After tooth extraction, patients closely monitor the healing process of the hole. And usually everything goes well - the wound heals, new tissues form, redness in the area of the injured gum disappears. But sometimes frightening formations appear - lumps, hematomas, compactions. Of particular concern is the white growth after tooth extraction. In this case, consulting a doctor is advisable, since the growths can be both safe and requiring treatment.
Signs of alveolitis
The following symptoms indicate alveolitis of the socket:
- Socket pain that continues or renews on the 3-5th day after tooth extraction. In an uncomplicated postoperative period, it resolves in 1-2 days. At the beginning of the disease it is aching and becomes more intense after eating. At a later stage, the pain is constant and cannot be tolerated; painkillers help for a short time. It can radiate into the ear, into the temple on the side of the sore hole.
- The appearance of a bitter taste and putrid odor from the mouth.
- Enlargement and tenderness of the submandibular lymph nodes.
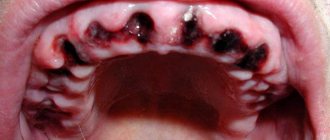
Upon examination, when alveolitis has just begun, the dentist discovers:
- redness of the gums,
- contents in the form of remains of a loose blood clot, food particles, saliva in the wound,
- that the hole is “dry”;
- in the midst of inflammation:
- swollen red mucous membrane along the edges of the hole,
- soreness when touched,
- there is a gray or yellowish coating on the walls.
The patient himself causes the “dry socket” effect to appear.
A dry socket will definitely manifest itself if the patient does not adhere to the dentist’s recommendations after tooth extraction and willfully allows such actions as
:
- thinking that he is making his condition easier by rinsing blood clots out of the tooth socket too often and intensively;
- thinking that his tongue has healing properties, he constantly “checks” with his tongue the surrounding tissue of the pit and the pit itself inside;
- Having convinced himself that he should drink in a thin stream, he drinks everything through a straw or sips all drinks from a spoon with his lips, thereby creating a vacuum effect in the mouth;
- not giving a damn about the doctor’s strict recommendations, he ignores the restrictions, and at least a little, at least a little, engages in heavy physical labor or sports during the rehabilitation period after removal (oh, like, look how cool I am!).
Dry socket syndrome in wisdom teeth
The concept of dry socket syndrome refers to the wisdom tooth. In the case of a wisdom tooth, this is practically alveolitis. It can also occur in this area, especially in the area of the lower wisdom teeth due to the fact that as a result of swallowing, as a result of opening the mouth, the muscles tense, which aggravate the occurrence of alveolitis.
What can dry socket syndrome lead to and what to do?
Dry socket syndrome can lead to very severe pain that radiates to the temple and ear. This is a very great torment: a person cannot, even if he is not sensitive, he cannot tolerate it, he will definitely take painkillers 4-5 or 6 tablets. And as a result of this, he will still go to the dentist. This dry socket condition will not go away on its own. It can only get worse - up to inflammation of the jaw, alveolitis. There can be very disastrous consequences.
Causes of alveolitis
Normally, after a tooth is removed, a clot of blood cells and fibrin, the protein from which a blood clot is built, forms in the socket. It almost completely covers the bottom and walls of the alveoli. The clot serves as a mechanical barrier, biological protection against infection and additional injury to the wound surface. In this case, healing occurs by primary intention. The wound is slowly filled first with loose tissue, then with denser connective tissue, and later with young bone.
But there are situations when the healing process is disrupted.
Inflammation of the socket occurs if:
- The operation was highly traumatic, which reduced the protective capabilities of one’s own tissues;
- The blood clot, as the main defense, is broken or completely absent (“dry socket”):
- prolonged bleeding;
- early destruction of the clot;
- non-compliance with the rules of care (for example, increased rinsing, eating hard or too hot food soon after surgery);
- Tooth extraction was carried out for emergency reasons due to an acute infectious process: periodontitis or periodontitis with complications;
- There are common reasons:
- reduced immunity;
- blood clotting disorder;
- elderly age;
- lack of proper dental hygiene.
Content:
- When white plaque is the norm
- When white plaque is a harbinger of disease
- Why do complications occur after tooth extraction?
- How to recognize the problem
- Diagnostic measures
- Treatment of alveolitis
After tooth extraction, it is important to monitor the condition of the mucous membrane.
