One of the most severe, excruciating pains is toothache. It occurs for various reasons: caries, infection, loss of dental filling, inflammatory process, periodontal disease. In addition to severe pain, swelling of the cheeks, gums, and jaw may be observed. Failure to see a dentist in a timely manner often leads to the development of phlegmon and tooth loss. Broad-spectrum antibiotics are often used in dentistry. The drugs allow you to get rid of gumboil, inflammation, and pain. The remedies are selected individually and taken taking into account the doctor’s recommendation.
The main risk factors for the development of candidiasis include:
- improper oral hygiene;
- wearing orthopedic structures or removable dentures;
- long-term inhalation therapy;
- decreased salivation due to certain pathologies;
- hypothermia;
- stress;
- taking antibiotics;
- changes in hormonal levels;
- decreased immunity, including due to chronic diseases;
- endocrine pathologies, including obesity, diabetes;
- smoking;
- carrying out chemotherapy or radiation therapy.
Oral candidiasis occurs much more often in children than in adults. Newborns can become infected even in utero if the mother has thrush - infection occurs during natural childbirth. After birth, the infection can be transmitted to the child through the skin of the mother's nipples and hands, and from her oral mucosa. The source of infection is unsterile pacifiers and oilcloths, and medical personnel who do not follow the rules of asepsis and antisepsis during invasive procedures. In an older child, oral candidiasis is often caused by a weakened immune system or improper dental care.
Osteotropic antibiotics: what they are and what they are used for
Osteotropic antibiotics are often used in dental practice. An antibacterial drug (ABP) is prescribed:
- to eliminate the inflammatory-purulent process (chronic and acute) with peristitis, abscess, odontogenic sepsis, pericoronitis;
- as a prophylaxis against infectious complications after implantation and surgery;
- patients at risk (patients with diabetes, cardiovascular problems).
Antibacterial therapy is contraindicated for surgical interventions on bone tissue, bleeding, and large-area wounds in the oral cavity.
Oral candidiasis is divided into 3 types:
- Pseudomembranous. This is a classic thrush in the form of a superficial white film or white spots. Accompanied by a feeling of slight discomfort. In mild forms of the disease there may be only a few such plaques, and they can be easily removed. In severe cases, many large spots appear, they merge and gradually affect the entire mucous membrane, and can penetrate lower, affecting first the throat, and then the esophagus, up to the gastrointestinal tract. The spots may thicken, making them difficult to remove. Most often, ordinary acute candidiasis occurs in adults who have taken antibiotics, immunosuppressants or corticosteroids, as well as in infants.
- Atrophic. It can be acute or chronic. In the first case, there may be no plaque, but the mucous membrane becomes inflamed - it becomes bright red, the patient complains of a strong burning sensation in the mouth, increased dryness, and sometimes an unpleasant taste with a hint of bitterness or metal. Most often, acute candidiasis is a consequence of drug therapy. The chronic form usually occurs due to wearing orthodontic structures or dentures. The symptoms of the disease are more subtle.
- Hyperplastic. Candidiasis in the mouth affects the lips, corners of the mouth, cheeks, soft palate, and back of the tongue. White spots are usually large, merge with each other, and may acquire a yellow tint. Gradually they become rough and cannot be scraped off. The disease is chronic and is diagnosed only in adults.
Antibiotics for gumboil and inflammation of tooth roots -
Let's look at what antibiotics can be used for adults for gum gum disease. The choice here is quite large, for example, ranging from inexpensive antibiotics - such as lincomycin or amoxicillin, to more expensive drugs (for example, β-lactam antibiotics, 2nd generation fluoroquinolones and macrolides). Below we will look at the most popular antibiotics and tell you whether they work well for this type of dental inflammation.
1) Amoxiclav (or Augmentin) - these drugs contain a combination of “the antibiotic amoxicillin and clavulanic acid.” Many modern pathogenic bacteria produce β-lactamase enzymes that destroy amoxicillin. Clavulanic acid protects amoxicillin from the action of beta-lactamases, which greatly increases the effectiveness of the antibiotic. But using the most common amoxicillin (without combination with clavulanic acid) in dentistry today is already pointless.
