I degree - sensitivity and movement in the limb are preserved:
- IA – coldness, paresthesia, numbness of the limb
- IB - pain in the distal parts of the limb at rest.
II degree – disorders of movement and sensitivity of the limb occur:
- IIA – limb paresis (decreased muscle strength and range of active movements in the distal parts)
- IIB - limb paralysis (lack of active movements)
III degree – necrobiotic phenomena develop:
- IIIA – subfascial edema
- IIIB – partial muscle contracture
- IIIB – total muscle contracture
The degree of limb ischemia is taken into account when choosing a treatment method for acute vascular occlusion.
General information
Vascular occlusion is a blockage (more often of arteries than veins), which is characterized by a pronounced decrease in the speed and quality of blood flow. Occlusion can cause necrosis and, as a result, lead to death.
The pathology is quite common and can affect the organs of visual perception, the central nervous system, limbs and great vessels. sepsis and peritonitis develop . Abdominal ischemic syndrome develops against the background of a lack of adequate blood circulation in the digestive tract. The pathology is associated with occlusion of the unpaired visceral branches of the abdominal aorta - the celiac trunk and mesenteric arteries (superior, inferior). Abdominal toad can develop under the influence of both internal ( thrombosis ) and external factors (traumatic occlusion).
What is an occlusive dressing?
This method of sealing the lesion is used for wounds that require maintaining sterile conditions and protection from the external environment.
Applying an occlusive dressing to the knee joint requires certain skills and technique:
- cover the wound surface with sterile gauze;
- Place the top of the scarf on the thigh area and wrap it around the waist;
- bend the bandage at the base by 2 cm;
- cross the ends under the thigh, tie knots on the thigh;
- Throw the top over the knot formed and then pass it under the knot.
What else causes stenosis?
More rare cases are associated with a specific pathology. Narrowing of the arterial vessel is observed with a disease of the connective tissue that forms the stroma of the artery. This is called fibromuscular dysplasia - the vessels cease to maintain tone and collapse, stopping blood flow. Stenosis can accompany some inflammatory diseases of the vascular wall - arteritis, systemic vasculitis, Takayasu's disease, Horton's disease. There are rare pathologies, for example moyamoya disease, in which there is a slow progressive narrowing of the lumen of the arteries.
Stenosis can occur after an injury - a strong blow, a concussion. After some traumatic brain injuries, a special hematoma is observed - subintimal, which has the appropriate localization. A blood clot that forms due to increased blood clotting and rare types of anemia can block the lumen. There is antiphospholipid syndrome, in which young patients experience heart attacks and strokes precisely because of increased coagulation. Blood clots form when heart rhythm disturbances occur while taking certain medications.
The narrowing may be due to congenital structural features of the vessels - they can be tortuous and hypoplastic. Vascular pathology accompanies systemic diseases, diabetes, obesity and metabolic disorders.
Pathogenesis
When the blood thickens, there is an accumulation of fibrin in its composition, which leads to thrombus formation . Venous formations are characterized by constancy - they are located in one area and clog the vessels of the extremities, leading to necrosis and gangrene . Arterial formations are characterized by migration; they often break away from the original source and disrupt the blood supply to large organs, provoking the development of stroke , heart attack and other dangerous conditions.
Prevention
Distal occlusion develops in childhood. Attentive parents can prevent the development of irreversible changes. Prevention of postural disorders, timely treatment of diseases of the ENT organs, fight against bad habits, early treatment of caries of primary teeth will prevent deformation of the facial skeleton and improper growth of teeth. If violations are detected, you need to make an appointment with the orthodontist as soon as possible. The younger you are, the easier it is to correct your bite.
Classification, types of occlusion
It is customary to distinguish between arterial and venous occlusion.
Types of occlusion by localization:
- Occlusion of mesenteric vessels . It is characterized by an acute circulatory disorder in the mesenteric vessels, which inevitably leads to intestinal ischemia. As a result of thrombosis, the trophism (nutrition) of the intestinal walls is disrupted, and an acute inflammatory process develops, including peritonitis .
- Occlusion of cerebral vessels. The gradual growth of cholesterol plaques in volume can lead to complete blockage of the vessels supplying blood to the brain. The vessels lose their elasticity and a blood clot forms at the site of attachment of the cholesterol plaque as a result of platelets adhering to the damaged vascular wall.
