Darkening of the tooth near the gum can be caused by various reasons. Not all of them are associated with dental diseases and pathological processes in the oral cavity. For example, sometimes a tooth darkens due to taking medications containing iron gluconate, or excessive consumption of grape or tomato juice.
However, in most cases, the causes of darkening of the tooth near the root and gums are pathological processes. This is a reason to immediately contact a dentist. The following diseases lead to this symptom:
- Cervical caries;
- Tartar;
- Fluorosis.
Let's talk about these diseases and methods of treating them in more detail.
Cervical caries
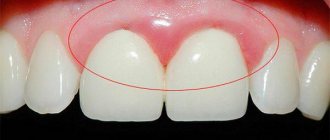
Cervical caries is localized on the neck of the tooth - the place where the enamel comes into contact with the gum. This pathological process occurs very quickly, which makes it one of the most dangerous types of this disease. Cervical caries can develop into pulpitis, periodontitis or a root pathological process within just a few months. It is much faster than localized, for example, on the vestibular or occulus surface.
Cervical caries requires immediate treatment. If the disease is started, the pathological process will quickly “spread” to the roots of the tooth. In this case, the patient will begin to experience acute pain. When the roots are destroyed, it becomes impossible to save the tooth, and the only way to “treat” is removal.
But there are also advantages. If cervical caries is detected at an early stage, when the pathological process has not yet affected the dentin and roots of the tooth, this disease can be cured using a conservative method. The dentist will perform fluoridation and remineralization of the enamel, restoring its strength. In this case, preparation is not required or minimal.
If the pathological process has reached the dentin - the patient is concerned not only about the darkening of the tooth, and increased sensitivity, as well as pain - then treatment is carried out by filling. The dentist removes the destroyed tissue, then cleans the tooth from the remains of harmful microorganisms and closes it with a filling.
The most common cause of cervical caries is insufficient dental hygiene. To prevent this disease, it is necessary to brush your teeth regularly, at least 2 times a day, use floss (dental floss), and, if you are predisposed, use an irrigator.
Why do some teeth turn dark?
There are several reasons:
Poor, incomplete, poor-quality cleaning of the tooth canal and carious cavities on the tooth
With such incomplete cleaning, the organic residues left inside the tooth (blood, pus, and others) begin to break down and cause darkening of the tooth.
The darkening of the front tooth from the inside can be caused by filling paste and waste products of bacteria that have developed in a poorly sealed canal. This case of tooth darkening is a case of moderate complexity of treatment. That is, darkening of the tooth, or more precisely, a change in its color, may be associated with the condition of the tooth canal, in which inflammation could develop due to incomplete removal of the pulp or leakage of the canal filling during previous treatment.
Canal filling with “wrong” dental materials
It is these incorrect materials that lead to a change in tooth color, up to brown shades.
This type of tooth darkening is a difficult case of treatment. Such cases are difficult to treat. Especially if the darkened tooth was treated a long time ago in another clinic. The filling material used to fill a tooth canal can cause darkening under certain conditions.
Tooth darkened after impact
When a tooth is hit (most often the anterior upper central one), the neurovascular bundle is torn off, which extends from the bone into the tooth. After this separation, the part of this bundle that remains in the tooth begins to collapse inside the tooth. The products of this destruction of non-living tissue stain the tooth. This case of darkening refers to mild cases of treatment.
Tartar
Tartar is a bacterial-mineral plaque that forms on the cervical surface of the enamel due to insufficient oral hygiene, as well as due to smoking and an incorrect diet.
First, a soft coating forms on the surface. It consists of bacteria and food debris. Soft plaque is easy to clean - it is removed even when chewing carrots, apples and other hard foods, as well as during oral hygiene using a toothbrush, floss or irrigator.
However, if a person does not remove the soft plaque, it can begin to petrify - change its structure, become hard and mineral. Turn into tartar. Hard plaque is much more difficult to remove - it often even resists cleaning with a classic brush.
Tartar is not only unsightly, it is also the cause of many diseases. For example, it can cause gingivitis and other gum inflammations. This occurs due to contact between bacteria and soft tissues of the oral cavity. But the most dangerous consequence of tartar is periodontitis, the inflammatory process of the periodontium, the tissues surrounding the roots and base of the tooth. It can lead to tooth mobility and loss.