The dosage regimen for adults is 500 mg 2-3 times a day (2 or 3 times depending on the severity of inflammation), the duration of administration is usually 5 days, but if necessary, the doctor can extend the drug for another 2-3 days. A package of the antibiotic Amoxiclav (15 tablets of 500 mg) costs from 330 rubles, and a package of the antibiotic Augmentin (14 tablets of 500 mg) costs from 180 rubles. And we do not recommend purchasing their Russian analogues containing a combination of “amoxicillin and clavulanic acid,” especially since they will not be cheaper.
Important: if you decide to purchase inexpensive amoxicillin (without clavulanic acid), then it should be used at least in combination with the antibiotic metronidazole (Trichopol). The latter is taken for purulent infections according to the same regimen - 500 mg 3 times a day (5-7 days in total). Only in this case can we expect at least some acceptable effectiveness from the treatment.
2) Ciprofloxacin (Tsiprolet) - this inexpensive, popular antibiotic belongs to the 2nd generation fluoroquinolones. The recommended regimen for use in adults is 500 mg 2 times a day (for 5 days), and the cost of a package of the Indian-made drug will be about 120 rubles. It works well for apical periodontitis, i.e. inflammation at the apex of the tooth root. In addition, the risk of developing diarrhea with this drug is lower - compared to β-lactam antibiotics (Amoxiclav, Augmentin).
Antibiotic Tsiprolet (10 tablets, 500 mg each) –
However, if we are talking about long-term apical periodontitis (especially if there have been cases of a fistula with purulent discharge in the projection of the tooth root), if there is acute pain indicating the formation of a purulent abscess at the apex of the tooth root, it would be optimal to prescribe an antibiotic containing the combination “ciprofloxacin” + tinidazole." These are drugs - “Ciprolet-A” or “Tsifran-ST”, in which, in addition to 500 mg of ciprofloxacin, each tablet also contains 600 mg of tinidazole. Their cost is from 210 and 320 rubles, respectively, but 1 package of each drug will be enough for you for a full 5 days of antibiotic therapy.
Tinidazole is an antibacterial drug with antiprotozoal activity, i.e. it is effective against anaerobic microorganisms (which are especially numerous during the formation of pus at the site of inflammation). In addition, tinidazole is very effective against Clostridium difficile and Clostridium perfringens, which are responsible for the development of diarrhea while taking antibiotics, and thus, when taking combination antibiotics with tinidazole, diarrhea is practically excluded.
3) Azithromycin (Azitral) - it is usually prescribed for allergies to β-lactam antibiotics (for example, amoxicillin). There are different regimens of use, but according to studies for purulent odontogenic infections, the optimal treatment regimen is to take a single dose of 1000 mg for 1 day, after which the drug is taken for another 2 or 3 days at a dose of 500 mg once a day. But the price of this antibiotic will be high if we do not take into account Russian manufacturers.
For example, a good Indian drug with azithromycin “Azitral” will cost you 220 rubles per package of 3 capsules of 500 mg (it turns out that you will need to purchase 2 packages for the course). The short course of use is due to the fact that this antibiotic has a cumulative effect, and therefore, even after taking it, therapeutic concentrations of the antibiotic remain in the body for several days.
Is it worth using Azithromycin for complications of caries (apical periodontitis, swelling or fistula on the gum, or gumboil on the face) - it’s definitely not worth it. This is due to the fact that in patients with inflammation at the apex of the tooth, drugs with azithromycin show good effectiveness only in 50% of cases, and in the remaining half of patients, the sensitivity of the microflora in the inflammation site to azithromycin is regarded as “low”. Below we will also demonstrate scientific works that confirm this.
4) Lincomycin or Clindamycin are quite old antibiotics belonging to the lincosamide group. Moreover, clindamycin is a more effective analogue of lincomycin (in terms of effectiveness against certain types of pathogenic bacteria that cause purulent inflammation, it is 2-10 times more effective than lincomycin). The peculiarity of these antibiotics is a certain affinity for bone tissue, which is an advantage for purulent inflammation in the teeth, as well as their low price. The disadvantages include a narrow spectrum of antimicrobial action, as well as the fact that they often cause diarrhea.
