Child's nose, nasal mucosa in children
The nose of a young child is relatively small, the nasal passages are narrow, and the lower nasal passage is absent. The nasal mucosa is delicate, relatively dry, and rich in blood vessels. Due to the narrowness of the nasal passages and the abundant blood supply to their mucous membrane, even minor inflammation causes difficulty breathing through the nose in young children. Breathing through the mouth is impossible in children in the first six months of life, since the large tongue pushes back the epiglottis. The exit from the nose, the choanae, is especially narrow in young children, which is often the cause of long-term disruption of nasal breathing in them.
Paranasal sinuses in children
The paranasal sinuses in young children are very poorly developed or completely absent. As the facial bones (upper jaw) increase in size and teeth erupt, the length and width of the nasal passages and the volume of the paranasal sinuses increase. By the age of 2 years, the frontal sinus appears, and the maxillary cavity increases in volume. By the age of 4, the lower nasal passage appears. These features explain the rarity of diseases such as sinusitis, frontal sinusitis, ethmoiditis in early childhood. Consultations with a pediatric ENT specialist at the Markushka clinic.
Chronic tonsillitis
Your child is undergoing surgery. We would like to give you and your child information about the need for this intervention. We make sure that you do not feel helpless in this situation. We would like to acquaint you with the essential aspects of the operation itself, and the risk factors in case of its failure. The written information provided to you serves this purpose. Read it carefully to discuss any unclear points with your doctor.
Every healthy child has lymphoid tissue in the pharynx, which is united into the so-called lymphadenoid pharyngeal ring. It includes the palatine tonsils - “tonsils” - they can be seen when examining the mouth - they look like balls protruding on the sides of the tongue, the pharyngeal tonsil - it cannot be seen during a direct examination of the oral cavity, it hides in the nasopharynx, behind the palate, lingual tonsil - located at the root of the tongue, and many lymphoid follicles scattered along the back wall of the pharynx, at the entrance to the larynx (see Fig. 18). These formations help the child defeat pathogenic bacteria that enter the throat during breathing and eating, and contribute to the formation of local immunity - protection against pathogens. By the way, in these organs there are no cells that affect the sexual development of the child, they do not produce sex hormones, therefore their diseases do not affect the sexual development of the child, and if they are removed if necessary (more on this later), sexual development is not disrupted.
In early childhood - usually from 2 to 5-7 years - the described organs work very hard, as the child expands the scope of contacts with peers by attending kindergarten, and inevitably often becomes infected and develops respiratory diseases. Moreover, if the child’s immune forces are not strong enough due to congenital characteristics, environmental factors and other reasons, the lymphoid organs increase in volume. This enlargement of the palatine tonsils is called “hypertrophy of the palatine tonsils”; they can become inflamed - inflammation of the tonsils is called tonsillitis. Tonsillitis can be acute or chronic. In children, chronic tonsillitis and adenoids - an enlarged pharyngeal tonsil - are often combined.
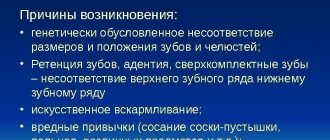
The tonsils of the pharynx have a significant impact on the state of health and the development of nearby organs. What kind of influence is this? A noticeable obstruction to the passage of air through the nose leads to breathing through the mouth. The consequence is obvious - untreated air enters the respiratory tract - not purified, not warmed and not humidified. A chronic inflammatory process, constantly smoldering in the tissue of the tonsils and adenoids, periodically exacerbating, contributes to protracted, recurrent diseases of the trachea and bronchi (bronchitis, obstructive bronchitis, tracheitis, pharyngitis), can independently cause or aggravate the course of allergies, in severe cases manifested in the form of bronchial asthma , allergic rhinopathy, atopic dermatitis. Adenoids and enlarged palatine tonsils, filling the pharynx, impair the functioning of the auditory tubes, which cannot supply sufficient air to the middle ear, as a result of which secretory otitis media develops, which can lead to hearing loss, and if infection enters the ear, to its acute inflammation – acute purulent otitis media. Poor breathing through the nose contributes to improper development of the maxillofacial area - the bite of the teeth is disrupted, the shape of the face changes (the so-called “adenoid face”).
