Enlarged tonsils in a child may indicate that the body is fighting some kind of infectious carrier, or some other pathologies. With this symptom, it is necessary to treat the underlying pathology in the body.
Author:
- Oganesyan Tigran Sergeevich
ENT pathology expert
4.10 (Votes: 10)
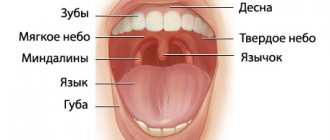
Tonsils (tonsils) are a collection of lymphoepithelial tissue, which is the point of contact of the immune system with the external environment. Thanks to this, the body produces protective immunoglobulin proteins in response to bacteria, viruses, fungi and other foreign microorganisms. Thus, the formation and maturation of immunity occurs. Located at the border of the respiratory and digestive tracts, the tonsils promptly intercept viruses and bacteria that enter the body with inhaled air, water and food.
Enlarged tonsils in a child are not a separate disease. They say:
- that the body is fighting some kind of infectious carrier;
- about genetically determined proliferation of lymphoepithelial tissue without an infectious agent;
- about possible blood diseases (oncohematological diseases), autoimmune diseases and diseases of the endocrine system.
The problem is that tonsil hypertrophy progresses quickly, and it is important not to miss the moment when the painful condition begins to cause severe discomfort to the child, but to treat the underlying pathology in a timely manner. Only an experienced doctor, whose specialization is children's ENT diseases, can correctly determine the true factor in the appearance of the symptom and choose competent therapy to eliminate it.
When should you see a doctor?
Even slightly enlarged tonsils in a child are a signal to contact a pediatric otolaryngologist. However, mild hypertrophy of the glands often does not manifest itself in any way, so it cannot be noticed visually. A visit to the doctor is required if the child, in addition to enlarged tonsils, has:
- classic signs of a cold: pain when swallowing, redness of the throat, cough, nasal congestion, fever, uncharacteristic weakness, headache;
- white plaque on the tonsils;
- swollen lymph nodes;
- pustules, ulcers in the larynx;
- swelling of the neck.
Diagnosis of the disease
Diagnosis of acute laryngitis is not particularly difficult. The diagnosis is based on the presence of acute respiratory infections symptoms, as well as hoarseness, shortness of breath, and barking cough. Call a doctor: he will listen to complaints, examine the child, measure the temperature, listen to the lungs and make a diagnosis.
Causes of enlarged tonsils in children
The increase is caused by the following infectious agents: pneumococci, staphylococci, herpes, streptococci, chlamydia, Haemophilus influenzae, adenovirus, influenza virus. They can be located in the lacunae of the tonsils without manifesting themselves in any way (for example, remain after treatment for a disease), but at a favorable moment they begin to actively multiply and cause an enlargement of the organ. Such triggers can be:
- decreased immunity;
- allergies;
- bad ecology;
- hormonal disorders;
- severe hypothermia;
- lack of vitamins;
- infections.
Mechanism of disease development
Acute laryngitis is an inflammation of the mucous membrane of the larynx. The larynx is located in the front region of the neck. It connects the pharynx to the trachea and performs three vital functions:
- sound-producing (the vocal apparatus is located in it);
- respiratory;
- protective (prevents food and foreign particles from entering the trachea).
Under the influence of a number of factors (hypothermia, overstrain of the vocal cords, allergies, infectious diseases, etc.), the mucous membrane of the child’s larynx becomes inflamed. As a result, a sharp dilation of blood vessels occurs, edema develops, the lumen of the glottis narrows (or completely closes), speech function is impaired and breathing becomes difficult.
The degree of enlargement of the tonsils in a child
There are 4 stages of hypertrophy of the glands:
- At the first stage, the inflamed tissue of the tonsils covers no more than 30% of the lumen between the pharynx and the sky. In this state, it causes almost no discomfort, so it is difficult to detect at this stage.
- At the second stage, hypertrophied tissue covers half of the lumen. The child begins to have difficulty swallowing and breathing freely, and a sensation of a foreign body in the throat.
- At the third stage, there is severe difficulty in breathing and swallowing.
- On the fourth, the pharynx is almost completely blocked by inflamed tonsil tissue. It is difficult to bring the condition to this stage, since already at the third stage the child’s well-being requires immediate medical attention.