Tartar treatment is quick and comfortable. Ultrasound, laser, or Air Flow technology can be used to break down mineral deposits. The dentist chooses a specific technique depending on the characteristics of the disease. Thus, thin dental plaque is cleaned using the Air Flow method - mineral deposits are removed by a water-air flow with the addition of active substances.
What to do if a tooth is rotten
Rotten teeth - what to do? The first step is to make an appointment with a dentist and get ready for long-term treatment:
- Complete diagnostics of the oral cavity. A comprehensive X-ray examination will indicate changes in dental tissues, even if this is not visible during a routine examination.
- Identification of the main rotten areas. The doctor will determine the number of affected teeth and the stage of decay for each unit.
- Coordination of the treatment plan. Dental protocols are aimed at preserving each dental unit, so an experienced dental therapist will guide the patient towards treatment and filling cavities. If the decay process has gone very far and the root is affected, then the dental unit will have to be removed followed by prosthetics or implantation.
- Carrying out treatment. A rotten tooth usually indicates pulpitis, so the patient will have the dental nerve removed, the cavities cleared of pus, and the crown restored with high-quality composite materials.
- Professional hygiene. This is a mandatory stage in the fight against rotten teeth, so the patient will be referred for the removal of soft plaque and tartar.
- Identification of the causative agent of the pathological process. The doctor will make a smear for analysis, and after laboratory testing, will select therapy for the patient’s quick recovery.
Dental treatment of rotting units is always comprehensive, aimed at physical restoration and elimination of the causes of decay.
Fluorosis
Fluorosis is a dangerous dental disease that is caused by consuming extremely large doses of fluoride. Usually this substance enters the human body along with tap water. In addition, the source of fluoride can be the work environment or even the wrong toothpaste.
Fluorosis begins with the appearance of white, dull spots on the surface of the teeth. They are not always visible to the naked eye. Over time, the spots change color - they first turn yellow, then turn brown. If you don’t consult a dentist at this point, fluorosis can turn into erosive or destructive forms - when the disease begins to destroy the enamel.
Treatment of fluorosis is almost always conservative. The dentist remineralizes the enamel, restoring the balance of calcium, phosphorus and fluoride. Darkened areas are bleached. In addition, the patient is recommended to change his lifestyle to reduce the amount of fluoride consumed - for example, install a special water filter at home or change his place of work.
Fluorosis is often “epidemic” in nature. If it is caused by an increased content of fluoride in tap water, it develops in the whole family. If the reason was a violation of industrial safety - for the entire team. In the Ryazan region, fluorosis is often detected in residents of the Rybnovsky, Chuchkovsky and Shatsky districts, where the water contains an increased amount of fluoride.
The root of a tooth has rotted: what to do?
If the root of a tooth has rotted, you cannot limit yourself to simple treatment. The affected unit will have to be removed. Otherwise, a rotten tooth root can have serious consequences:
- tissue necrosis;
- abscesses;
- headache;
- formation of a cyst at the root apex;
- fracture or dislocation of a tooth root;
- periodontal diseases.
After removal, you need to immediately resolve the issue of restoring the dentition line. This will help maintain the bite and stabilize the position of the treated teeth. The best option is implantation. And here different options are possible.
Implantation for rotten teeth
If an x-ray shows pathological processes in the root of the tooth, removal is unlikely to be avoided. But you can immediately consider implantation options with your doctor. An experienced dentist-implantologist will refer the patient for diagnostics - he will assess what the rotten tooth root looks like, what area is affected and then propose protocols:
- One-stage implantation. Suitable when part of the crown has rotted, but the root is only affected. In this case, the doctor will carefully remove the tooth and immediately install a dental implant. An artificial dental crown will be placed on the implant, and after the implant has completely healed, a permanent prosthesis made of metal ceramics or zirconium dioxide will be placed.
- Single-stage implantation. It differs from the previous protocol in that after implantation of the implant, the doctor will observe the healing process and only then perform prosthetics.
