One of the most common reasons for visiting pediatric otolaryngologists is inflammation of the tonsils in a child, otherwise known as tonsillitis. Inflammation affects the palates; tonsils are paired lymph glands, often called tonsils. The cause of inflammation of the tonsils in children can be either a viral or bacterial (streptococcal and staphylococcal) infection.
Pediatric ENT doctors at the Miracle Doctor clinic comprehensively assess the child’s condition and develop individual treatment regimens. Experience and the latest equipment allow them to provide high-quality diagnostics and treatment of ENT organs of patients of all ages.
What are lacunae
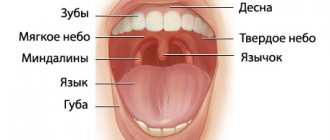
The tonsils are covered on the outside with a mucous membrane with depressions called lacunae. They protect the body from pathogens and ensure filtration of everything that enters the mouth.
In the follicles that make up the tonsils, lymphocytes mature and are released onto the surface of the lacunae to destroy microbes. In a healthy person, the lacunae cleanse themselves.
Surgery
If no conservative treatment methods lead to a lasting therapeutic effect, the doctor recommends surgical treatment: tonsillotomy or tonsillectomy.
The hospital practices both of these types of tonsil removal:
- tonsillotomy - partial removal of the tonsils in children aged 3-12 years while preserving the protective functions of the lymphoid tissue that make up the tonsils;
- Tonsillectomy - complete removal of the tonsils, is used when the tonsils are pathologically changed and are a source of chronic infection, or when complications arise from the organs, blood vessels, and joints of the body.
At the Yauza Clinical Hospital, all types of operations to remove tonsils are performed under anesthesia. In the process of tonsillectomy, a bipolar coagulator is used, which minimizes trauma to surrounding tissues and allows almost completely to avoid blood loss due to coagulation of the vessels feeding the tissue.
The Clinical Hospital on Yauza uses modern technology for tonsillectomy with suturing of the wound surface. The innovative tonsillectomy technique allows:
- minimize the risk of bleeding in the postoperative period;
- significantly speed up the postoperative healing period;
- reduce the rehabilitation period: hospital stay - up to a day; restoration of working capacity - after 7-10 days.
The cost of tonsillectomy is calculated for each patient separately and depends on the diagnostic examination, surgical method, and length of hospital stay.
At the Clinical Hospital on Yauza you are guaranteed:
- strict adherence to the treatment protocol;
- examination in a laboratory equipped with the latest advances in medical science;
- conservative treatment and tonsillectomy using the most effective technologies and using innovative equipment;
- stay in a comfortable room;
- constant supervision of experienced practitioners.
For any manifestations of tonsillitis, contact the Clinical Hospital on Yauza through the website by filling out the online appointment form.
You can see prices for services
Why is rinsing prescribed?
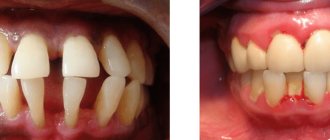
When immunity decreases, the production of lymphocytes decreases, and an inflammatory process begins in the lacunae. As a result of the disease, the ability to cleanse itself decreases and the recesses of the tonsils become clogged with purulent plugs.
The person’s health deteriorates and the following appears:
- heat,
- severe sore throat
- difficulty swallowing.
With frequent such manifestations, doctors diagnose chronic tonsillitis. And rinsing is prescribed to prevent the spread of infection to other organs.
This stops the exacerbation of tonsillitis and in some cases eliminates the need for surgical intervention to remove the tonsils. Washing is almost painless, as doctors use modern equipment to carry it out quickly.
Important! It is dangerous to clean lacunae on your own due to the risk of damaging the delicate mucous membrane of the palate and pharynx.
Complications
If inflammation of the tonsils becomes chronic, then exacerbations of the disease occur; 6-7 times a year. The presence of frequent exacerbations indicates a weakened immune response of the child’s body to the presence of infection in the tonsils. Inflammation of the tonsils often leads to the development of complications in the ears, lungs and other organs of the child. In the case of chronic inflammation, the tissue of the tonsils becomes scarred, lacunar plugs appear, and the lacunae themselves become foci for the spread of staphylococcal and streptococcal infections.
.
Types of washing
Purpose of appointment: to remove pus from the lacunae and treat them with a drug. After this, the patient's condition improves significantly.