Causes
Primary pharyngitis is associated with exposure to the pharyngeal mucosa of infectious agents. The disease can be provoked by intestinal and general infections, inflammation of the upper respiratory tract. In some cases, the cause is burns of the throat mucosa, foreign objects in the throat, or damage to the throat during surgery. The most common causative agents of pharyngitis are the following pathogenic microorganisms:
- influenza viruses, herpes, parainfluenza, cytomegalovirus, enteroviruses, adenoviruses, rhinoviruses;
- bacteria such as staphylococci, meningococci, streptococci, Haemophilus influenzae and diphtheria bacillus, corynebacteria, moraxella, diplococci;
- fungi, intracellular agents (chlamydia, mycoplasma).
Pharyngitis of viral etiology is observed in 70% of cases, bacterial and other ones account for 30%. Its acute form is associated with pathologies such as infectious mononucleosis, measles, scarlet fever, and ARVI. The chronic type of pharyngitis is more often diagnosed in patients with the following inflammatory diseases of the oropharynx:
- adenoiditis;
- sinusitis;
- stomatitis;
- rhinitis;
- chronic tonsillitis;
- sore throat;
- caries.
Risk factors for the development of pharyngitis include local or general hypothermia. There is a high probability of inflammation of the pharyngeal mucosa as a result of exposure to spicy food, tobacco smoke, dusty or cold air. Patients who have the following are also at risk:
- weakening of local immunity;
- removal of the palatine tonsils, after which atrophic changes in the pharyngeal mucosa are observed;
- gastroesophageal reflux, which causes stomach contents to flow into the throat;
- posterior rhinitis, in which mucus flows down the throat when blowing the nose;
- difficulty breathing through the nose, causing unpurified cold air to be inhaled through the mouth;
- allergies due to histamine reaching the mucous membrane of the throat.
Types and forms
Bacteria and viruses enter the mucous membrane of the pharynx from other areas of inflammation. For this reason, pharyngobronchitis, pharyngolaryngitis, nasopharyngitis and pharyngotonsillitis in children are diagnosed more often than the isolated form of pharyngitis. Depending on the nature of the course, the disease can be of the following types:
- Spicy. Inflammation continues for 2 weeks. The symptoms of the disease are pronounced. Pain and sore throat and dry cough are more common. The cause may be infectious and inflammatory processes in the trachea or nasopharynx.
- Chronic. It lasts for more than six months with frequent exacerbations.
Taking into account the area of inflammation, the disease is divided into 2 more types: widespread - the entire back surface of the pharynx is affected, limited - inflammation is observed only on the lateral ridges. Depending on the location, chronic pharyngitis in children can be presented in the following forms:
- catarrhal (only the mucous membrane of the throat is affected);
- granulosa (inflammation is located deeper in the lymphoid follicles);
- atrophic (accompanied by drying out of inflamed tissues).
Symptoms
Pharyngitis in a child is accompanied by pain when swallowing, dryness, rawness and sore throat. Against this background, a shallow cough is observed, and hoarseness appears. When examining the throat, the following signs can be noted:
- redness of the wall of the pharynx, soft palate and velopharyngeal arches;
- a granular throat in a child with protruding, inflamed follicles;
- hyperemia and swelling of the uvula, lateral ridges of the pharynx.
The temperature of a child with pharyngitis can be normal or low-grade (37 degrees). It rises higher if the disease develops against the background of viral diseases. Then the little patient experiences fever, headache and swelling of the submandibular lymph nodes. The following symptoms indicate a chronic course of the disease:
- obsessive cough;
- sensation of a foreign body in the throat;
- loose mucous membrane of the throat.
Depending on the form and nature of the disease, very different, subjective symptoms may be observed. The main ones are the following:
- With a fungal form (pharyngomycosis). There are erosions and cracks in the corners of the mouth (jams), a cheesy coating on the back wall of the pharynx, and enlarged lymph nodes in the neck.
- In the atrophic form. Thinning, pallor and dryness of the mucous membrane of the throat are diagnosed. It contains hard-to-remove dried crusts.
- In chronic hyperplastic form. The child may complain of a dry and sore throat. Thick mucus accumulates on the pharyngeal mucosa, which can cause vomiting. Against this background, hyperplasia of the throat epithelium can be noted.
Acute pharyngitis
It has a clear clinical picture. The child complains that it hurts to swallow, itching, dryness and sore throat. The increase in temperature is insignificant - up to 37-38 degrees. If the illness occurs against the background of a cold, then all its characteristic symptoms will appear, including cough, runny nose, and conjunctivitis. With an “empty throat”, the pain in the throat intensifies - this is a characteristic symptom.