The regimen for taking Lincomycin is 2 capsules 3 times a day, for a total of 5 days (a package of the drug costs only 60 rubles). Clindamycin dosage regimen: 1 capsule 150 mg 4 times a day for 4 days. The latter is the drug of choice for allergies to β-lactam antibiotics, which include penicillins, amoxicillin, cephalosporins, etc. Affordable price – pack of 16 tablets. 150 mg each (made in Serbia) costs approximately 160 rubles. To prevent diarrhea while taking antibiotics, they should also be combined with tablets. Metronidazole.
Is it worth using Lincomycin - modern studies show that lincomycin shows good effectiveness only in 36.8% of cases (in at least 63.2% of cases - pathogenic bacteria in the inflammation site have only weak sensitivity to lincomycin). Moreover, if we are talking about a long-existing focus of inflammation in the area of the tooth root (in the presence of a fistula or purulent abscess), lincomycin is effective only in 19% of cases, at the same time in 47.6% of cases it demonstrates only weak effectiveness, and in the remaining 33 .4% of cases – patients have complete resistance of the microflora in the inflammation site to lincomycin.
It is also worth considering that lincomycin has very low bioavailability (when taken on an empty stomach, only about 30% of the drug is absorbed through the intestines). Simultaneous food intake reduces bioavailability by 4-5 times, i.e. bioavailability will be only about 5%. Taking on an empty stomach and poor bioavailability make the drug excessively harmful to the normal microflora of the stomach. In addition, taking Lincomycin can often cause antibiotic-dependent diarrhea.
SUMMARY (which antibiotic is better for inflammation at the root of the tooth) –
To compare the effectiveness of antibiotics in this article, the author of the article used personal experience in prescribing them, as well as the scientific work “Sensitivity of microbial associations of exudate of a periodontal pocket and odontogenic lesion to antibacterial drugs” (Makeeva I.M., Daurova F.Yu.), which was performed in 2016 at the Medical University. Sechenov, Moscow.
From this work we learn the following. In patients with apical periodontitis (inflammation at the apex of the tooth root), antibacterial drugs with the combination of amoxicillin + clavulanic acid were highly effective in 79-80% of cases, for ciprofloxacin (without tinidazole) - in 76% of cases, for azithromycin - from 66 % to 52% of cases, and for lincomycin - only from 36% to 19% of cases. Thus, if you have swelling of the gums or gumboil on your face, or there is acute pain when biting on a tooth, you should definitely not use lincomycin or azithromycin.
The 1st choice drugs are 2nd generation fluoroquinolones, namely the antibiotic ciprofloxacin (you can use the usual “Tsiprolet”, but the best drugs are those where ciprofloxacin is combined with tinidazole - these are “Ciprolet-A” or “Cifran-ST” ). Moreover, the last 2 drugs are the first choice drugs also for those patients who have a history of diarrhea during antibacterial therapy. In second place are β-lactam antibiotics such as Amoxiclav or Augmentin, which can be used as monotherapy or in combination with metronidazole (to enhance the effect in purulent inflammation).
If we are talking about the need for antibacterial therapy in a hospital setting (purulent abscesses, phlegmons, odontogenic osteomyelitis, etc.), then the drugs of first choice will be antibiotics of the cephalosporin group (i.m.), for example, the antibiotic Ceftriaxone.
Important: Remember that you should not take antibiotics on your own without a doctor's prescription. The choice of antibiotic is made by the doctor, taking into account the specific situation in the oral cavity, the severity of purulent inflammation, and also taking into account your chronic diseases. Antibiotics for gum gum disease are prescribed immediately after opening the tooth by a dentist, as well as after making a small incision in the gum (if necessary). But antibiotics cannot be a replacement for these medical procedures, because... Antibiotics are not able to “sterilize” infection in root canals and around the apex of the tooth.
