Indications for treatment of periodontitis
There are two main ways to treat periodontitis: conservative and surgical. Each of them has its own indications and contraindications.
According to modern dental standards, a doctor should give preference to conservative methods. They are indicated for both acute and chronic periodontitis, including the appearance of cysts and granulomas, loose teeth, and increasing inflammation.
However, orthograde treatment cannot be used in all cases. Indications for surgical intervention are:
- obstruction of the tooth root canals;
- the presence of a stump tab or pin that cannot be removed without damaging the roots;
- multiple perihilar cysts or cysts growing into the maxillary sinus;
- wide affected area (over 10 millimeters);
- perforation of the tooth cavity or root wall;
- ineffectiveness of conservative treatment methods.
Important!
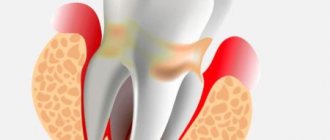
When we talk about periodontitis, we often mean apical (also known as periapical or apical) periodontitis - that is, inflammation at the apex of the tooth root. The cause of this disease is endodontic problems. Another type of periodontitis, marginal, affects the gums in the cervical area of the tooth, but it already belongs to the field of periodontology. This material is devoted to the treatment of apical periodontitis only.
Exacerbation of chronic periodontitis
Often patients seek treatment for acute chronic periodontitis, which manifests itself quite clearly. This mainly applies to granulomatous and granulating types, exacerbations of which occur much more often than fibrous types. Clinical manifestations during this period include:
- constant localized pain;
- swelling of soft tissues;
- the presence of a reaction to mechanical stimuli;
- painful reaction of the lymph nodes.
Treatment methods for dental periodontitis
| Conservative treatment | Surgery |
Therapeutic:
Physiotherapeutic:
Conservative treatment of periodontitis is accompanied by the use of antibiotics. | Surgical treatment:
|
Important!
The probability of successful conservative treatment of periodontitis is 70 - 90%
Causes of acute periodontitis
Among the main reasons for the development of acute periodontitis are:
- acute inflammation of the pulp that occurs against the background of teeth affected by caries; pulp and periodontal tissues are closely related;
- the use of arsenic for pulp devitalization, which provokes inflammation of the pulp tissue due to the toxic effect of the drug penetrating the periodontium;
- the use of strong antiseptics and various cauterizing agents that are injected into the root canal, which provokes inflammation in nearby tissues;
- entry of a large amount of filling material into the periodontal space.
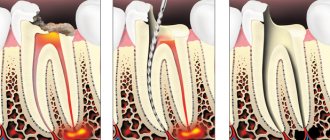
Stages of periodontitis treatment
The number of visits to the clinic for the treatment of periodontitis depends on the stage of the disease (acute periodontitis, chronic, chronic in the acute stage) and the chosen technique. Often, therapy is carried out in several stages and requires at least 2 - 3 visits to the attending physician, since it is not recommended to install a permanent filling until the inflammation is completely removed.
- Preparation for treatment: diagnosis using an x-ray, anesthesia injection.
- Drilling a tooth to access canals, removing a nerve, or removing an old filling.
- If necessary, expand channels.
- Antiseptic treatment of canals, application of medications, physiotherapeutic procedures.
- Installation of a temporary filling.
- Removal of the temporary filling, antiseptic treatment of the canals (this stage is repeated until the source of inflammation is completely eliminated; sometimes this may take several months).
- Installation of a permanent filling, control x-ray.
In parallel, the patient is prescribed antibacterial and anti-inflammatory therapy, as well as home rinses with disinfectant solutions.
Recommendations after treatment
After conservative or surgical treatment, you should not eat food for 2-3 hours due to the effects of anesthesia. Pain may be experienced for 7 days after surgery. It is recommended to rinse your mouth with antiseptics and a decoction of medicinal herbs. For severe pain, it is recommended to take painkillers. If pain persists and severe swelling is observed, contact your doctor immediately.
At the same time, the crown of the tooth changes its color, the presence of a carious cavity and tooth mobility are noted. Dentists at the CELT clinic successfully treat even the most advanced and severe forms of chronic periodontitis!
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
Features of the treatment of periodontitis with fistula
Odontogenic fistula is one of the complications of periodontitis, mainly granulating. It consists of holes in the mucous membrane, which are formed due to the proliferation of granulations and destruction of the tissues surrounding the tooth. In severe cases, a fistula can appear not only in the gum, but also in the cheek, and even on the skin of the face. Purulent contents are released through the hole, which appears due to the inflammatory process in the periodontium.
