Surgical interventions in the complex treatment of periodontitis
The surgical stage is mandatory in the complex treatment of many inflammatory forms of periodontal disease. The main goal of periodontal surgery is to eliminate the etiotropic factor, create optimal conditions for improving oral hygiene, and eliminate periodontal pockets while stimulating the regeneration of periodontal tissue.
Treatment begins with a thorough examination of the patient, including general and local status. An important point is the assessment of the quality of oral hygiene at the preoperative stage of treatment, which is also a decisive factor in deciding whether to perform surgery.
At the initial stage of the oral cavity sanitation scheme, unpromising teeth are removed. When determining indications for tooth extraction, not only the degree of destruction of the marginal periodontium and pathological mobility are taken into account, but also the condition of the periapical tissues, the possibility of using the tooth to fix the prosthesis, position in the dental arch, continuity of the dentition, the form of destruction of the alveolar process, as well as the general health of the patient .
Indications for tooth extraction are the following clinical situations:
- degree III tooth mobility with bone loss of more than 70% in interalveolar height;
- damage to the bifurcation with loss of bone tissue in the interradicular space (grade III);
- destruction of bone tissue in single- and multi-rooted teeth below the apex;
- generalized loss of alveolar bone with retention of less than 3 mm at the apex;
- loss of bone tissue (more than 50%) in combination with damage to the dental pulp;
- the periapical focus of inflammation is connected along its length with the bone periodontal pocket;
- The periodontal focus of inflammation maintains a chronioseptic state in the patient and is the cause of focally caused diseases and autoallergic conditions (the focus of chroniosepsis).
- single standing movable teeth;
- preserved roots of decayed teeth that cannot be used in orthopedic structures;
- ineffective endodontic treatment (maintenance or increase in symptoms of periodontitis);
- the presence of foci of destruction at the root apex that do not tend to reverse development (based on x-ray).
Tooth extraction for inflammatory periodontal diseases is usually not difficult. After extraction, the wound heals by secondary intention. When the effect of the anesthetic wears off, slight pain appears in the wound, the severity of which depends on the traumatic nature of the procedure. From the socket of an extracted tooth, in addition to the primary one, secondary bleeding is possible, associated with chronic inflammation in the tissues, dilation of blood vessels and increased permeability of their walls.
Sometimes (from 2.7 to 10% of cases) alveolitis develops after tooth extraction. It can be caused by pathogenic microflora in the periodontal tissues and in the oral cavity, as well as the unsatisfactory general health of the patient.
For the treatment and prevention of alveolar bleeding and alveolitis, it is proposed to use various anti-inflammatory drugs: gelevit, oxycelodex, honsurid, catalugem, etc.
In particular, the use of a soft dressing “Solcoseryl dental adhesive paste” prevents bleeding from the socket and significantly reduces inflammation after tooth extraction in patients with periodontal diseases. The analgesic effect occurs immediately after applying the paste to the mucous membrane and lasts for 2-6 hours. The paste base consists of gelatin, pectin and carboxymethyl cellulose. After absorption of saliva or wound secretion, it forms a stable film.
Severe bleeding from the socket 15-20 minutes after tooth extraction is a contraindication for applying a dental dressing and requires careful hemostasis.
In some cases, tooth extraction due to periodontitis leads to complications associated with degenerative changes in hard and soft tissues. Microorganisms contained in periodontal pockets initiate the inflammatory process in the socket, since they can be pushed deep into the tissue during the application of forceps. Subgingival dental deposits remaining on the walls of the socket cause mechanical irritation and, in combination with existing pathological granulations, prevent wound healing. Gum tissues that have lost contact with the alveolar bone due to its destruction are often torn during tooth extraction, which maintains bleeding. Healing of the socket slows down because the marginal epithelium prevents the formation of granulations. In addition, a wide strip of marginal gingiva, when healing, forms a soft ridge along the alveolar edge, subsequently making it difficult to manufacture and fit orthopedic structures.
As a rule, supra- and subgingival deposits and granulations are not removed before tooth extraction. This is prevented by the mobility of teeth, which is actually the main reason for their removal.
In accordance with the facts presented, we have proposed a tooth extraction operation with preliminary excision of the epithelial edge of the gum (the instructions “Method of tooth extraction” are approved by the Ministry of Health of the Republic of Belarus).