Treatment with antibiotics for swelling of the gums near a tooth or acute pain when biting on a tooth is not the main treatment. If it is possible to save a tooth, the root canals must first be opened (to create an outflow of purulent discharge from the source of inflammation at the apex of the tooth root). And only after this are antibiotics prescribed. If you use an antibiotic just to suppress inflammation, you create a situation in which the infection at the site of inflammation becomes resistant to the antibiotic, and subsequent exacerbations of inflammation will be much more serious.
Antibiotics for toothache -
Tooth pain is a consequence of either inflammation of the nerve in the tooth (this disease is called pulpitis) or inflammation at the apex of the tooth root (apical periodontitis). Antibiotics for toothache do not quickly reduce it, because... they do not have an analgesic effect. True, they can reduce pain indirectly - by reducing inflammation, but this effect will develop for so long that it does not have any clinical significance.
An effective remedy for relieving toothache are non-steroidal anti-inflammatory drugs (NSAIDs), which include Nurofen, as well as other much stronger analgesics. You should start taking antibiotics before visiting the dentist only in one case, for example, if in the evening or at night you have acute pain when biting on a tooth or swelling of the gums/face, but you are planning an urgent visit to the dentist the next day.
Treatment of candidiasis in the mouth
There are several types of candidiasis of the oral mucosa, but treatment tactics do not differ significantly.
The most commonly used drugs for oral candidiasis are local antimycotics in the form of aerosols, solutions, gels, for example, fenticonazole, miconazole or amphotericin B.
Additionally, antiseptics with antifungal activity are used in the form of solutions for rinsing or lubricating lesions. For rinsing, preparations based on hexetidine and chlorhexidine are often used. A good medicine for candidiasis in the mouth is Lugol's solution, it is used to lubricate plaques.
To strengthen the immune system, it is recommended to take vitamins, especially C, P and group B.
Oral and even infusional antifungal antibiotics for oral candidiasis (sertaconazole, miconazole, isoconazole) are required for severe or chronic disease.
It is important that during the therapy period patients follow a diet that excludes fast carbohydrates (all types of sweets), since they are an excellent breeding ground for candida. Patients should refrain from eating sour and spicy foods.
When treating oral candidiasis in children, it is recommended to carry out “alkalinization” - treating pacifiers, bottles and toys that the baby may put in the mouth with a baking soda solution.
The choice of antimycotic drugs in the complex treatment of patients with oral candidiasis
M. O. Nagaeva Candidate of Medical Sciences, Associate Professor of the Department of Therapeutic Dentistry of the State Educational Institution of Higher Professional Education Omsk State Medical Academy of the Ministry of Health of the Russian Federation
M. G. Chesnokova Doctor of Medical Sciences, Professor, Department of Microbiology, Virology and Immunology of the State Educational Institution of Higher Professional Education Omsk State Medical Academy of the Ministry of Health of the Russian Federation
I. V. Anisimova Candidate of Medical Sciences, Assistant of the Department of Therapeutic Dentistry of the State Educational Institution of Higher Professional Education Omsk State Medical Academy of the Ministry of Health of the Russian Federation
The true incidence of oral candidiasis in Russia is unknown, since it is not officially registered, so publications on this problem in the domestic literature are few [5]. Colonization of mucous membranes by Candida fungi in practically healthy people ranges from 15 to 40% and can increase to 80% against the background of any pathology.
The relevance of research
Increased growth of the fungus, leading to the development of candidiasis, is observed when local and systemic immunity is impaired.
Exogenous infection is also possible. Superficial mucosal candidiasis also occurs in practically healthy individuals. Deep candidiasis develops with severe immunodeficiency against the background of candidal stomatitis, glossitis or pharyngitis. Fungi penetrate into the blood through damaged mucous membranes, causing fungemia and sepsis.