Specialists carry out the procedure in different ways:
syringe. A solution is drawn into a 20-gram syringe. Instead of a needle, a special nozzle with a curved end is put on so that the solution falls directly on the stopper. The liquid under the pressure of the piston is fed into the lacuna and flushes it.
Washing the tonsils- Vacuum method of washing tonsils . The tonsils are anesthetized, a vacuum suction cup is attached to them, through which the purulent contents are pumped out. After this, the medicinal composition is pumped into the lacuna.
- Ultrasonic washing of tonsils . The cleaning principle is based on a combination of cavitation and ultrasound. Air bubbles form in the washing liquid, and when they rupture, the membranes of microbial cells are damaged.
The Kuntsevo Medical Center has modern otolaryngological equipment, which allows the operation to be performed as quickly, efficiently and painlessly as possible.
Reviews
Andrey
For most of my life I was tormented by constant exacerbations of chronic tonsillitis. Every spring and autumn I consistently lost two weeks for treatment. Surgery to remove tonsils has bothered me since childhood. My wife almost forcibly brought me to the clinic. I didn’t even imagine that new techniques can eliminate the problem absolutely painlessly. I have been living without constant exacerbations for a year now, and I am very grateful to the hospital specialists for this.
Natalia
Not long ago I had to bring my child to have his tonsils removed. From my own experience I remember how unpleasant and painful this procedure is. I was more worried than my son. However, the clinic doctors were able to find an approach to the child and calm him down. The operation was performed without pain or blood. Now I know for sure that your clinic employs super specialists and kind, sympathetic people.
How is the procedure performed?
All rinsing methods are based on exposing the tonsils to a stream of disinfecting solution or vacuum. Cleaned tonsils are treated with medications.
Processing each tonsil takes from 30 seconds to 1.5 minutes. The time depends on the choice of type of cleaning of the lacunae and the depth of damage to the lacunae.
Important! Before the procedure, you cannot eat for 1.5-2 hours. This is due to the fact that rinsing provokes a gag reflex.
To prevent possible discomfort, the doctor treats the tonsils with a local anesthetic with lidocaine or novocaine in the form of a spray.
Conservative therapy
Depending on the diagnostic results, the doctor draws up an individual treatment plan. Acute tonsillitis is treated by a therapist on an outpatient basis using conservative methods, using antibacterial drugs in the form of tablets, rinsing, washing, and irrigation of tonsil lacunae.
Therapy of chronic tonsillitis is the responsibility of an otolaryngologist, who acts together with an immunologist.
A good result in the treatment of the disease is achieved by affecting the tonsils themselves. The hospital's otolaryngologists conduct courses of medical manipulations, during which:
- caseous plugs are removed;
- The folds of the tonsils (lacunae), which hide foci of infection, are cleaned.
During the treatment process - washing, lubricating and irrigating the tonsils with medicinal solutions, inflammation is stopped, the compensatory stage of the disease is prolonged, which makes it possible to delay or avoid tonsillectomy. Additionally, complex treatment at home is prescribed.
Contraindications
Treatment of lacunae is not prescribed for patients with:
- exacerbation of other chronic diseases, including caries;
- cancer diagnoses;
- in the 1st and 3rd trimester of pregnancy;
- pathology of the retina;
- severe pathologies of the heart and blood vessels;
- up to 3 years of age.
For hypertension, consultation with a specialized specialist is required.
Important! It is necessary to warn the doctor about any existing individual intolerance to drugs.
Survey
In the department of otorhinolaryngology (ENT) of the hospital, patients with a chronic form of the disease are examined using:
- pharyngoscopy (visual method);
- PCR diagnostics - a high-precision method of molecular genetic diagnosis of infectious diseases;
- bacteriological tests - diagnosis of the main agent of infection and its sensitivity to antibiotics;
- antigen tests - diagnosis of immune system activity;
- general blood tests.
Recommendations after procedures
Rinsing the lacunae of the tonsils is a physical effect on the inflamed tissue, so after cleansing, discomfort and mild pain are possible.
You cannot eat immediately after the procedure, the first meal should not be earlier than 30 minutes later. It is necessary to regularly gargle with miramistin, furatsilin solution, infusion of chamomile, oak bark.
Washing the tonsils is not a very pleasant procedure, but it is done quickly. Its effectiveness has been proven by many years of use for the relief of chronic tonsillitis.
How to treat inflamed tonsils?