In children, hypertrophied inflammation of the pharyngeal mucosa is observed. Large and medium-sized granulations form on it, which cause pain. Characteristic symptoms of the acute form are the following:
- child's refusal to eat;
- irradiation of pain in the ear and lower jaw;
- pinpoint hemorrhages in the hard palate;
- pain and enlargement of regional nodes;
- drowsiness, apathy.
Chronic
A distinctive sign of the chronic form of the disease is a false cough, in which sputum is not produced. It is celebrated mainly at night. Mucus accumulates on the back wall of the throat, which the child constantly swallows reflexively. When examining the throat, you may notice its redness and graininess. Purulent plaque is observed only with a bacterial etiology of the disease. Other distinctive features are presented in the list:
- slight increase in temperature in the morning;
- dry throat, which causes you to constantly swallow;
- hoarseness of voice;
- feeling of stuffiness in the upper part of the throat;
- malaise.
Pharyngitis in infants
The disease is much more severe in infants. Since they cannot say what bothers them, the parents themselves have to identify the disease. In infants, general symptoms predominate, expressed by signs from the following list:
- poor sleep, anxiety;
- periodic coughing;
- tearfulness and moodiness;
- temperature 39 degrees;
- regurgitation after feeding;
- loss of appetite;
- salivation - salivation;
- dysphagia – a disorder of swallowing;
- severe fever;
- rash on the body;
- dyspepsia;
- runny nose.
Complications
Most complications of the disease occur due to improper treatment. The infection spreads throughout the body, primarily affecting the respiratory tract, although inflammation can also affect the membranes of the brain. The list of complications of pharyngitis includes the following serious diseases: Otitis, Tonsillitis, Sinusitis, Rhinitis, Conjunctivitis, Meningitis.
Treatment of pharyngitis in children
Treatment of this disease in childhood is often limited to local treatment. It consists of inhalation and rinsing. Young children who cannot rinse their mouths are recommended to drink plenty of fluids and drip irrigation of the mucous membranes with antiseptics. If the child already knows how to dissolve tablets, then he is prescribed lozenges with analgesic, antibacterial and softening effects.
To prevent pharyngitis from getting worse in children, it is necessary to take measures to treat the underlying disease: caries, tonsils, adenoids, intestinal dysbiosis, colds, rhinitis, sinusitis, etc. Taking into account the etiology of inflammation of the pharyngeal mucosa, systemic therapy with the following drugs is prescribed:
- antibiotics - for bacterial infections;
- antiviral – for viral infections;
- antimycotics – for fungal infections;
- antihistamines - for allergies.
Antibacterial agents can also be used topically, for example, such as Bioparox, Grammidin or Orasept. Regardless of the chosen regimen, treatment should be aimed at achieving the following goals:
- normalization of temperature - it is recommended to take antipyretic drugs, for example, children's Paracetamol or Cefecol;
- reduction of pain and discomfort in the throat - inhalations, rinsing, warm, generous drinks are indicated;
- ensuring complete rest - bed rest is prescribed;
- elimination of nasal congestion - it is necessary to instill vasoconstrictor drops into the nostrils;
- strengthening the immune system - for this purpose, Grippferon or Derinat is instilled into the nose.
Treatment of pharyngitis in children at home
If the child has no complications or high fever, the doctor may allow treatment at home. An important criterion for recovery in this case is compliance with bed rest during the acute period - until the temperature drops to normal values. Parents must follow the following rules:
- give the baby only warm food;
- exclude spicy foods that irritate the throat mucosa;
- regularly ventilate the patient’s room;
- carry out wet cleaning and humidify the air daily;
- limit the patient's vocal load.
You can give drink not only warm water, but also milk with honey or soda. If the temperature has subsided, then hot foot baths are allowed. To gargle, use decoctions of chamomile, oak bark, and calendula.
To eliminate unpleasant symptoms in the throat, inhalations are indicated. It is better to carry them out using a nebulizer. The recommended frequency of the procedure is 1-4 times per day. Borjomi mineral water, Furacilin solution or saline solution are suitable for inhalation. The latter can be diluted with tincture of calendula or propolis in a ratio of 20:1.