Treatment of candidiasis should be individual for each patient, taking into account the localization and severity of the process and the possibility of a chronic stage of the disease, taking into account the immune status and the presence of other diseases. Etiotropic treatment is the most important component of the complex treatment of patients with oral candidiasis. Eradication of the pathogen is the first step, after which one can proceed to the prevention of relapses and correction of local and general predisposing factors. Etiotropic therapy can be local (in the case of isolated candidiasis of the oral cavity) and systemic (if the infectious process spreads to the lower parts of the digestive tract, skin, and other mucous membranes). Systemic therapy for candidiasis of the oral mucosa is prescribed, as a rule, only for certain indications: chronic hyperplastic candidiasis, erosive-ulcerative form of candidiasis; oral candidiasis due to diabetes mellitus, immunodeficiency state; with ineffective local therapy.
The list of antifungal drugs is huge, and every year new drugs appear in the form of rinses, solutions, and tablet forms. The main group of specific drugs consists of antimycotic agents, but today the sensitivity of Candida fungi to them is variable and often insufficient. However, susceptibility testing is not considered routine, is not always available, and is not generally considered a standard practice in patient management. Susceptibility tests are considered useful in cases where we are dealing with deep infections caused by non-albicans Candida species. In these cases, especially if the patient has already been previously treated with antifungal azoles, the possibility of microbiological resistance should be considered.
The purpose of our study was to determine the sensitivity to antimycotics of strains of fungi of the genus Candida isolated from patients with oral candidiasis.
Materials and methods
At the Department of Therapeutic Dentistry of Omsk State Medical Academy and State Clinical Hospital No. 1 in Omsk, we conducted a clinical examination of 48 patients with complaints of pain and burning in the oral mucosa. The examination was carried out according to the algorithm proposed by Nedoseko V.B., Anisimova I.V. (2003) [3].
As part of a comprehensive examination of patients, a microbiological examination of material obtained by scraping from the mucous membrane of the dorsum of the tongue was carried out. The biomaterial was collected before treatment was prescribed using a dry sterile swab without the use of a transport medium. Before taking microbiological material, patients were advised to refrain from eating and hygiene procedures. The microbiological material was placed in a sterile transport tube and delivered to the bacteriological laboratory within two hours. In order to isolate facultative anaerobic microorganisms and yeast-like fungi of the genus Candida, the biomaterial was inoculated on nutrient media. A series of successive twofold dilutions of the material from 102 to 1012 was prepared. To isolate staphylococci, the corresponding dilutions were inoculated onto yolk-salt agar; to identify streptococci, inoculation was carried out on blood agar with sodium azide. To isolate bacteria of the genus Haemophilus and Neisseria, the material was inoculated on chocolate agar with lincomycin, enterobacteria on Endo medium, and enterococcal agar was used to detect enterococci.
To isolate fungi of the genus Candida, the biomaterial was inoculated on Sabouraud and Candiselect medium.
To identify fungi, cultural properties were assessed on Candisilect medium; biochemical identification was carried out using the Auxocolor test system.
To determine the sensitivity of yeast-like fungi of the genus Candida to antimycotic drugs (nystatin, amphotericin B, clotrimazole, fluconazole, itraconazole), the classical disk diffusion method and Fungitest were used.
To set up the disk diffusion method, a culture suspension was prepared in an isotonic sodium chloride solution, 1 ml of the suspension was poured onto the surface of the Mueller-Hinton medium. The results were recorded by measuring the diameter of the zone of inhibition of culture growth to the antimycotic.
To conduct the Fungitest, a suspension of fungi was prepared from a pure culture grown on Sabouraud’s medium—the first calibrated inoculum with a turbidity corresponding to the standard of 3 x 106 fungi/ml.
A 1:20 dilution of the primary solution was added to the suspension medium to obtain a standard inoculum (103 CFU/ml). The standard inoculum was added to the wells of the microplate. Incubated for 48 hours.
Research results and discussion
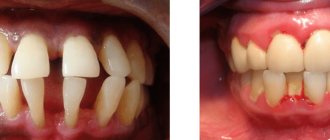
When examining 48 patients, we identified 23 patients with signs of oral candidiasis. All patients complained of pain, burning, and dry mouth. In 60.8% (14 patients) clinical signs of chronic atrophic candidiasis were detected (Fig. 1), in 39.2% (9 patients) chronic hyperplastic candidiasis was detected (Fig. 2).