The presence of a simple sore throat is not an indication for tonsil removal! There are many treatment methods that avoid invasive intervention:
- Antibiotics. It would not be amiss to remind you that the course of antibiotics must be taken completely in accordance with the doctor’s recommendations, without skipping a single dose of medication and without abandoning treatment at any stage.
- Washing with various agents with an antibacterial effect. You may even be prescribed a simple solution of chlorhexidine, which will definitely not cause harm, but may well be a good medicine.
- Application of special solutions. This could be Lugol's solution or propolis - the doctor prescribes one or the other based on your individual characteristics.
- Physiotherapy. Ultrasound, magnets, electrophoresis - all this can be a completely sufficient method of treatment without any surgery.
- Maintaining a healthy lifestyle, strengthening the immune system and avoiding hypothermia, although not a treatment method, is an excellent method of preventive intervention in the development of severe pathologies.
You can also read our article on the treatment of chronic tonsillitis.
Results and discussion
The peripheral zone of adenoid vegetations in patients of the 1st group practically does not contain connective tissue and is characterized by a pronounced and full-blooded microvasculature, the boundaries of large rounded lobules are poorly distinguishable.
The peripheral zone in patients of group 2 consists of lobules of predominantly small size (about 2 times smaller than in group 1), separated by connective tissue septa with many small full-blooded vessels, especially veins and venules. Such sclerotic septa distinguish this group from observations in group 1. The microvasculature network is still pronounced, but individual arterioles and capillaries are sclerotic and hyalinized.
The middle zone in patients of group 1 is distinguished by a large number of small full-blooded vessels, thanks to the linear accumulations of which the boundaries of the lobules of lymphoid tissue are visualized. Connective tissue layers are not expressed. Sclerosis of the layers and walls of blood vessels is not determined.
In patients of group 2, the middle zone is distinguished by its large size, clear interlobular boundaries with sclerosis and clusters of full-blooded, sclerotic vessels.
The basal zone in patients of the 1st group is represented by loose connective tissue with many small vessels with an expanded lumen, in some cases with initial signs of sclerosis of their walls. In the stroma of the basal part there is a diffuse lymphoid infiltrate that does not form any structures.
In the 2nd group of patients, significant changes in the basal zone were revealed, in light of the prognosis of intraoperative hemorrhage. There is an increase in stromal sclerosis, sclerosis and hyalinosis of the walls of vessels of various sizes, mainly veins with cavernous expansion of the lumen and rigid walls. In the sclerotic stroma there is a diffuse lymphoid infiltrate, which forms extensive accumulations at the resection edge, spreading into the underlying connective tissue layer (Fig. 1, a, b on the color insert).
Rice. 1. Patient N., 18 years old (group 2). Lymphoid tissue, basal zone. a: 1 - stromal sclerosis, 2 - pronounced sclerosis of the walls of microvasculature vessels, dilated venules and small veins; b: 1 – sclerosis and hyalinosis of the walls of vessels of different calibers, mainly veins with a cavernous dilated lumen. Hematoxylin and eosin staining. Uv. 400.
Patients of the 2nd group at the edge of resection of adenoid tissue are characterized by the accumulation of many cavernous dilated venous vessels with sclerotic walls and the phenomenon of “immersion” of lymphoid tissue deep into the sclerotic connective tissue layer of the adenoids with a well-developed microvasculature. This phenomenon is confirmed by histological examination of the underlying tissues after adenotomy. Lymphoid tissue is represented by both B-dependent zones (lymphoid follicles with large active light centers) and T-dependent zones (Fig. 2 on color insert).
Rice. 2. Patient K., 18 years old (2nd group). Biopsy from the underlying tissues after adenotomy. The phenomenon of “immersion” of lymphoid tissue deep into the connective tissue layer of the adenoids. 1 - cavernous dilated veins with rigid sclerotic walls. Lymphoid tissue is represented by both B-zones - lymphoid follicles with large active light centers (2) and T-zones (3). Hematoxylin and eosin staining. Uv. 100.
conclusions
1. The vessels of adenoid vegetations have clear age-related characteristics, which are most clearly manifested from the age of 18 and are characterized by the development of sclerosis and hyalinosis with the formation of cavernous dilated full-blooded veins with thickened rigid walls.
2. In patients over 18 years of age, there is a morphological restructuring of the connective tissue (basal) layer, namely the newly discovered phenomenon of “immersion” of lymphoid tissue with a well-developed microvasculature, which may increase the risk of intraoperative bleeding during adenotomy in this age group.
The authors declare no conflict of interest.