The causative agents of infectious diseases of the respiratory tract (most often streptococci) after a sore throat remain in the palatine tonsils, and their chronic inflammation develops - chronic tonsillitis. Under unfavorable circumstances (hypothermia, stress, viral infection), the process in the tonsils is activated. This occurs in the form of another sore throat with plaque on the tonsils or purulent plugs. What is very dangerous is that each exacerbation of tonsillitis can cause complications in the form of diseases of other organs and systems of the child’s body, most often rheumatic diseases of the heart and joints, kidney diseases (pyelitis, pyelonephritis, glomerulonephritis). In addition, exacerbation of tonsillitis or tonsillitis sometimes causes complications in the form of an abscess (ulcer) in the pharynx. This complication is called peritonsillar abscess. A peritonsillar abscess indicates that the palatine tonsil is unable to cope with its function; it can recur at any time.
What factors contribute to enlargement of the pharyngeal tonsils and the development of chronic tonsillitis?
- Heredity - at least if the parents suffered from adenoids or tonsillitis, the child, to one degree or another, will also face this problem.
- Inflammatory diseases of the nose, throat, pharynx - and respiratory viral infections, and measles, and whooping cough, and scarlet fever, and tonsillitis, etc.
- Eating disorders - especially overfeeding.
- Tendency to allergic reactions, congenital and acquired immunity deficiency.
- Violations of the optimal properties of the air that the child breathes - very warm, very dry, a lot of dust, an admixture of harmful substances (ecological conditions, excess household chemicals).
- Inadequate (incorrect) treatment of acute tonsillitis (tonsillitis). The most common mistakes are an incomplete course of antibiotic treatment, incorrect dosing, violation of the therapeutic and protective regime (early getting out of bed, walking outside before 7-10 days from the start of treatment).
Thus, the actions of parents aimed at preventing chronic tonsillitis come down to correction, and even better, to the initial organization of a lifestyle that promotes the normal functioning of the immune system - feeding according to appetite, physical activity, hardening, limiting contact with dust and household chemicals.
What is the difference between chronic tonsillitis and tonsil hypertrophy?
Hypertrophy of the tonsils is an increase in their size in the age of a child up to 9-10 years. With chronic tonsillitis, the tonsils can be of any size; its distinctive feature is the development of a chronic inflammatory process in the tonsils.
What if a child, along with chronic tonsillitis or enlarged tonsils, has adenoids?
The presence of adenoids and difficulty in nasal breathing significantly influence the development of tonsil disease. In this case, otolaryngologists suggest that in the case of a compensated form of tonsillitis, while preserving the palatine tonsils, it is necessary to remove the adenoids, and in the case of a decompensated form, include adenotomy in the scope of the operation to remove the palatine tonsils, which slightly lengthens the operation and is almost imperceptible to the patient, but greatly affects the result of the operation. If this is not done, the child has a high probability of progression of tonsillitis or adenoiditis, which will negate the results of tonsillectomy - difficult nasal breathing will persist, the child will again become ill often, snoring will not go away or will worsen.
When is tonsillitis treated and when is surgery performed?
There are two forms of chronic tonsillitis: compensated and decompensated. In the decompensated form, surgical treatment is not possible - the tonsils must be removed. This diagnosis is made when tonsillitis often worsens (2-3 sore throats per year), the process extends beyond the tonsils, if diseases of distant organs and systems develop, for example, nephritis, rheumatic diseases of the heart and joints. Tonsils must be removed if a peritonsillar abscess develops.
Is it possible and necessary to treat chronic tonsillitis?