- Occlusion of the arteries of the lower extremities. In this case, a sharp closure of the lumen of the peripheral artery and the development of an acute form of ischemic syndrome are characteristic. Such changes lead to disruption of trophism and nutrition of the lower extremities, paralysis and even gangrene . With occlusion of the femoral artery, extensive circulatory disorders develop not only in the lower extremities, but also in the pelvic organs, which can pose a real threat to the life and health of the patient. Both the superficial (SFA) and deep femoral artery can be affected.
- Occlusion of cardiac vessels. Damage to the coronary arteries is very common. When the supply vessel is completely blocked, irreversible consequences develop in the form of necrosis - myocardial infarction . ischemia develops , which manifests itself as signs of angina pectoris . The blockage can occur due to a blood clot or atherosclerotic plaque. With long-term, chronic occlusion, bypass pathways are formed - collaterals, through which nutrients are supplied. In 98% of cases, the coronary arteries are affected by atherosclerosis .
- Occlusion of the subclavian artery. As a result of blockage, ischemia occurs not only in the upper extremities, but also in the brain. Dizziness , weakness in the arms, problems with speech and visual perception appear The consequences of occlusion of the subclavian arteries are severe.
- Occlusion of the carotid artery. There is both complete and partial blockage of the vessels that supply blood to the brain. Occlusion of the internal carotid artery, which nourishes and supplies the brain and is responsible for intracranial circulation, is rare. Damage to the common carotid artery can lead to problems with visual perception.
- Occlusion of the iliac artery. The first manifestation of the lesion is numbness in the legs, fatigue, ischemia of the legs, and the appearance of pain when walking. Gradually, damage manifests itself in the functioning of the pelvic organs, impotence , and the functioning of the abdominal organs is disrupted.
- Occlusion of the eye or occlusion of the retinal artery. It is extremely rare. It is characterized by a completely asymptomatic course and a sudden deterioration in vision up to complete blindness.
Occlusion in dentistry
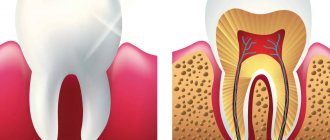
In dentistry, occlusion is closure, i.e. the most complete and dense contact of the chewing surfaces with each other. In simple words, dental occlusion is the relationship of the jaws relative to each other.
The occlusal surface of the tooth is that part of the tooth surface that is located from the deepest part of the central fissure to the top of the cusps.
6 keys of occlusion according to Andrews
Andrews is credited with formulating his own theory based on crown morphology and evaluating 120 models with “ideal” occlusion in orthodontically untreated patients. He developed rules (keys) for the relationship of a single tooth to both the adjacent and the antagonist tooth, taking into account its position.
- Key 1 – ratio of painters;
- Key 2 – mesiodistal type (crown angulation);
- Key 3 – torque and inclination of tooth crowns;
- Key 4 – rotation;
- Key 5 – contact point;
- Key 6 – Spee curve.
Central occlusion
The definition includes other names:
- intertubercular contact;
- maximum closure of teeth;
- intertubercular contact position;
- intercuspation.
Central occlusion determines the position of the lower jaw, which is characterized by:
- uniform, symmetrical contraction of the muscles that raise the lower jaw;
- the central position of the heads of the temporomandibular joint in the articular fossae;
- maximum fissure-tubercle contacts of the dental rows.
Dental signs of central occlusion:
- Between the teeth of the lower and upper jaws there is the most dense tubercle-fissure contact.
- Each tooth intersects with two antagonists. The only exceptions are the lower central incisors and upper third incisors.
- The midlines between the central lower and upper incisors are located in the same sagittal plane.
- The lower teeth overlap the upper teeth by no more than a third of the length of the crown in the frontal region.
- The cutting edge of the lower incisors contacts the palatal cusps of the upper incisors.
- The upper first molar occludes the 2 lower molars, covering two-thirds of the first molar and one-third of the second.
- The buccal cusps of the lower teeth overlap the buccal cusps of the upper teeth in the transverse direction.
You can learn more about occlusion in dentistry in the book “Functional Occlusion” by Peter Dawson.