Very often a white coating appears in the extraction area. It frightens patients because it seems something strange to them, and to some it resembles an accumulation of purulent masses. It should be noted that white plaque in the socket after tooth extraction can be either normal or a complication. In the first case we are talking about natural regeneration, in the second - about alveolitis.
Diagnosis and treatment of alveolitis of the socket after tooth extraction
If you have had a tooth removed, but after 2 days the pain in the socket has not gone away, or additional signs of inflammation have appeared, you should not postpone your visit to the doctor. Self-medication can lead to complications such as periostitis, osteomyelitis, and damage to adjacent teeth. The sooner treatment begins, the faster and with less risk of unpleasant consequences the wound will heal.
Even if your tooth was removed in another clinic, our specialists will help you.
Typically, diagnosing alveolitis of the tooth socket is not difficult. A medical history and examination is sufficient. But if necessary, to clarify the depth of the lesion, you may be prescribed additional studies: radiography or radiovisiography.
SM-Dentistry uses only high-quality materials; all instruments are sterilized using powerful sterilizers that eliminate the possibility of infection.
Treatment measures for alveolitis at SM-Dentistry:
- Local anesthesia will relieve acute pain and help you endure treatment.
- Complete cleansing of the wound from parts of the destroyed blood clot, food debris, plaque - a clean wound surface should remain.
- Treatment with disinfectants, antimicrobial and anesthetic agents.
- Application of a special turunda (tampon with medications).
The doctor will give recommendations for further care:
- special baths with antiseptic;
- painkillers;
- gentle diet.
It is possible that treatment of socket alveolitis will need to be supplemented with physiotherapeutic methods.
Healing of the tooth socket after extraction
Tooth extraction is a surgical intervention with the formation of a wound after extraction, therefore, as after any intervention, the wound formed at the site of the tooth must also undergo a healing process, and its tissue must recover and fill the voids. This process lasts for 4 months. The stages of tooth socket healing are as follows:
- a blood clot forms immediately after removal;
- 2-3 days - epithelization of the hole begins;
- 3-4 days - the first signs of granulation tissue formation appear;
- 7-8 days - part of the blood clot is replaced by granulations, gum cells begin to form an epithelial layer; the process of bone tissue formation begins;
- Days 14-18 - granulation tissue completely fills the socket, and the socket itself is completely covered with new epithelium. New bone cells are actively forming on the walls of the socket;
- 1-2 months - active process of bone tissue formation;
- 2-3 — filling the hole with bone tissue; tissue saturation with calcium;
- 4th month - bone formation ends, the structure becomes spongy.
If, when a tooth is removed, a blood clot does not form in the socket, the healing process of the socket occurs thanks to its walls - they are the ones who contribute to the development of granulation tissue. Otherwise, the further stages of healing are the same as those described above.
Healing after removal of an inflamed tooth
We have described a 4-month process of tissue restoration, however, they are restored so quickly only if there is no injury, inflammation or infection in the tooth and surrounding tissues. If the listed processes take place, tissue regeneration does not proceed so quickly. As a rule, it is prevented by the formation and course of the inflammatory process, the time period increases and the stages of healing look like this:
- epithelization and formation of granulation tissue occur in 10-15 days instead of 3-5 days;
- Bone tissue formation begins only on the 15-16th day instead of the 7-8th.
- closure of the hole by the epithelium is 2 times slower and ends only on the 30th or 50th day;
- only at 2 months the hole is completely filled with osteoid cells, which then become full-fledged bone;
The process of epithelium and bone formation can be even longer if the walls of the socket and/or gum tissue were severely damaged during tooth extraction.
Possible complications
Since tooth extraction is a surgical procedure, unpleasant consequences may arise after it is performed—complications of various kinds. In this case, the causes of such complications can be either the patient’s negligence in hygiene after surgery or the incorrect actions of the surgeon. Another category of etiology of adverse consequences is the complex course of the operation (with increased bone strength, non-standard shape or size of the tooth root).