Let us emphasize that treatment is not only possible, but also necessary. Until the child develops the changes mentioned earlier, every six months, local treatment should be carried out in the form of irrigation of the pharyngeal mucosa with aqueous solutions that have anti-inflammatory, antiallergic and antimicrobial properties, as well as general treatment methods, including vitamin preparations, agents that affect immune system, locally acting vaccine preparations, physiotherapeutic methods (magnetic and laser therapy, inhalations). Otolaryngologists consider it particularly important in the treatment of tonsillitis to conduct a course of washing the lacunae of the palatine tonsils (7-10 procedures per course of treatment).
How urgently should the operation be performed?
The operation to remove the tonsils - tonsillectomy - is planned, that is, it is performed when the child is in full health or in remission of chronic diseases. It cannot be performed during acute illnesses (ARI) and 3-4 weeks after recovery. Thus, it is always possible to perform this operation in a period favorable for the child, which will minimize the risk of postoperative complications.
Do palatine tonsils grow again, are relapses possible?
No, completely removed tonsils cannot grow back.
How are tonsils removed?
This operation is performed using local or general anesthesia (narcosis). It lasts 25-30 minutes and, with proper psychological preparation of the child, is tolerated satisfactorily. The simplicity of the operation does not indicate its safety. Complications due to anesthesia, bleeding, and damage to the palate are also possible. But all this does not happen often.
Surgeons have long abandoned the removal of tonsils using ultrasound and laser due to the huge risk of complications.
How long does a child stay in the hospital after surgery?
Due to the high risk of bleeding in the postoperative period, the child is in the hospital for 6 days after surgery.
What should you do after your baby is discharged?
The child is discharged from the hospital under the supervision of an ENT doctor or pediatrician at the clinic at the place of residence. Home treatment is usually recommended for 1-2 weeks. In this case, physical activity should be limited, however, there is no need to keep the child in bed. When eating during the first days, you should not eat hot, spicy foods, sour juices and fruits, carbonated drinks, or ice cream. After 5-7 days, the diet becomes normal. 10-14 days after discharge, if the child’s general condition is satisfactory, there is no elevated body temperature, and the wound in the pharynx is healing smoothly, you can visit the children’s group and go outside. You can’t just do sports or go to the pool. The wound in the pharynx heals completely in 3-4 weeks. A month after the operation, there are no restrictions in lifestyle or diet.
How to remove tonsils at the Children's City ENT Center?
To establish a diagnosis, if there is no ENT doctor in the clinic, you can make an appointment at the city ENT consultation office by calling 2-78-49-00 (inquiry).
Reception is carried out on weekdays, from 8.00. until 20.00.
If the diagnosis of “chronic tonsillitis” has been established and you have made the decision to operate on your child, with a referral for surgical treatment issued at the clinic, you should go to the emergency department of the 3rd Children’s Clinical Hospital at any time convenient for you. Your child will be registered for hospitalization on the day you choose and will be given an examination plan (a list of tests necessary to perform the operation). Hospitalization is carried out on Tuesday and Thursday, from 13.00. until 15.00. and on Sunday from 16.00. until 18.00. The operation is carried out the next day.
In young children, the inhaled air is poorly warmed
Due to the insufficient development of cavernous tissue in young children, the inhaled air is poorly warmed up; therefore, children should not be taken outside at temperatures below -10 degrees. C. Cavernous tissue develops well by the age of 8-9 years, this explains the relative rarity of nosebleeds in children of the 1st year of life. A wide nasolacrimal duct with underdeveloped valves contributes to the transfer of inflammation from the nose to the mucous membrane of the eyes (examination by a pediatric ophthalmologist at the Markushka clinic). Passing through the nose, atmospheric air is warmed, moistened and purified. Every 10 minutes, a new layer of mucus passes through the nasopharynx, which contains bactericidal substances (lysozyme, complement, etc.), secretory immunoglobulin A.
The functions of the tonsils and their appearance are normal
Before diagnosing throat diseases, it is necessary to familiarize yourself with general information about the functions and appearance of the tonsils. These formations are accumulations of lymphoid tissue and are often called tonsils.
- Red throat in a child: how to treat it at home if it constantly hurts and hurts to swallow?