Rice. 1. Patient K., 65 years old. Chronic atrophic candidiasis of the oral cavity
Rice. 2. Patient I., 69 years old. Chronic hyperplastic candidiasis of the oral cavity. Candida infection
As a result of microbiological examination of material from the oral cavity of 23 patients, 75 strains of opportunistic microorganisms were isolated and identified (48 strains of Candida albicans, 27 strains of opportunistic bacteria). Most of the isolated microorganisms were sown in significant concentrations (104 CFU - 29.3%, 106 CFU 40.0%, 108 CFU - 22.7%). At the same time, Candida albicans was most often found in association with S. epidermidis (104 CFU, 106 CFU), E. faecalis (104 CFU, 106 CFU), S. salivarius (106 CFU). When determining the sensitivity of Candida albicans fungi to antimycotic drugs, 18 (37.5%) strains with signs of resistance were identified. The greatest resistance of the isolated fungal strains was determined to nystatin (33% of sensitive strains) (Fig. 3).
Rice. 3. Sensitivity to antimycotics in the disk diffusion method
The sensitivity of Candida albicans to itraconazole, ketoconazole, 5-fluorocytazine and miconazole was 100% (Fig. 3, 4).
Rice. 4. Sensitivity to antimycotics in the Fungitest method
When determining sensitivity to fluconazole using the disk diffusion method, 94.4% of strains sensitive to fluconazole were identified. When using the Fungitest method, sensitivity to fluconazole at concentration 8 was 88.8%, to fluconazole at concentration 64 - 100%. 94.4% of C. albicans strains were sensitive to clotrimazole. All isolated strains were sensitive to amphotericin B(64); only 66.6% of strains were sensitive to amphotericin B(8). When determining sensitivity to amphotericin B by the disk diffusion method, 77.4% of the studied strains showed sensitivity.
Conclusion
When prescribing etiotropic treatment for patients with oral candidiasis, it is necessary to take into account the results of a mycological study with determination of sensitivity to antifungal drugs, since the isolated strains of Candida albicans showed resistance to antifungal drugs in 37% of cases. When choosing a method for determining sensitivity to antifungal drugs, it is necessary to take into account that the disk diffusion method is indicative; Fungitest has pronounced specificity and high sensitivity. In addition, the methods differ in the spectrum of antimycotics. Thus, to ensure the optimal choice of antifungal drugs in practice, we can recommend the use of two methods - both disc diffusion and the Fungitest method.
- Anisimova I.V. Clinic, diagnosis and treatment of diseases of the oral mucosa / I.V. Anisimova, V.B. Nedoseko, L.M. Lomiashvili. - M.: Medical book, 2008. - 194 p.
- Borovsky E.V. Diseases of the mucous membrane of the oral cavity and lips / E.V. Borovsky, A.L. Mashkilleyson. - M.: Medpress, 2001. - 320 p.
- Nedoseko V.B. Algorithm for examining a patient with diseases of the mucous membrane of the oral cavity and lips /V. B. Nedoseko, I. V. Anisimova // Institute of Dentistry. — 2003, No. 2 (19). - pp. 32-36.
A complete list of references is in the editorial office
Prevention
To prevent the development of the disease, you should carefully monitor the condition of the oral cavity. Every person is recommended to undergo a preventive examination at the dentist once a year and have their teeth treated on time. People who wear dentures should do so more often. Smoking is also one of the causes of thrush, so it is advisable to give up this bad habit.
During the period of antibiotic therapy, it is necessary to take eubiotics to correct the intestinal microflora.
1.General information
In order not to be interrupted by terminological references in the future, we will stipulate the following as a kind of preamble.
Opportunistic is an infection that occurs, literally, “at an opportunity,” “if possible,” i.e. under a certain combination of conditions favorable for the opportunistic microorganism. In turn, conditional pathogenicity implies asymptomatic parasitism or commensalism (harmless coexistence) of any microculture in the host’s body - as long as the host is healthy and immunocompetent - and the ability of this culture to undergo rapid pathogenic activation with a weakening of the immune defense, a significant change in the structure of the microbiome and some other circumstances.