Indications for surgery are the following factors:
- degree III-IV mobility of 2 or more teeth with uneven alveolar bone resorption;
- mobility of teeth III-IV degrees with mild gum recession and the presence of bone pockets;
- discrepancy between the clinical and radiological picture: degree II tooth mobility, gum recession of no more than 1/3 of the root; The radiograph reveals bone pockets up to the root apex.
Operation description
Pain relief is carried out using injection anesthesia, indicated for a specific area of surgical intervention.
Using an ophthalmic scalpel, incisions are made along the marginal gum from the vestibular and oral surfaces so that subsequently one flap is higher in height than the other. Their location depends on the location of the bone pockets and the level of alveolar bone resorption. From the side of the bone pockets, the incision passes below the marginal part of the gum by 1-2 mm; From the side of the preserved alveolar bone, the incision is made as close as possible to the edge of the gum. As a result, the last flap will be larger in height. The length of the incision has the shape of a straight line with the ends bent towards the crowns of the teeth that are not subject to removal (which subsequently close the dentition defect). An arch is formed at the end of the linear incision to prevent gum recession in remaining teeth.
Deep into the tissue, the incision is made at an angle from the edge of the gum to the level of the bottom of the periodontal pocket and extends all the way to the cementum of the root. This direction allows excision of the epithelium along the edge of the gum, pathological granulations in the pocket and subgingival dental plaque. Therefore, the angle of inclination of the spatula depends on the depth of the pocket and the thickness of the alveolar wall (Fig. 1).
Rice. 1. Scheme of excision of the epithelium along the gum edge.
Hemostasis is carried out, and the operation to remove mobile teeth (usually 2-3) is immediately performed. When applying forceps, tissues excised from the oral and lingual sides of the tooth are captured. The hole is filled with a preparation containing hydroxyapatite. The material must be chemically stable in the physiological environment of the body, exhibit resistance to oxidation, prevent the accumulation of harmful reaction products, and not cause galvanic-electric phenomena.
These requirements are largely satisfied by materials containing hydroxyapatite [Ca10(PO4)6(OH)2] with a Ca/P ratio of 1.67, which is an analogue of the inorganic component of the bone and dental tissues of the body.
Calcium reduces the permeability of cell membranes and the vascular wall, preventing the development of inflammatory reactions. Hydroxyapatite gel helps accelerate the healing of bone wounds, the formation of a functionally and structurally complete osteoregenerate according to the type of primary healing. The use of the drug allows you to reduce the duration of pain in the postoperative period and promotes the rapid elimination of edema in all categories of patients.
The wound is sutured in such a way that the more movable flap covers the tooth socket. As a result, the suture passes not in the center, but along the edge of the alveolar ridge, which improves the conditions for wound healing. The number of stitches depends on the length of the incision: one stitch is placed at a distance of about 1 cm from the other.
The incisions made in this way ensure the extraction of the tooth(s) from the socket simultaneously with the inner epithelial lining of the marginal gum, granulations and subgingival deposits. As a result, the risk of microbial contamination of the tooth socket is reduced compared to the classic removal of mobile teeth. Wound healing is accelerated because it occurs by primary intention. In addition, partial excision of the marginal gingiva prevents the formation of a mobile marginal ridge along the alveolar bone. Filling the socket with a material containing hydroxyapatite reduces the risk of further atrophy of bone structures and a decrease in the level of the alveolar margin.
Depending on the clinical picture of periodontitis, other surgical interventions on the tissues of the oral cavity may be performed. For painless treatment of soft tissues, teeth and bones, local anesthesia is usually used: in the upper jaw - infiltration, in the lower jaw - often conduction. Depending on the goals, surgical interventions are divided into 3 groups: operations within the free and attached gums (curettage, gingivotomy, gingivectomy); operations within the free, attached gums and alveolar mucosa (frenulotomy, lip and tongue frenuloplasty, vestibuloplasty, closure of gum recession); operations on the gums, alveolar mucosa, bone tissue of the alveolar process (operations according to Widman; operations according to Neumann; modified operations according to Kirland, Ramfiord, Nissle; operations of apical displacement of the flap).