Tonsils perform two main functions: protective and hematopoietic. They produce antibodies that fight pathogenic microorganisms, preventing them from entering the body. The tonsils also form lymphocytes - cells of the immune system.
A healthy person has 4 tonsils: 2 paired and 2 unpaired, they are located at the junction of the nasopharynx and pharynx. Normally, these formations are the size of a walnut and are colored light pink. Also signs of normal tonsils include:
- absence of redness and plaque;
- the mucous membrane is not inflamed, there is no pronounced vascular pattern;
- the tonsils do not come into contact with the palatine arches and do not extend beyond them;
- When pressing on the tonsils with a medical spatula, no pus or mucus is released.
The combination of all these signs indicates a person’s health. However, for some people, increased size of the tonsils is the norm - this is an individual characteristic of the body.
Tonsils, adenoids in a child, children
By the age of 4-10 years, the tonsils are already well developed, and their hypertrophy can easily occur. During puberty, the tonsils begin to undergo reverse development.
The tonsils are like a filter for microbes, but with frequent inflammatory processes, a focus of chronic infection can form in them, causing general intoxication and sensitization of the body.
The proliferation of adenoids (nasopharyngeal tonsil) is most pronounced in children with constitutional abnormalities, in particular with lymphatic-hypoplastic diathesis. If the adenoids are significantly enlarged (degree 1.5-2), they are removed, since nasal breathing is impaired in children (children breathe with an open mouth - the air is not purified and warmed through the nose, and therefore they often suffer from colds), the shape of the face changes (adenoid face), children become distracted (mouth breathing distracts attention), and their academic performance deteriorates. When breathing through the mouth, posture is also disturbed; adenoids contribute to the formation of malocclusion. Treatment of adenoids - homeopathic pediatrician, Markushka clinic.
Treatment of tonsillitis
The methods of therapy directly depend on the nature of the infection and the form of the disease.
So, for bacterial tonsillitis, the patient is prescribed a course of antibiotics, for the viral form of the disease - anti-inflammatory drugs, for fungal - antifungal drugs. The name and dosage of the drug is selected exclusively by the doctor. Excessive independence of parents can lead to irreversible consequences. To eliminate the unpleasant symptoms accompanying tonsillitis, the patient may be prescribed the following medications:
- antipyretic drugs in the form of syrup, tablets or suppositories;
- rinsing with antiseptic solutions;
- local anesthetic and anti-inflammatory sprays, lozenges;
- washing the lacunae of the palatine tonsils (carried out with a special syringe under the supervision of a specialist).
In addition, physiotherapeutic procedures have proven themselves well in the treatment of sore throat and chronic tonsillitis:
- electrotherapy;
- phonophoresis;
- phototherapy;
- laser therapy;
- Ural Federal District, etc.
If the parents of a sick child seek medical help too late, and the disease has become irreversible, and conservative methods have not brought the expected result, surgical treatment (tonsillectomy) may be required.
Larynx in children
The larynx in young children has a funnel-shaped shape (later - cylindrical) and is located slightly higher than in adults (at the level of the 4th cervical vertebra in a child and the 6th cervical vertebra in an adult). The larynx is relatively longer and narrower than in adults; its cartilages are very pliable. The false vocal cords and mucous membrane are delicate, rich in blood and lymphatic vessels, elastic tissue is poorly developed. The glottis in children is narrow. Young children's vocal cords are shorter than older children's, which is why they have a high-pitched voice. From the age of 12, boys' vocal cords become longer than girls'. These features of the larynx explain the easy development of stenotic phenomena in children, even with moderate inflammatory changes in the mucous membrane of the larynx.
The increased neuromuscular excitability of a small child is also of great importance. Hoarseness, often observed in young children after a cry, often depends not on inflammatory phenomena, but on the weakness of the easily fatigued muscles of the vocal cords.