Alveolitis
Alveolitis often forms when, after removal, a blood clot does not form in the socket for some reason. Without a clot, the socket is deprived of a protective barrier from external influences and is therefore susceptible to the appearance of an inflammatory process. The first and main symptom of this disease is pain immediately after removal or after 2 days. There is swelling of the gums, inflammation of the edges of the socket, due to the fact that a blood clot has not formed, the cavity is filled with food, which further contributes to the development of the inflammatory process. Other characteristic signs: temperature, unpleasant odor from the hole, poor health, pain and swelling of the mucous membrane at the extraction site.
The etiology of the development of alveolitis is considered to be an infection caused by oral microbes entering the socket. The body is not able to form a protective barrier in the hole, so inflammation rapidly develops in it.
The following causes of alveolitis are distinguished:
- chronic inflammation in the tissues of the oral cavity, its exacerbation;
- high degree of tissue trauma due to complex tooth extraction;
- a blood clot did not form during or after the operation (for example, due to the patient’s violation of the doctor’s recommendations);
- disorders in the immune system, chronic fatigue, chronic diseases;
- long removal process (longer than 40 minutes).
Treatment of alveolitis
Depending on the severity of alveolitis, both local and general treatment can be prescribed. Local methods are usually used using antiseptic rinsing and treating the socket with an antimicrobial agent. In addition to this treatment, vitamins and antibiotics may be prescribed.
In the case of general treatment, physiotherapy is also added, and the overall period of treatment and healing of the hole is increased.
Socket bleeding
Bleeding can occur both immediately after the operation and some time after the operation: from 1 hour to 24 hours or more. The period of manifestation of alveolar bleeding varies depending on the reasons that cause it. An earlier manifestation may be caused by vasodilation, later - due to injury to the socket by the patient after surgery. However, the etiology of the complication may also include injuries during removal (gums, alveoli, blood vessels) and diseases of the body (sepsis, hypertension, leukemia, the first 2 days of the menstrual cycle in women, taking aspirin and its analogues, diabetes).
The process of preventing bleeding depends on what causes it: local causes are eliminated by applying sutures to the rupture sites or applying cold, using a tampon. If the bleeding is caused by low blood clotting, medications are used to increase clotting.
Paresthesia
Sometimes after tooth extraction, patients complain of numbness in the oral cavity. Symptoms can be expressed over a period of 1 to 30 days or even more. The cause of paresthesia lies in nerve damage. Dentists can speed up the restoration of damaged tissue by prescribing vitamins B and C to the patient in combination with injections of galantamine and dibazole.
Neighboring teeth change position, Popov-Gordon effect
The body does not tolerate emptiness, therefore, after a tooth is removed and there is no analogue in its place for a long time, the neighboring teeth (and the tooth on the opposite jaw) tend to fill the resulting space, leaning towards the socket. Obviously, in such a situation, the dentition changes, which leads to curvature, changes in chewing load and bite.
The problem can be solved by replacing the missing tooth with an analogue after the hole has healed and tissue restoration: an implant, a prosthesis.
Communication of the oral and nasal cavities
When extracting molars and premolars of the upper jaw, the floor of the maxillary sinus may be injured, which will lead to the formation of a connection between the oral cavity and the nasal cavity.
It is noteworthy that this complication occurs even if all actions were performed correctly by the dentist. Its causes are usually:
- absence of a bone septum or close adherence of the roots to the sinus;
- bone destruction due to chronic inflammation in the area of the apex of the tooth root;
The complication requires surgical intervention by a specialist, since the entry of food and drink into the nose through the oral cavity usually leads to inflammation in the sinus (sinusitis), which in itself is a very unfavorable consequence and requires long and complex treatment.
Intervention is not carried out only if acute purulent sinusitis of the upper jaw has developed.
Other complications
Other complications are caused by: incorrect actions of the doctor and the characteristics of the patient’s body.
First category of reasons:
- improper use of forceps and, as a result, damage to the crest of the alveolar tissue;
- erroneous extraction of a tooth germ due to the ignorance of the doctor during milk extraction;
- injuries to adjacent teeth due to careless work of a dental surgeon;
Second category of reasons:
- weak or defective teeth located nearby may break during surgery on the causative tooth;
- low strength of the causative tooth, which causes its fracture and the need to remove parts;
- weak jaw tissue, which increases the risk of fracture and complications;
- individual features of the structure of the roots, jaw and location of nerves.