The purpose of the operations of the first group is the elimination (revision) of pockets (true and false), which are places where microbes and their metabolic products accumulate. A necessary condition for these interventions is the normal width of the attached gum and the absence of pathology of the architectonics of the vestibule of the oral cavity.
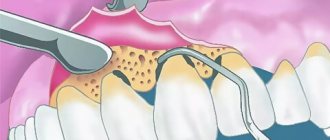
Closed curettage is indicated for shallow (up to 4-6 mm) gum pockets; as a palliative method of surgical intervention, it can also be performed for deeper pockets. Contraindications include fibrous changes in the pocket wall, thinned gums, and abscess formation. It is carried out with a sharp excavator and curettes after preliminary opening. In this case, subgingival dental deposits are removed and the inner walls of the pocket are scraped out. It is advisable to remove tartar using ultrasonic devices. This achieves greater surface cleanliness and increases the antimicrobial effect when using chlorhexidine solution as an irrigation liquid. The disadvantage is the lack of visual control of the walls and bottom of the pocket.
Open curettage was proposed to eliminate the shortcomings of closed curettage. A scalloped incision is made along the gingival margin, beveled inward to the base of the pocket. The flaps are peeled off, the remains of tartar and granulation are removed, the flaps are de-epithelialized, placed in place and fixed with sutures in the interdental space.
Gingivotomy is indicated for deep and narrow periodontal pockets. In this case, the pocket is dissected along its entire length, then the edges of the flap are separated, dental plaque is removed, the inner surface of the pocket is de-epithelialized, and the wound surface is treated with an antiseptic. The flaps are placed in place and secured with sutures.
If there is an abscess, the incision is made horizontally, the wound is washed and drained using a rubber strip. Gingivectomy is indicated in the presence of periodontal pockets. One of the conditions is a sufficient width (at least 2 mm) of the attached gum zone, which should remain after excision of the pocket to its full depth. The operation is not performed when bone pockets form.
Osteomucogingival operations (flap according to Widman, Neumann) are performed in the presence of bone pockets. Two vertical incisions are made, usually involving 4 teeth. A horizontal incision is made, slightly retreating from the gingival margin, on the vestibular and lingual sides. Mucoperiosteal flaps are peeled off. Granulation tissue and remaining dental plaque are removed, and bone pockets are eliminated. If necessary, the relief of the outer surface of the bone of the alveolar ridge is modeled, which ensures the maximum possibility of wound healing by primary application. The flaps are placed in place and fixed in the interdental spaces with interrupted sutures.
Modifications of flap operations are numerous, and all of them are aimed at increasing the effect by minimizing the disadvantages inherent in known interventions. The most typical is postoperative tissue retraction. In this regard, osteoplastic materials are used in combination with the technique of directed regeneration of bone structures.
Flap surgery with cementotomy and dental immobilization
The indication for surgical intervention is localized periodontitis, involving 3-4 teeth with exposed roots, grade I-II mobility, and the presence of bone pockets.
Anesthesia is administered to the corresponding area of the jaw. The operation begins with dissection of the soft tissues in the interdental spaces with a sickle-shaped scalpel. The direction of the incision in the interdental space is parallel to the base of the papilla between the proximal sides of the teeth. In this case, the cutting instrument, sliding along the vestibular surface of the tooth with its plane, enters the periodontal pocket and is directed to the middle of the proximal surface of the adjacent tooth until it stops. Following this, the cutting part of the instrument moves in the direction from the root to the crown of the tooth. Dissection of interdental soft tissues is carried out in a section of the dentition that exceeds the area of the intended intervention by 1-2 teeth on each side (modification of the incision by V. I. Lukyanenko, 1973). This makes it possible, while maintaining the area of the surgical field, to do without vertical incisions, which increase gum recession in the postoperative period. Vertical incisions are made in exceptional cases, when the surgical field is located on an area in the projection of no more than 3 teeth, especially in the lower jaw. Then, alternately from each side, sliding along the surface of the tooth with a rasp, they enter the periodontal pocket and, moving the instrument to the apical part, with fan-shaped movements, peel off the flaps on both sides of the alveolar process throughout the entire incision and to the depth of the lesion. Then the flaps are retracted from the bone to a distance that allows free manipulation in the surgical field.