On the one hand, the formation of a fistula facilitates the course of the disease, since inflammatory products are eliminated through it (which means that the patient most likely will not suffer from severe pain). On the other hand, non-intervention over time can lead to tooth loss.
You can get rid of a fistula only by eliminating its cause - damage to periodontal tissue. Treatment follows a standard scheme: mechanical treatment of the canals, disinfection and thorough filling. Due to the outflow of pus through the fistulous tract, treatment is most often successful and takes less time. After creating suitable conditions, the fistula goes away on its own, but in severe cases, surgical removal of overgrown granulations may be necessary.
What happens if the fistula is not treated?
If the fistula is not treated, then nothing good will end. The tooth will need to be removed, and what’s more, the bone surrounding the tooth suffers greatly, and the vestibular cortical plate suffers. When the tooth is not treated, when the cause of the fistula is not dealt with, the cortical plate is quite destroyed. Large cavities are formed in the bone, as exudate is formed, all this rots and the bone decomposes, softens and becomes infected, lyses, and exits through the fistulous tract.
Therefore, in addition to, as I said earlier, there is a fairly strong load on the body, since a fistula is a constant open source of infection in the oral cavity.
Treatment of chronic forms of periodontitis
There are three types of chronic periodontitis: fibrous, granulating and granulomatous.
- In fibrous periodontitis, the tissues surrounding the apex of the tooth are replaced by fibrous tissue. The patient usually does not feel pain, and the disease can only be determined by an x-ray.
- Granulating periodontitis is characterized by the growth of granulation tissue: the process of bone resorption (resorption) starts, fistulous tracts are formed, through which inflammatory products are separated. As the granulations expand, the patient begins to experience periodic aching pain.
- Granulomatous periodontitis is accompanied by the appearance of a granuloma - a neoplasm at the root apex. It is a chamber of connective tissue filled with granulations. If the disease is not treated, the growth of granuloma can even lead to a jaw fracture.
Treatment of chronic periodontitis is often carried out using conservative treatment methods. According to modern standards, doctors, as a rule, do not carry out separate treatment for granulomas, cysts and fistula tracts: if the canals are disinfected and properly sealed, the neoplasms will disappear on their own. In advanced cases, surgical intervention is permissible.
Periodontitis - symptoms and treatment
Acute apical periodontitis
After periodontal damage for one of the above reasons, a short-term intense tissue response occurs.
This process is accompanied by clinical symptoms of acute periodontitis.[7] The tissue response is usually limited to the periodontal ligament. It leads to typical neurovascular inflammatory reactions, which are manifested by hyperemia (overflow of blood), vascular congestion, swelling of the periodontal ligament and extravasation (leakage into the tissue) of neutrophils. Since the integrity of the bone, cementum and dentin has not yet been compromised, periapical changes at this stage are not detected by X-ray examination.
If the inflammation was caused by non-infectious irritants, the lesion may disappear, and the structure of the apical periodontium is restored.[13][14]
When infection occurs, neutrophils not only fight microorganisms, but also release leukotrienes and prostaglandins. The former attract more neutrophils and macrophages to the affected area, and the latter activate osteoclasts - cells involved in the destruction of bone tissue. Thus, after a few days, the bone surrounding the periodontium can be resorbed (dissolved), then in the area of the root apex, an expansion of the periodontal fissure is detected radiographically.[15]
Neutrophils die at the site of inflammation and release enzymes from their granules that cause the destruction of extracellular matrices and cells. This “splitting” of tissue prevents infection from spreading to other parts of the body and provides space for protective cells to penetrate.
During the acute phase, macrophages also appear in the periodontium. They produce proinflammatory and chemotactic (allergic) cytokines. These molecules enhance the local vascular response, bone destruction and extracellular matrix degradation, and may also cause hepatocytes to increase the production of acute phase proteins.
Acute primary periodontitis has several possible outcomes:
- spontaneous healing;
- further strengthening and spreading into the bone (alveolar abscess);
- exit to the outside (formation of fistulas or sinus tract);
- chronization of the process.[19]
Chronic periodontitis
The prolonged presence of microbial stimuli results in a shift towards macrophages, lymphocytes (T cells) and plasma cells, which are encapsulated in collagenous connective tissue.