Signs
Distal occlusion pathology is identified before a dental examination based on the patient’s facial shape. The lower part of the face is shortened, and the upper jaw protrudes or is smoothed, depending on the form of the pathology. The mouth is usually slightly open, and the lower lip is located behind the upper incisors; there is a specific fold on the chin. Teeth are crowded and incorrectly aligned.
Distal bite photo.
Patients complain of difficulty biting and chewing food. Their incisors and premolars do not completely close. If the anomaly is severe, there may be problems with sound pronunciation and breathing.
Causes
Most often, occlusion develops as a result of embolism, blockage of a blood vessel by a dense formation. This process can develop as a result of:
- Infectious disease . In this case, the blood flow is blocked by inflammatory-purulent blood clots or the accumulation of a large number of pathogenic microorganisms.
- Air embolism . It develops as a result of an air bubble entering the systemic bloodstream. It is determined after traumatic damage to a vessel or after an incorrectly performed injection.
- Fat embolism . As a result of metabolic , fat particles accumulate and a fat clot forms from them.
- Arterial embolism . Thrombi form on the valve apparatus of the heart and are characterized by instability and mobility, which can lead to separation of thrombotic masses and blockage.
Occlusion of the vessels of the neck and coronary arteries is formed in the area of their branching or narrowing.
Causes of thrombosis:
- malignant neoplasms;
- atherosclerosis;
- traumatic injuries;
- aneurysms;
- thromboembolism.
As a result of traumatic damage to muscle tissue and the skeletal system, compression occurs and blood flow is blocked.
Treatment of distal bite
The approach to correction should be comprehensive. If malocclusion occurs due to adenoids or spinal curvature, these factors must be eliminated. Local impact on teeth will not produce results.
In a child under 6 years old, you can quickly get rid of a distal bite without irreversible consequences and complications. The effect can be assessed by looking at the photos before and after treatment. At preschool age, the anomaly of the facial skeleton has not yet had time to fully form, so with timely correction this problem can be avoided.
The result of correcting a distal bite.
Experienced orthodontists can successfully cope with the problem in a child under 12-13 years old with the help of special structures that stimulate jaw development. The following designs are used for this:
- Frenkel function regulator;
- bionator;
- trainer;
- open Klammt activator;
- myobrace;
- closed Heupl activator.
These removable structures are effective and do not harm health. They are most effective in combination with special gymnastics. Over time, the act of chewing is normalized, the development of the jaw that is lagging in growth is stimulated, and its shape changes. The use of braces to correct distal occlusion is less effective. In most cases, the problem is not caused by an abnormality in the teeth, but by an incorrect configuration of the bone structures. Therefore, you need to influence the problem area.
Is successful correction possible in adults?
Not all parents care about correcting the pathology in their child, so adults with distal occlusion often turn to orthodontists. Is it possible to help them? Yes, there are methods for correction in adults, but it is much more difficult to do this than in childhood. Surgical treatment is often used.
For minor problems, results can be achieved with braces. Changing the position of teeth allows you to achieve a good cosmetic effect and improve chewing function. With pronounced changes in the facial skeleton, only surgery will help. Often, surgical treatment and orthodontic appliances are used in combination.
The price of treatment depends on the chosen technique, and the effectiveness depends on the qualifications of the doctor and the characteristics of the patient.
Symptoms
Against the background of damage to the brachiocephalic vessels, there is a decrease in performance, weakness and dizziness . The brachiocephalic trunk is responsible for the blood supply to the soft tissues of the head and the brain. If the left artery is additionally involved in the pathological process, then the clinical picture worsens significantly. Main manifestations:
- pale skin;
- nausea;
- headache;
- pain during physical activity;
- confusion;
- paraplegia;
- swelling and development of necrosis;
- burning sensation or numbness;
- deterioration of visual perception;
- hallucinations;
- difficulty breathing, swallowing;
- speech disorders;
- cardiopalmus;
- absence of pulse in the affected area.
If any of the above symptoms appear, it is necessary to conduct a thorough analysis and diagnosis to identify the true cause and subsequently prevent the development of severe complications.
How to diagnose pathology?