Rules of care
To prevent complications due to the patient’s fault, it is very important to follow all the dentist’s instructions, namely:
- The first day after surgery: keep the installed tampon in the mouth for 30 minutes, do not eat for 2 hours; do not load food and do not touch the socket area with your tongue or toothbrush;
- 2-3 days after surgery, minimize the load on the teeth located in the extraction area, limit the intake of solid and hot foods, giving preference to soft and liquid foods;
- Refrain from smoking (to prevent a vacuum from occurring in the socket) and try not to drink alcoholic beverages;
- Buy a soft toothbrush to gently clean the area of the extracted tooth a few days after the operation; in the first days it is better not to brush the injured area at all;
- The next day after the operation, make oral baths for the socket (do not rinse under any circumstances) with warm salted water (but not with special rinses).
- Do not exercise for 2-3 days;
- Do not take a hot bath on the first day after removal;
- Do not take aspirin and its analogues.
Prevention of alveolitis at SM-Dentistry
If the operation is not an emergency, then dentists first treat caries and other inflammatory diseases in the oral cavity, which can become a source of infection.
After the operation, you will receive detailed recommendations for caring for the socket so that the blood clot forms correctly and does not break down prematurely. To do this, you must follow a diet (do not eat hard or hot foods), do not use intensive rinsing and cleaning in the area of the injured hole, and use antiseptic and painkillers.
Sign up for a consultation with a dental surgeon by calling 24/7 in Moscow +7 (495) 777-48-06.
Dentist consultation Treatment of caries
Dentists' recommendations
After surgery, it is important to monitor the condition of the wound and follow the doctor's instructions. The hole filled with blood gradually overgrows and is completely covered with granulation tissue 14-20 days after the operation. The first three days after tooth extraction you cannot:
- rinse the mouth,
- eat solid food
- drink through a straw
- smoking and drinking alcohol,
- use a brush with stiff bristles,
- take a hot bath and go to the sauna.
If possible, you should avoid physical activity and stop taking medications that prevent blood clotting. Compliance with the listed recommendations contributes to the speedy healing of the wound.
Prices
| Name of service | Price, rub.) * |
| Initial consultation with a dentist-therapist | 1,500 rub. |
| Repeated consultation with a dentist-therapist | 800 rub. |
| Treatment of caries (imaging, anesthesia, isolation of the oral cavity, installation of an insulating lining and filling made of composite light-curing imported material) | from 4,350 rub. |
| Treatment of alveolitis with socket revision | 3,000 rub. |
We accept VISA, MASTERCARD, MAESTRO bank cards for payment.
Would you like us to call you back?
Treatment of alveolitis
If alveolitis occurs after tooth extraction, you need to undergo dental treatment aimed at:
- elimination of the infectious focus;
- preventing possible complications;
- maintaining the integrity of the rest of the dentition.
First, the dentist cleans the socket and rinses it. It is important to wash away all purulent masses and dead tissue from it. Antiseptics and hydrogen peroxide work well for this purpose.
To reduce painful symptoms, which deprive the patient of the opportunity to fully rest and work, analgesics are used. It is better to use them by applying applications. Compresses are changed every half hour. It is also possible to take drugs orally, that is, in the form of painkillers and anti-inflammatory tablets.
If the patient has concomitant diseases or reduced immunity, the doctor may decide to prescribe antibiotics. They quickly relieve inflammation and speed up the healing of damaged tissue.
If you seek qualified dental care in a timely manner, the prognosis for alveolitis is favorable. After 3-5 days, the symptoms begin to subside, and the person’s well-being improves. Residual socket pain may persist for another 2-3 weeks, but it does not pose a threat.
Temperature increase
Tooth extraction usually does not cause an increase in temperature; in rare cases, there is an increase in temperature up to 37.5º in the first few hours after the operation, but this also goes away by the evening of the same day. If the temperature is higher and lasts longer, this may be a sign of an inflammatory process in the socket. In this case, you should immediately consult a doctor.
Reasons for the release of osteomaterial
The reasons for the appearance of osteomaterial differ depending on the location of its “loss”.
When appearing in the oral cavity
Bone chips enter the oral cavity as a result of suture divergence, disruption of the location of the bone material or the membrane holding it.
This complication appears in the first 2-7 days, when regeneration processes have not yet begun and the material has not been fixed by connective tissue (a single bone mass has not begun to form).