Removal of granulations and vegetations of the epithelium begins from the apical parts of the surface of the flaps, and a scalpel can be used, which, during manipulation, is at an angle of 30° to 90° with respect to the surface of the flap and moves from the base of the flap to the periphery, scraping off granulations and vegetations . During the removal of granulations and vegetation from the flap, the outer surface of the flap is placed on the index finger. This ensures its reliable fixation and control of the depth of immersion of the cutting tool into soft tissue. Next, they begin to remove granulations adjacent to the tooth and alveolar bone. At this stage, scalers and small curettage spoons are used. If there are sharp bony protrusions on the alveolar process, they are ground off with a diamond head.
Treatment of the roots of non-pulp teeth is carried out by scraping with sharp instruments (excavator, sharp hooks of various shapes) surface deposits of tartar along with granulations and necrotic tissue on the surface of the cement. The roots of pulpless teeth are subjected to cementotomy. In this case, the root surface is periodically stained with a 2% aqueous solution of methylene blue or other neutral dyes. Cementomy is completed with an elongated bur with a blunted and polished end part, holding it at different angles relative to the surface of the tooth root (from 20° to 90°). Preparation is carried out until the stained areas of the tooth root disappear. After this, the treated surfaces are polished with polishers. The wound is thoroughly washed with antiseptic solutions (furacillin, 1% hydrogen peroxide solution, etc.) under pressure from a syringe with a blunt needle. Before placing the flaps in place, if necessary, the periosteum and submucosa are dissected along the entire length, creating conditions for displacing the flaps in the coronal direction. Due to the fact that during this operation the edge of the flap largely retains its original shape, it is possible to completely restore the anatomical configuration of the dental papillae. Sutures are made of catgut with an extended resorption period, the nodes are left at the level of the interdental spaces 1-2 mm below the base of the papilla.
When the interalveolar septa are resorption by more than half, the flaps are sutured with U-shaped sutures, creating so-called cuffs around the teeth.
Splinting teeth for periodontitis
To restore the chewing activity of mobile teeth, reduce the inflammatory process in the periodontium and prevent complications, splinting and/or the production of permanent dentures are used.
A splint is a type of denture that connects adjacent teeth into a single system, evenly distributing the chewing force and eliminating traumatic occlusion. In accordance with this, the splint must meet a number of requirements: firmly fix and not displace teeth without introducing excessive load, leave interdental spaces free, and not interfere with brushing and self-cleaning of teeth.
Indications for temporary splinting:
- tooth mobility I-III degrees;
- bone resorption of more than 1/2 of the root length;
- preparation for periodontal surgery;
- creating conditions for professional oral hygiene;
- replacement of minor dental defects;
- preparatory stage for permanent splinting;
- stabilization of the results of orthopedic and orthodontic treatment.
The simplest temporary structure is a wire splint that is placed tightly over the teeth just below the equator. In most cases, 6-8 teeth are connected with a block in such a way that the splinted teeth individually are not mobile.
Removable splints rest on the crown of the teeth and consist of hook clasps surrounding the teeth. In cases of low tooth mobility, these splints provide satisfactory support, but their fixing effect is significantly less than that of permanent splints.
When making removable splints, you need to ensure that they do not interfere with the closure of the dentition, so that at rest the splint fits exactly to the teeth without tension and maintains its position when chewing. The advantage of the splint is good fixation of the teeth in relation to horizontally acting forces, ease of manufacture: the teeth do not need to be ground, and the pulp does not need to be removed. The negative side of this splint is its low aesthetics due to the clasp located on the cheek side.
When making permanent (fixed) splints, artificial crowns are put on individual teeth, which are connected to each other, and thus a stable system is formed.
A fixed splint can be applied to teeth with intact pulp or root filling. The structure must be made in such a way that chewing pressure is evenly distributed over all supporting teeth, eliminating overload of individual teeth, and ensuring protection of the gums and periodontium.