To diagnose abnormal clamping of the CC pathways, a comprehensive neurological examination is performed. The most accessible technique is ultrasound screening of head and neck vascular tissues. The most informative method confirming the initial diagnosis is angiography of cerebral vessels. Angiography is used in difficult cases, as well as before instrumental intervention (for planned surgery).
Magnetic resonance angiography is as safe and informative as possible due to the inaccessibility of other diagnostic methods. Additionally, a referral is made for a nuclear resonance scan of the brain. With joint hardware diagnostics, damage to the carotid “traces” is 100% detected.
Computer scanning helps to identify areas affected by oxygen deprivation. Color differences in degenerative areas in the resulting images help differentiate different types of ischemia. This type of disease can be determined only after 2-3 days. In the first hours of ischemia development, changes in brain tissue are not visible. Destruction can be determined only by indirect signs.
Tests and diagnostics
It is recommended to consult a doctor at the first manifestations of the disease. After examination, collecting anamnesis and assessing the manifestations of clinical symptoms, they begin diagnostics, which includes:
- CT arteriography;
- Doppler ultrasound;
- cerebral angiography;
- MR angiography;
- coagulogram;
- MRI of the brain.
Only after a comprehensive examination is appropriate treatment prescribed, which is selected individually for each patient.
Course of the disease
Once atherosclerotic plaques appear, they will no longer be able to resolve, but only gradually progress. The rate of growth of an athersclerotic plaque depends on many risk factors, including cholesterol levels. All people over 50 years of age are recommended to undergo an annual ultrasound of the carotid arteries in order to exclude the development of atherosclerotic plaques and the risk of ischemic stroke.
With the development of complications of atherosclerosis of the carotid arteries, discirculatory encephalopathy quickly progresses. Frequent TIAs, and even more so ischemic stroke, contribute to the death of part of the brain tissue and disruption of brain function. Patients with atherosclerosis of the carotid arteries often develop vascular dementia (dementia).
After restoration of the patency of the carotid artery, the phenomena of cerebrovascular insufficiency are stopped, and the likelihood of repeated cerebrovascular accidents is significantly reduced.
Diet for occlusion
To restore the elasticity of the vascular wall, strengthen it and reduce the severity of occlusion, it is recommended to adhere to certain dietary rules. In case of occlusion, it is recommended to adhere to a special cholesterol-lowering diet, which includes:
- Legumes . Beans and legumes are sources of protein, iron, folic acid and contain absolutely no fatty acids.
- Whole grains (wheat bread, buckwheat, oatmeal and brown rice).
- Cabbage (all types, especially broccoli). Prevents salt deposition, normalizes the lipid spectrum of cholesterol, enriches the body with vitamins K and C.
- Asparagus . Helps lower blood pressure and reduce cholesterol in the blood.
- Persimmon . Rich in fiber and has a pronounced antioxidant effect.
- Spinach . Allows you to reduce blood pressure in hypertensive patients.
- Turmeric . It has an anti-atherosclerotic effect, reduces the volume of cholesterol plaques, and reduces the severity of the inflammatory process.
Risk factors for carotid atherosclerosis
Risk factors for carotid artery disease are similar to those for other types of cardiovascular disease. They include:
- Age
- Smoking
- Hypertension (high blood pressure) is the most important risk factor for stroke
- High cholesterol
- Diabetes
- Obesity
- Sedentary lifestyle
- Family history of atherosclerosis
Men under 75 years of age have a greater risk of developing carotid artery stenosis than women in the same age group. In the group over 75 years of age, women have a greater risk of stroke. In patients suffering from coronary artery disease, narrowing of the carotid artery is often detected.
List of sources
- Matyushenko A.A. “Pulmonary embolism as a general medical problem”, article in the journal RMZh No. 13 dated 07/03/1999
- Atayan A.A., Kosenkov A.N., Kuznetsov M.R., Chernookov A.I., Ivanova M.I., Khachatryan E.O. “Hybrid tactics in the treatment of acute disorders of mesenteric circulation”, RMZh No. 8(II) dated 10.25.2019
- Yavelov I.S. “The use of anticoagulants during thrombolytic therapy in patients with signs of acute occlusion of the coronary artery: how to individualize treatment?”, RMZh No. 26 of November 30, 2011