Mycosis is a systemic infection by fungal cultures. Candidiasis is an extremely widespread (in fact, the most common) variant of mycosis, caused by yeast-like opportunistic fungi of the numerous genus Candida, most often Candida ablicans (the causative agent, in particular, of urogenital “thrush”).
Thus, pharyngeal candidiasis is an opportunistic mycosis caused by the activation of Candida and predominantly localized in one of the ENT organs.
A must read! Help with treatment and hospitalization!
Popular questions about candidiasis
How to determine candidiasis?
The disease has a specific symptom - white plaque in different parts of the oral cavity.
Which doctor treats oral candidiasis?
Dentist-therapist.
How is candidiasis treated?
Doctors usually prescribe the following medications to treat oral thrush: chlorhexidine or hexetidine solution, as well as nystatin, amphotericin B, or miconazole. They are available in different dosage forms (in the form of a gel, solution, aerosol), everyone will choose the one that is convenient for themselves.
Diagnostic methods
The treatment is carried out by a dentist-therapist. Diagnosis begins with an examination and a detailed survey: the doctor will find out what medications you have taken recently, and whether there are any chronic or infectious diseases. A cytological examination of plaque taken from the mucosa is mandatory. This is important because a buildup of non-fungal flora can easily be confused with a fungal infection.
The scraping is performed in the morning, on an empty stomach; there is no need to brush your teeth before the procedure. The day before, it is important to avoid eating foods rich in carbohydrates so as not to provoke the growth of pathogenic flora. Research allows not only to accurately determine the causative agent and type of Candida fungus, but also to find out the sensitivity of fungi to the main antifungal drugs. Based on the test results, the doctor will determine the fungus in the oral cavity and prescribe medication.
3. Symptoms and diagnosis
As a rule, pharyngeal candidiasis occurs with few symptoms or with moderate severity of clinical manifestations. Typical symptoms include inflammation of the tonsils and mucous membranes, a dirty white coating, low-grade fever, mild malaise, discomfort or pain when swallowing.
Granulomatous, atrophic, hyperplastic, erosive-ulcerative forms are relatively less common, requiring differential diagnosis, in particular, with tuberculosis.
Candidiasis of the pharynx is easily chronic and occurs, as a rule, in waves.
The prognosis worsens when the mycotic infection spreads to adjacent and internal organs.
If oropharyngeal candidiasis is suspected, a smear is taken from the affected surface, then a culture is performed on a nutrient medium; Recently, genetic identification (PCR) and serological tests (detection of specific antibodies) have been increasingly used.
About our clinic Chistye Prudy metro station Medintercom page!
NON-ODONTOGENIC AND SPECIFIC INFECTION
NECROTIC STOMATITIS (VINCINS ULCER-NECROTIC GINGIVOSTOMATITIS)
Main pathogens
Fusobacterium is concentrated in the gingival sulcus
, pigmented
Bacteroides
, anaerobic spirochetes. With necrotizing stomatitis, there is a tendency for infection to quickly spread into surrounding tissues.
The causative agents are F. nucleatum, T. vinsentii, P. melaninogenica, P. gingivalis and P. intermedia
.
In patients with AIDS, C. rectus
.
Choice of antimicrobials
Drugs of choice:
phenoxymethylpenicillin, penicillin.
Alternative drugs:
macrolide + metronidazole.
Duration of therapy:
depending on the severity of the current.
ACTINOMYCOSIS
Main pathogens
The main causative agent of actinomycosis is A.israelii
, association with gram-negative bacteria
A. actinomycetemcomitans
and
H. aphrophilus
, which are resistant to penicillin but sensitive to tetracyclines, is also possible.
Choice of antimicrobials
Drugs of choice
: penicillin at a dose of 18-24 million units/day, with positive dynamics - transition to step-down therapy (phenoxymethylpenicillin 2 g/day or amoxicillin 3-4 g/day).
Alternative drugs
: doxycycline 0.2 g/day, oral drugs - tetracycline 3 g/day, erythromycin 2 g/day.
Duration of therapy
: penicillin 3-6 weeks IV, drugs for oral administration - 6-12 months.