Prevention
An important condition for the prevention of this disease in childhood is routine vaccination. Maintaining proper nutrition and taking vitamins will help prevent any inflammation of the respiratory tract. The child needs to be provided with regular daily exposure to fresh air. The list of preventive measures includes the following:
- hardening;
- limiting contact with sick people;
- ventilation of the home and regular wet cleaning;
- promptly treat colds, rhinitis, sinusitis, adenoiditis;
- Avoid child contact with tobacco smoke and dust.
Bibliography:
Diseases of the ear, nose and throat Luchikhin L.A. /2010
Pediatric otorhinolaryngology. Volume 1, Chistyakova V.R./2005
All about ENT diseases. Pechkareva A.V./2013
Otorhinolaryngologist L.V. Ledova
How is inflammation treated?
The tactics for treating enlarged tonsils in a child consists of treating the underlying disease that caused this symptom (taking antibiotics, antiviral or antifungal drugs), and influencing them directly to regenerate the affected tissues. The latter includes:
- washing the tonsils from pathogenic microorganisms and mucus with antiseptic solutions;
- reducing swelling - taking antihistamines and ultraviolet irradiation;
- UHF therapy, which improves blood microcirculation;
- exposure to ultrasound to free the lacunae of the tonsils from pus, which can accumulate in them;
- laser exposure to destroy infection and its pathogens.
How to treat chronic tonsillitis?
In this case, treatment should only take place under the supervision of a doctor. Its necessity is due to the fact that tonsillitis depletes the child’s immunity, and if treatment is not completed, it can worsen and lead to various kinds of complications: kidney disease, heart pathology, bronchitis, psoriasis, and diseases of other ENT organs.
Several ENT treatment options are possible; the doctor will determine the appropriate one after examining the child. In some cases, you will need to take a general analysis of ESR - erythrocyte sedimentation rate, which will allow you to identify the infection even in a latent form and begin treatment immediately.
To cure chronic tonsillitis, one of 2 treatment options is used: conservative or surgical.
The first involves taking antibacterial, antiviral, and antihistamine drugs. Local antiseptics and homeopathy and physiotherapeutic procedures (UVR, electrophoresis) are also prescribed.
Indications for surgery are frequent sore throats, purulent inflammations, lesions of other organs that arise against the background of tonsillitis. If based on all the symptoms you believe that your child has this disease, contact a specialist. The medical office is attended by an experienced doctor who diagnoses the disease and prescribes effective treatment, and gives recommendations for the prevention of chronic tonsillitis. The clinic also offers tests for children and adults and receives quick results by email. To make an appointment, use the convenient form on the website or the hotline number
Causes and routes of infection
The very name of the disease already makes it clear that the source of infection is a variety of viruses. These can be herpes viruses, influenza, Coxsackie viruses, ECHO viruses, adenoviruses, enteroviruses and others. Therefore, the disease is conventionally divided into adenoviral, influenza and herpetic.
The disease is highly contagious: you can become infected during a conversation, by sneezing, through dishes, toys, and food. Viruses that enter the body reach the surface of the tonsils and settle there. From the moment of infection, the patient remains a source of infection for another 30 days. Many factors increase the likelihood of developing the disease:
- cold season;
- improper and unbalanced diet;
- lack of personal hygiene;
- hypothermia (for example, caught in the rain, eaten cold ice cream);
- smoking in front of a child;
- bad ecology;
- climate change;
- weak immunity;
- the presence of a chronic source of infection in the body (for example, chronic tonsillitis);
- carious teeth;
- allergic reactions;
- tuberculosis, diabetes and other diseases;
- stressful situations.
Sore throats caused by influenza viruses or adenoviruses usually occur during the cold season, especially during outbreaks of epidemics, when the body's defenses weaken. Herpetic sore throats are more common in the summer. In order to understand in time that we are dealing with viral tonsillitis, it is necessary to be able to distinguish the main symptoms of the disease in a child.
Principles of treatment
The disease does not require hospitalization. All events are held at home.
Scarlet fever in children: how to treat a contagious disease:
- antibiotics (penicillin group) for a course of 10 days;
- antitoxic serum;
- gargling with a solution of furatsilin, a decoction of chamomile, calendula, eucalyptus;
- in case of dehydration - intravenous infusion of saline preparations;
- symptomatic therapy – antipyretics, non-steroidal anti-inflammatory drugs;
- gentle diet, bed rest.
The modern approach to the treatment of streptococcal infections guarantees a favorable outcome without serious consequences. Re-infection is diagnosed in 1-3% of patients.