectious lesions (for example, influenza or tonsillitis);
- intoxication with heavy metals and other harmful substances;
- tonsil injury;
- neoplasms in nearby areas;
- otolaryngological diseases;
- increased muscle pressure on the nerve;
- inflammatory processes in the brain, etc.
Taking into account the primary source, the patient is given conservative or surgical treatment.
Therapy
To treat neuralgia of the glossopharyngeal nerve, conservative therapy is prescribed. The only exception is if the underlying cause is tumors and hypertrophy of the styloid process, leading to compression of the nerve. In these cases, surgery is indicated.
To relieve pain, a 10% solution of cocaine is prescribed, which is applied to the root of the tongue and pharynx. This allows you to eliminate paroxysms for 6-7 hours. If this remedy turns out to be ineffective, a 1-2% novocaine solution is injected into the root of the tongue. Non-narcotic analgesics and anticonvulsants are also prescribed internally. If the pain syndrome is pronounced, it is advisable to prescribe sedatives, hypnotics, antipsychotic medications and antidepressants. AFT, multivitamin complexes and FiBS are used as general strengthening agents.
Among the physiotherapeutic procedures that have proven effectiveness are:
- SMT on the area of the larynx and tonsils;
- Diadynamic therapy;
- Galvanization.
1.General information
One of the paired cranial nerves is called the glossopharyngeal. This (IX) pair received its name in connection with the functions that it controls: the activity of the stylopharyngeal muscle, the sensitivity of the taste pimples of the basal part of the tongue, the secretory activity of the parotid gland, as well as the tactile sensitivity of a number of structures of the hearing organs and the oral cavity.
The term "neuralgia" is translated as "nerve pain" or "nerve pain." Neurogenic pain syndromes are distinguished by their specific nature (the pain is usually piercing, the sensations are similar to an electric shock extended over time), significant severity and persistence: it is impossible to find a forced position, conventional analgesics have little effect, etc.
A similar syndrome, caused by an isolated lesion of the glossopharyngeal nerve, is very rare in clinical practice - its statistical frequency is one case in approximately 620,000 people. Among the patients, men predominate, and in the age group - people over 40 years old.
A must read! Help with treatment and hospitalization!
Types of damage
Depending on the nature of the damage to the lingual nerve, the following types of nervous pathology are distinguished:
- Neuropraxia - occurs as a result of nerve stretching or blunt trauma without breaking the integrity. Changes in sensitivity in such cases subside over time, recovery takes several days throughout the week.
- Axonotmesis is nerve damage in which processes of degeneration and regeneration occur, while the axons retain their integrity. Normal sensitivity is restored (although not fully) within 2–4 months.
- Neurotmesis is damage to the integrity of the nerve, in which the prognosis for relieving neurosensory changes is very unfavorable and unpromising.
Most lingual nerve injuries are temporary, and approximately 90% resolve spontaneously after two months [2, 3]. If symptoms of damage persist for more than six months, then, unfortunately, the resulting nerve damage is almost irreversible. Symptoms of nerve damage include loss of sensation in the tongue, chin, or lower lip, as well as loss of sense of taste from the location of the damaged nerve.
How to protect yourself from lingual nerve damage
In order not to encounter this problem, you should contact a good specialist who can carefully plan and ensure qualified execution of the manipulations.
The lingual nerve provides sensation to the tongue. If unfavorable circumstances occur during the provision of dental care, it may be damaged. The nature and degree of the complication may be different - these indicators determine whether the functionality of the lingual nerve will be restored. Today, dentistry can offer complex therapy for successful but long-term restoration of lingual nerve function in more than half of cases.
Diagnosis of neuralgia of the submandibular and sublingual nodes
A neurologist can detect and diagnose diseases of the vegetative nodes during a personal examination of the patient. To establish an accurate diagnosis, topical diagnostics is used, which includes:
- patient interview;
- analysis of complaints;
- examination using palpation and additional techniques;
- as well as identifying objective signs of pathology.
Since there are several vegetative nodes in the head and face area, and the symptoms of their diseases are very similar, the main task of the neurologist during the initial examination will be to identify the location of the disease.
Using sliding and fixing palpation, the specialist identifies the localization of the pathological process. Sometimes pinching or superficial pain stimulation methods are used for accurate diagnosis.
If the doctor has doubts about the results of topical diagnostics, a diagnostic blockade technique is used, which makes it possible to absolutely accurately establish the source and localization of neuralgia. The blockade is carried out on an outpatient basis by injecting local anesthetics (novocaine, lidocaine, trimecaine) into the painful area. Pain relief for a while allows the doctor to make an accurate diagnosis.
Symptoms of neuralgia of the submandibular and sublingual nodes often have similar symptoms to inflammation of the gums and internal structure of the teeth. To rule out dental diseases, you may need to consult a specialist in this field.