Symptoms of tonsillitis
The manifestations of tonsillitis directly depend on the form of the disease. Thus, chronic tonsillitis is characterized by mild pain in the throat, discomfort when swallowing, the appearance of bad breath, and a low-grade fever (temperature in the range of 37-37.9 ° C). The acute form of tonsillitis has a greater number of characteristic symptoms. The presence of a disease in a child is indicated by the following manifestations:
- intense pain in the throat, aggravated by swallowing, eating, talking;
- partial or complete loss of voice, hoarseness;
- swelling and hyperemia of the tonsils;
- a sudden increase in body temperature to 39-40°C, which lasts about a week;
- general weakness;
- chills;
- body aches;
- enlarged lymph nodes.
The occurrence of any of these symptoms is a serious reason to contact a qualified otolaryngologist.
Trachea in a child, children
The trachea in newborns is funnel-shaped, its lumen is narrow, the posterior wall has a wider fibrous part, the walls are more pliable, the cartilage is soft and easily compressed. Its mucous membrane is delicate, rich in blood vessels and dry due to insufficient development of the mucous glands, elastic tissue is poorly developed. The secretion of the glands provides a layer of mucus on the surface of the trachea 5 microns thick, the speed of which is 10-15 mm/min (provided by cilia). The growth of the trachea occurs in parallel with the growth of the body, most intensively in the 1st year of life and during puberty. The structural features of the trachea in children lead to the easy occurrence of stenotic phenomena during inflammatory processes; frequent isolated lesions (tracheitis), combined with damage to the larynx (laryngotracheitis) or bronchi (tracheobronchitis) are determined. In addition, due to the mobility of the trachea, its displacement may occur during a unilateral process (exudate, tumor).
Bronchi in a child, children
The bronchi are quite well formed at birth. The growth of the bronchi is intense in the 1st year of life and during puberty. Their mucous membrane is richly vascularized, covered with a layer of mucus, which moves at a speed of 3-10 mm/min, in the bronchioles it is slower - 2-3 mm/min. The right bronchus is like a continuation of the trachea; it is shorter and wider than the left. This explains the frequent entry of a foreign body into the right main bronchus. The bronchi are narrow, their cartilage is soft. Muscle and elastic fibers in children of the 1st year of life are not yet sufficiently developed. The tenderness of the bronchial mucosa and the narrowness of their lumen explain the frequent occurrence of bronchiolitis with complete or partial obstruction syndrome in young children.
Lungs in children, child
The lungs of newborns weigh about 50 g by 6 months. their mass doubles, triples by the age of 12, increases 10 times by the age of 12, and 20 times by the age of 20. The pulmonary fissures are poorly expressed.
In newborns, the lung tissue is less airy, with abundant development of blood vessels and connective tissue in the septa of the acini and an insufficient amount of elastic tissue. The latter circumstance explains the relatively easy occurrence of emphysema in various pulmonary diseases.
The formation of the lung structure in children depends on the development of the bronchi
The formation of the lung structure occurs depending on the development of the bronchi. After the trachea divides into the right and left main bronchi, each of them is divided into lobar bronchi, which approach each lobe of the lung. Then the lobar bronchi are divided into segmental bronchi. Each segment has independent ventilation, a terminal artery and intersegmental septa made of elastic connective tissue.
The segmental structure of the lungs is already well expressed in newborns. There are 10 segments in the right lung, 9 in the left. The upper left and right lobes are divided into three segments - 1, 2 and 3rd, the middle right lobe - into two segments - 4th and 5th. In the left lung, the middle lobe corresponds to the lingular lobe, which also consists of two segments - the 4th and 5th. The lower lobe of the right lung is divided into five segments - 6, 7, 8, 9 and 10th, and the left lung - into four segments - 6, 8, 9 and 10th. In children, the pneumonic process is most often localized in certain segments (6, 2, 10, 4, 5), which is associated with the characteristics of aeration, the drainage function of the bronchi, the evacuation of secretions from them and possible infection.
External respiration , that is, the exchange of gases between atmospheric air and the blood of the capillaries of the lungs, is carried out through simple diffusion of gases through the alveolar-capillary membrane due to the difference in the partial pressure of oxygen in the inspired air and venous blood flowing through the pulmonary artery into the lungs from the right ventricle. Compared to adults, young children have pronounced differences in external respiration due to the development of acini, numerous anastomoses between the bronchial and pulmonary arteries, and capillaries.