Indications for adhesive prosthetics:
- splinting of the dentition for periodontal diseases complicated by partial edentia - included defects of the 3rd and 4th Kennedy classes of small extent (1-2 teeth in the anterior part of the dentition, 1 tooth in the lateral part);
- splinting a group of teeth after orthodontic treatment;
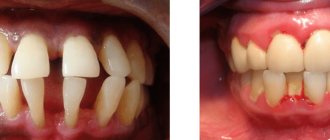
- splinting a group of mobile teeth in order to redistribute the load and ensure the stability of these teeth (Fig. 2);
Rice. 2. Splinting of teeth before surgical treatment.
- splinting the frontal area of the dentition if it is necessary to preserve aesthetics and it is impossible to manufacture traditional aesthetic structures;
- splinting of the dentition with a well-preserved anatomical shape of the coronal part of the tooth and with bone resorption of no more than 1/2 of the root length;
- splinting of the frontal area of the teeth with the possibility of preserving their vitality.
A correctly made splint secures the teeth well and leaves the interdental spaces free, thereby ensuring the ability to maintain oral hygiene, slows down or stops the development of the pathological process during the complex treatment of periodontitis.
The most common periodontal diseases
The periodontium is an anatomical structure that unites the tissues surrounding the tooth and holding it in the socket.
This supporting-fixing function is provided by the gum with the periosteum, alveolar bone, periodontium, and tooth cement. It follows from this that periodontology is not only a science that deals with the treatment of gums. It covers a wider range of different pathological conditions. When exposed to negative factors and pathogens, the following periodontal diseases develop:
- Gingivitis is an inflammation of the gums that occurs without compromising the integrity of the periodontal junction. In terms of prevalence, the process can be localized, generalized, and in form - catarrhal, ulcerative, hypertrophic. Treatment tactics will also be determined by the severity of the disease.
- Periodontitis is an inflammatory disease of periodontal tissues that occurs with damage to the dental-gingival junction and is a consequence of insufficiently effective treatment of gingivitis.
- Periodontal disease or (generalized form of periodontitis) is a non-inflammatory process characterized by dystrophic damage to periodontal tissue.
Much less frequently, periodontal damage can be caused by uncompensated diabetes mellitus and other somatic disorders. There are also cases of tumor growth of periodontal tissues.
Attention to periodontal problems is due not only to the widespread prevalence of pathology among diseases of the dentoalveolar region, but also to the fact that poor-quality treatment measures and their delay lead to a deterioration in the stability of teeth and subsequent loss.
In Moscow, specialists from the Dental Studio clinic are actively involved in the issues of periodontology and gum treatment. Periodontology is a complex science, so prices for the treatment of gums and other pathologies in this area are justified.
Closing gum recessions
Closing gum recessions is carried out only by surgical methods, which involve moving donor flaps to the recession zone and plastic surgery of the existing defect. You can receive a transplant in several ways:
- Pedicled flap. In this case, the donor tissue is a nearby area of the mucous membrane. The technique is used in the presence of localized defects.
- Gingival flap. It is taken from the gum area, provided that the volume of tissue in the selected area is sufficient.
- A scrap from the sky. In this case, the donor fragment is taken from a specific area of the hard palate
To close recession zones, the method of directed tissue regeneration can be used. In this case, special membranes are used as donor tissue, which can be absorbable or non-absorbable. These membranes promote the migration of cells from natural tissues and subsequent regeneration of the damaged area.
This method does not require the formation of a donor wound, but is not suitable for all patients. To obtain a successful result, the membrane must be covered with a layer of mucous membrane, which will provide the necessary nutrition, which is not always possible. In addition, due to the long process of formation of new tissue, it is necessary to observe certain rules of oral hygiene, therefore this method requires the active and conscientious participation of the patient in the treatment process.
Diagnostics
- Taking anamnesis;
- dental examination with measurement of the depth of periodontal pockets (periodontogram);
- orthopantomogram (OPTG), CT;
- rheoparodontography (assess the tone of blood vessels);
- Schiller-Pisarev test;
- microbiological studies (PCR);
- blood tests (general, sugar).
Differential diagnosis of periodontitis is carried out with gingivitis, eosinophilic granuloma of the jaw, periodontal changes in Lefebvre-Papillon syndrome. What examination methods will be required depends on the form and severity of the disease.
Open curettage of periodontal pockets
This type of operation does not have the disadvantages of the previous method. A good overview of the problem area allows the doctor to remove all granulation tissue and thereby prevent further progression of the disease. Open curettage is performed under local anesthesia and takes place in several stages:
- The surgeon makes an incision in the gum in the projection of the neck of the tooth.