Pro-inflammatory cytokines (immune system cells) are powerful stimulators of lymphocytes. Activated T cells produce a variety of cytokines that reduce the production of proinflammatory cytokines, leading to suppression of bone destruction. In contrast, T cell-derived cytokines may simultaneously enhance the production of connective tissue growth factors, which has stimulatory and proliferative effects on fibroblasts and the microvasculature.
The possibility of suppressing the destructive process explains the absence or delayed bone resorption and restoration of collagen connective tissue during the chronic phase of the disease. Consequently, chronic lesions may remain asymptomatic for a long time without significant changes on radiographs.[21]
The balance that exists in the periodontium can be disrupted by one or more factors, for example, microorganisms “located” inside the root canal. They progress into the periodontium and the lesion spontaneously becomes acute with the reappearance of symptoms.
As a result, during these acute episodes, microorganisms may be found in the surrounding periodontal bone, with a rapid increase in radiographic appearance. This radiographic pattern is due to apical bone destruction that occurs rapidly during the acute phases and is relatively inactive during the chronic period. Consequently, the progression of the disease is not continuous, but occurs in intermittent bursts after periods of “stability.”
Cytological studies show that about 45% of all chronic periodontitis are epithelialized. When epithelial cells begin to proliferate, they may do so in all directions randomly, forming an irregular epithelial mass that contains vascular and infiltrated connective tissue. In some lesions, the epithelium may grow into the entrance of the root canal, forming a filling-like seal at the apical foramen.
Features of the treatment of periodontitis in the acute stage
Exacerbation of periodontitis goes through two phases: intoxication and exudation (appearance of discharge). As the disease progresses, the patient first experiences aching and episodic pain, and then constant throbbing and tearing pain, so treatment cannot be delayed.
Acute periodontitis can be serous or purulent. In the second case, purulent exudate accumulates in the apical part of the tooth root, and the main task for the doctor is to remove it. Sometimes this is enough to clean the tooth cavity and treat the canals, but in severe cases it may be necessary to cut the periosteum for drainage.
Symptoms of the disease
General symptoms depend on the form of the pathology. When granulomas form, attacks of pain are observed when exposed to hot food. Pressure on the affected tooth and gum is accompanied by pain. The size and density of the mucosa in the affected area changes, and a granuloma forms under the bone or mucosa.
An exacerbation is accompanied by the appearance of fistulas, which grow and gradually release their contents into the oral cavity. In this case, purulent fistulas can appear not only on the gums, but also on the cheekbones, cheeks, neck, and chin. Isolation of pus may be performed along with the isolation of granulosa tissue. Then the fistula goes away, and a scar appears in its place.
The granulomatous form occurs for a long time without pronounced symptoms. Only after the granuloma grows to a large size and cysts form, the main symptoms appear: discoloration and severe pain in the tooth, development of gumboil and swelling of the gums in the affected area. Cysts that are too large can cause a jaw fracture and long-term rehabilitation.
Fibrous periodontitis is the most hidden form of pathology. There is no pain when chewing food or drinking hot drinks. Severe symptoms are observed only during exacerbation. There is general poisoning of the body due to the penetration of pus into the blood, the tooth becomes loose, and the lymph nodes in this area become larger.
Treatment of periodontitis at home
Periodontitis cannot be cured at home, since the disease is caused by bacteria that colonize the dental canals. The only way to get rid of them is to carry out antiseptic treatment and sealing of the canals, and this can only be done by a doctor, but by waiting for a visit to the clinic, you can alleviate the symptoms and reduce pain.
Disinfectants that do not irritate the mucous membranes can be used for rinsing 4 - 5 times a day. Doctors also recommend rinsing with a solution of salt and soda, including after treatment, to relieve swelling and reduce inflammation. Non-steroidal anti-inflammatory drugs are suitable for pain relief. All this will help relieve symptoms, but is not a cure.
You may experience pain after periodontitis treatment. Normally, they last 3–5 days and gradually fade away. If the pain does not subside or returns with renewed vigor, re-therapy is necessary.
Signs of the disease
The nature of toothache indicates the degree of neglect of the disease. A doctor will help you determine the properties of pain during your consultation.
Making an accurate diagnosis is the doctor’s task, but below are the symptoms of periodontitis:
- prolonged pain or painful throbbing in the tooth or gum;
- increased sensitivity when pressure is applied to the tooth surface;
- asthenia or increased body temperature;
- phantom feeling of tooth swelling;
- swelling of the gums;
- lack of response to cold, hot or sweet;
- easy mobility.