Causes of hypertrophy
In the human body, tonsils or tonsils perform a protective function. This organ is located at the intersection of the nasal canals of the pharynx, directly at the base of the tongue. From the outer part of the neck, the tonsils are palpable, especially if they have increased significantly in size. The main function they perform is to prevent the entry of bacteria and infections along with food, water and air.
If the number of pathogens that enter the pharynx is excessive and the lymphoid tissue cannot cope with its main function, then its inflammation occurs, as a result of which it becomes the causative agent of the pathological process, as it progresses, the tonsils enlarge. When this organ is enlarged in a child, experts call this disease chronic tonsillitis or its acute form. Another name for this disease is sore throat .
An increase in the size of a child's tonsils can be considered as a sign of a decrease in the protective properties of the immune system, as well as dysfunction of the filtering organ, which accumulates microorganisms and gradually becomes inflamed.
Depth of breathing in children
The depth of breathing in children is much less than in adults. This is explained by the small mass of the lungs and the structural features of the chest. The chest in children of the 1st year of life seems to be in a state of inhalation due to the fact that its anteroposterior size is approximately equal to the lateral size, the ribs extend from the spine almost at a right angle. This determines the diaphragmatic nature of breathing at this age. A full stomach and bloated intestines limit the mobility of the chest. With age, it gradually moves from the inspiratory position to the normal one, which is a prerequisite for the development of thoracic breathing.
How to treat?
In children, therapy for enlarged tonsils differs from that used for adults. The doctor prescribes specific medications for the child. Mostly, the specialist prescribes macrolides, since when taking penicillin-type drugs, a child’s body may experience an allergic reaction. On an individual basis, the doctor selects the dose , as well as the course of treatment, which, after the onset of remission, must in no case be interrupted.
In addition to medications, additional therapy should include, as Dr. Komarovsky agrees, rinsing procedures and inhalations, for which herbal decoctions or infusions should be used. It is also recommended to irrigate diseased tissues with children's antiseptics.
When tonsillitis occurs in a chronic form, then in this case children with this disease are registered. During periods of exacerbation - in spring and autumn, preventive therapy is carried out in full accordance with the individual program selected by the doctor. In order to ensure regulation of the size of the lymphoid gland, the doctor prescribes treatment methods that have a gentle effect on the inflamed tissue.
If a specialist observes a deterioration in the child’s immune system, rheumatism develops, or heart disease occurs in addition to disruption of the vascular system, then surgery is recommended. This measure is carried out mainly to ensure that the child does not lag behind in his development and does not experience a decline in mental abilities .
Conservative methods
Traditional therapeutic methods of treatment used for inflamed tonsils include the following:
- antibacterial methods, which are based on taking drugs with an immunostimulating effect. They also include rinsing and lubricating enlarged tonsils with antiseptic drugs,
- physiotherapeutic procedures with ultrasound, laser, as well as the use of other energy sources for therapeutic effects on the inflamed organ,
- vitamin therapy.
Oxygen requirements in children are significantly higher than in adults
The oxygen requirement in children is much higher than in adults. Thus, in children of the 1st year of life, the need for oxygen per 1 kg of body weight is about 8 ml/min, in adults - 4.5 ml/min. The shallow nature of breathing in children is compensated by a high breathing frequency (in a newborn - 40-60 breaths per 1 minute, at the age of 1 year - 30-35, 5 years - 25, 10 years - 20, in adults - 16-18 breaths per 1 min.), with the participation of most of the lungs in breathing. Due to the higher frequency, the minute volume of breathing per 1 kg of body weight is twice as high in young children as in adults. The vital capacity of the lungs, that is, the amount of air (in milliliters) maximally exhaled after maximal inhalation, is significantly lower in children compared to adults.
Thus, the anatomical and functional features of the respiratory system in children create the preconditions for milder breathing disorders than in adults.