- A certain area of the mucous membrane peels off.
- Granulations and deposits in periodontal pockets are eliminated.
- If necessary, plastic surgery of bone defects is performed.
- The flap is sutured, the surgical field is treated and protected with an aseptic dressing.
Due to the high traumatic nature of soft tissues, a limited area of gum can be treated in one operation, usually up to 8 teeth. After the wound has healed, repeated interventions are performed.
What are the possible complications?
Improper teething, accompanied by pericoronitis without treatment, can lead to the following serious complications:
- Formation of necrotic ulcers along the gingival margin. Subsequently, necrosis can spread to other tissues of the oral cavity;
- Damage to healthy neighboring teeth;
- Phlegmon of the perimaxillary spaces;
- Periostitis, which easily spreads to nearby areas;
- Osteomyelitis;
- Abscess formation.
Any of these pathologies can become life-threatening, so treatment of inflammation of the mucous membrane must be timely.
Treatment of pericoronitis is not difficult. A timely visit to the dentist and diagnostics will allow you to immediately carry out the correct treatment. For example, if a tooth initially erupts incorrectly, then removing it at the very beginning of the process will avoid further discomfort.
If for one reason or another it was not possible to visit a doctor on time, then you should come for a consultation when the first signs of inflammation appear. The purulent form is much more difficult to treat and causes more inconvenience. In addition, pus is the main cause of complications.
The post Treatment of pericoronitis appeared first on.
]]>
How to restore teeth with severe periodontitis
In severe cases of the disease, the risk of losing a tooth or an entire row of teeth is very high. Tooth extraction for periodontitis is indicated in cases of excessive mobility, when the unit is barely held in the bone and moves in all directions around its axis. If it is impossible to save the tooth, orthopedic treatment is carried out - prosthetics supported by natural teeth or implants.
For single defects or restoration of a tooth segment, two-stage implantation with delayed loading is used. Implants are implanted after a course of gum treatment and restoration of bone volume. Bone parameters are restored through osteoplastic surgery. After new bone tissue is formed (after 6 months), implants are implanted, the prosthetic system is fixed after they have fused with the jaw bone ( after 3-6 months
). Treatment may take about a year.
In case of complete edentia, one-stage implantation methods with immediate loading demonstrate high efficiency. The ability to install implants in deep bone layers that are not subject to inflammation allows you to avoid osteoplasty and sinus lifting. Treatment will take no more than a week.
Possible signs
Based on the nature of the flow, the following options are distinguished:
Acute catarrhal pericoronitis
During the process of teething, the patient experiences unpleasant sensations, which intensify when eating. The mucous membrane in the affected area will be red, swollen and painful when touched. Regional lymph nodes increase in size. Their palpation becomes painful.
Acute purulent pericoronitis
With this form of the disease, pain increases. Purulent discharge appears from under the hood. Pain when eating is accompanied by discomfort when swallowing. Mouth opening is limited.
The patient's general condition changes. There is an increase in body temperature to 37.5-38 degrees. Sleep is also disturbed and appetite is lost.
Chronic pericoronitis
The chronic course of the disease occurs if the necessary treatment is not carried out in a timely manner. Painful sensations decrease in intensity and appear only periodically. Since the hood remains, food continues to get trapped under it. This leads to bad breath. Regional lymph nodes are slightly enlarged and painful only on palpation. Swallowing and mouth opening are not impaired.
Closed curettage of periodontal pockets
Closed curettage or curettage is one of the few methods of treating periodontitis that allows you to eliminate granulations and various types of dental plaque from periodontal pockets. However, due to the lack of visual control, the doctor is not always able to completely eliminate these problems, which reduces the effectiveness of this method. That is why it is used for shallow periodontal pockets, which is typical for the earliest stages of the disease. With a more extensive lesion, the technique can only temporarily improve the patient’s health, but sooner or later periodontitis will begin to recur, which will require re-treatment.
Among the advantages of this type of surgical treatment are:
- Good aesthetic result.
- Rapid gum recovery.
- Minor blood loss.
Due to the features described above, closed curettage is not always used.