After at least 10-14 days from the moment of intervention, such a complication is rare - new bone tissue is formed, the granules bind and are not able to come out.
Dehiscence of sutures and displacement of the graft are often combined with the appearance of mobility of the dental implant (if installed) and bleeding.
Most often occurs due to errors by the patients themselves as a result of:
- playing sports (especially running, diving, cycling);
- head injuries;
- visiting the sauna;
- non-compliance with the rules for caring for seams.
Less commonly, the complication is associated with surgeon errors:
- use of low-quality suture material;
- errors in suturing;
- ignoring the use of membranes.
We recommend contacting trusted clinics that do not skimp on materials or doctors’ salaries.
When exiting through the nasal passages or nasopharynx
The appearance of bone material in the nasal passage on the operated side or exit through the nasopharynx is associated with its entry into the maxillary sinus, which communicates with the nasal cavity. This is possible if the sinus lining is damaged during surgery.
It is better to entrust such operations to an experienced doctor. Moreover, not just a dental surgeon, but an oral and maxillofacial surgeon with ENT training.
The situation can also occur with injuries leading to dislocation of a dental implant (in the case of simultaneous implantation and sinus lift). As a result of displacement of the implant, there is a possibility of compromising the integrity of the sinus mucosa.
As a result, bone material leaves the cavity through the nasal passage or nasopharynx. In the worst case, it remains in the sinus, which leads to the development of inflammation and unilateral sinusitis.
Any procedures carried out in the area of the maxillary sinuses must necessarily end with X-ray control. If foreign bodies are detected, removal must be immediate.
Edema
Swelling is another unpleasant consequence of tooth extraction. As a rule, it appears the next day after surgery and reaches its maximum value on the third day, after which it begins to decrease.
Cold compresses can be used to reduce swelling. To do this, you need to prepare ice cubes in advance, wrap them in cloth and apply them to the operation site for no more than twenty minutes. After a twenty-minute break, the procedure can be repeated. But it should be remembered that this method is effective in combating edema only in the first thirty-six hours after surgery.
What to do if bone loss occurs
If bone material comes out after a sinus lift, this should serve as an incentive for prompt action.
- The sooner the diagnosis is made and adequate treatment is started, the more favorable the further prognosis will be.
- If the start of treatment is delayed, pathological adhesions may develop with the implant being fixed in the wrong position.
In any case, a computed tomography scan is performed first . Allows you to determine the degree of “disaster” and not miss the onset of the inflammatory process:
- assess the condition of bone tissue;
- determine the quantity and placement of the remaining material;
- identify its presence or absence in the maxillary sinus.
If bone chips were released only from the oral cavity
Surgery is being performed. Sometimes it is possible to limit oneself only to plastic surgery of the bone material, filling the resulting gaps and re-applying sutures.
If osteomaterial gets into the sinus
Treatment can last for several months and will take place in several stages:
- Removal of a dislocated implant (if installed).
- Elimination of infectious complications - sinusitis, fistula (if present).
- After 1-2 months, in the absence of repeated complications and normal healing, a repeat sinus lift may be performed.
- Implantation is performed 3-6 months after the new bone is formed.
Our Center specializes in solving problems associated with complications in the maxillary sinuses
Patients often come to us after a failed sinus lift. The Center has a full-fledged ENT department to provide surgical care in complex clinical situations. A modern ENT unit includes all the necessary equipment for carrying out operations, including the removal of foreign bodies that provoked inflammation.
Levin Dmitry Valerievich
Founder and Chief Doctor of the Center
Injuries during tooth extraction
They are considered a complication, most often appear on the upper jaw, the highest risk is when removing premolars and molars. If removal is difficult, there is a risk of perforation of the floor of the maxillary sinus. It becomes damaged, and a hole appears in the bony septum between the nasal and oral cavities. This may be due to the anatomical features of the jaw structure (there is no bone septum or the roots of the teeth being removed are located close to the bottom of the sinus). Another possible cause is chronic inflammation in the area of the tooth root, due to which the bone septum becomes thinner and destroyed. Such an injury is eliminated immediately. If this is not done, liquid may enter the nose when swallowed or chewed. If such a symptom appears, you should contact your dentist so as not to provoke inflammation.