Note! Those places where deep caries treatment was previously carried out are examined. Often, untreated carious disease caused deep tissue damage.
In this case, chronic periodontitis, as a rule, is asymptomatic and is diagnosed only on an x-ray, or when it enters the acute stage.
Reviews about our doctors
I would like to express my gratitude to the dentist Elena Nikolaevna Kiseleva and her assistant Svetlana - they are real specialists and at the same time sensitive, not burnt out by years of practice.
Thanks to them, I have been coming back here for many years. Thanks to the management for such doctors! Read full review Svetlana Nikolaevna
13.08.2021
I am very grateful to Evgeniy Borisovich Antiukhin for removing my three eights. Especially considering that the lower tooth was not the simplest (it was located in an embrace with a nerve). The removal took place in 2 stages, one tooth under local anesthesia, two under general anesthesia. I had no idea that wisdom teeth could be... Read full review
Sofia
28.12.2020
Treatment of periodontitis with folk remedies and pharmaceutical preparations
Treatment of periodontitis with folk remedies and pharmaceutical drugs is something we categorically do not advise you to do. Such treatment of periodontitis can be not only ineffective, but also dangerous - it can lead to severe complications. For example, heating the area of inflammation during periodontitis can only worsen your condition.
It is important to understand that high-quality treatment of periodontitis implies the mandatory destruction of infection in the tooth canals. And this can only be achieved by processing them and using special preparations. Herbs, ointments and antibiotics from the pharmacy will not cope with this task. Therefore, do not risk your health and contact professionals for the treatment of periodontitis.
Treatment of the tooth and its canals in the treatment of periodontitis
- Anesthesia of the area of the diseased tooth. It is impossible to do without the use of anesthetics in the treatment of periodontitis, since the inflammation has gone deep into the tooth and affected the nerve endings. Without local anesthesia, the process of treating periodontitis will be very unpleasant and painful for the patient.
- When the anesthetic takes effect, the doctor will begin working with the diseased tooth. Treatment of periodontitis involves the removal of all destroyed dental tissues, depulpation of the tooth, as well as treatment of the dental canals.
- Treatment of canals for periodontitis involves their expansion and washing with antiseptic solutions. In order to eliminate inflammation and destroy infection, the dentist will place an antibacterial drug in the cavity of the canals.
- The drilled tooth is covered with a temporary filling and after that a break is taken in the treatment of periodontitis. The doctor sends the patient home, but before that he prescribes antibiotics and anti-inflammatory drugs, and provides detailed advice on the care of his teeth and oral cavity. You must follow all the dentist’s recommendations exactly, otherwise the treatment of periodontitis will either take longer or, what is much worse, be completely ineffective.
Next time you will need to see the doctor in 3-4 days to continue treatment of periodontitis.
Temporary filling of dental canals in the treatment of periodontitis
During the second visit to the doctor for the treatment of periodontitis, a temporary filling of the tooth canals is performed. But first, a control image is taken to make sure that the inflammatory process has stopped and the tooth tissue has begun to recover.
The second stage of periodontitis treatment involves performing the following manipulations:
- Removing a temporary filling from a tooth;
- Removing medication embedded in the tooth canals;
- Washing the channel cavities with an antiseptic solution;
- Filling the canals with a special temporary composite containing substances that help tooth tissues recover faster and also destroy all pathogenic bacteria.
Why is temporary root canal filling needed in the treatment of periodontitis? This event allows you to completely stop the inflammatory process and reduce the risks of developing periodontitis in the future.
Temporary canal filling in the treatment of periodontitis is done for several months. After filling the canals, the tooth is again closed with a temporary filling.
Take a short test and calculate the cost of treatment!
Take a short test
Causes
There are several causes of the disease:
- Traumatic. The disease occurs due to a bruise, sharp biting on a hard object, or a blow to one tooth. Another possible cause is injury during root canal treatment with dental instruments.
- Infectious. It develops due to the penetration of microorganisms into the tissues surrounding the tooth root. Typically, periodontitis occurs due to Staphylococcus aureus, Streptococcus.
- Medication. Occurs due to the effect of potent drugs on the peri-apical tissues of the tooth. Signs of the disease appear within a few hours after exposure to the drug.
The inflammatory process can occur slowly or very quickly. This does not depend on the cause of its occurrence.