- Classic implantation. For rotten teeth, the most popular option, as it allows for consistent treatment. After removal, the doctor prescribes antibacterial therapy, conducts the necessary tests, and completely cures the patient. When the gums have healed and all the teeth have been treated, implantation is prescribed - the implantation of an artificial root into the bone tissue of the jaw. Sutures are placed at the implantation site and complete osseointegration is expected. This is important, since if there is residual tissue inflammation, the implant may be rejected. A positive result is secured by installing a permanent crown. All treatment takes from 4 months to a year.
It is also worth considering implantation when completely removing rotten units, which often leads to a toothless mouth in the patient. To restore the full jaw row, all-on-4 and all-on-6 protocols are used - to install a fixed prosthesis on 4 or 6 implants.
Treatment of a darkened tooth
Darkening of the tooth near the gum requires immediate consultation with a doctor, regardless of the cause. If you leave the disease to its own devices, you can face more dangerous and serious consequences.
The doctors at our regional dental clinic are ready to help. We use modern equipment, progressive therapeutic practices and always put the patient's comfort as a priority. Therefore, treatment of a darkened tooth will be quick and effective. Don’t let the disease lead to dangerous consequences - make an appointment with the dentist!
Diagnosis and treatment
Only a dentist can determine the exact cause of blackening of the tooth root. To identify the provoking factor, doctors use different diagnostic methods:
- inspection,
- dental radiography,
- electroodontometry.
The treatment regimen is drawn up individually for each patient, taking into account the clinical picture. If you have tartar, professional teeth cleaning is recommended. If the darkening of the enamel is caused by caries, it is necessary to clean the carious cavity and install a filling.
How to prevent plaque formation?
As you know, the best treatment for diseases is their prevention. To prevent unaesthetic plaque on your teeth from bothering you and making you suffer in the dentist’s chair, remember a few rules that will help keep your teeth white, strong and smooth:
- Give up bad habits. No matter how trivial it may sound, it is smoking and alcohol abuse that are the strongest enemies of enamel. Put out the cigarette once and for all, minimize the consumption of wine, beer, vodka and other strong drinks, and within a couple of months you will notice that the condition of your teeth has noticeably improved.
- Review your diet . Coffee, soda, sweet juice and black tea are not at all safe for your teeth, even if you drink them through a straw. And caramels, toffees, cakes and chocolates not only leave an unpleasant coating on the enamel, but also provoke tooth decay. Include more fresh fruits, vegetables, and herbs in your diet - these are the foods that allow you to cleanse crowns naturally; in addition, plants strengthen the body.
- Don't write off sugar-free candies and chewing gum . These products activate salivation.
- Remember the rules of personal hygiene . Brushing your teeth twice a day is the key to healthy enamel, crowns, gums and nerves. Choose your toothpaste carefully, brush every square millimeter, be mindful of the space between your teeth, and be sure to remove the film from your tongue.
Effective and safe teeth whitening and cleansing of surface enamel stains is provided by Asepta Plus gentle whitening toothpaste. This paste has a unique multi-stage teeth cleaning system that guarantees whitening for 4 weeks without damaging the tooth enamel. Hydroxyapatite and potassium citrate, which are part of the paste, mineralize weakened tooth enamel, prevent the occurrence of increased tooth sensitivity, and calamus and eleutherococcus extracts strengthen the gums and accelerate the regeneration processes of the oral mucosa.
When is the best time to remove a tooth?
It is more advisable to cure deep root caries, which develops against the background of severe inflammatory processes, by removing the tooth. There are a number of reasons for this:
- A diseased tooth is a source of infection. If caries was on one root, most likely it will develop in another area.
- A person will constantly be accompanied by bad breath, which is impossible to get rid of.
- Pathology makes teeth mobile, which prevents you from chewing food normally. Problems with the gastrointestinal tract may occur.
- There is a risk of infection entering the circulatory system, resulting in the development of general infections, including sepsis.
In each specific case, the doctor selects an individual treatment program based on medical indications, the patient’s age and financial capabilities.
What can you do about black teeth at home?
At home, it is possible to combat the darkening of teeth only in cases where the cause is external - plaque or deposits of tobacco tar. You can try to eliminate them with a highly abrasive toothpaste. But this means:
- Ineffective if the plaque is dense and hard;
- Cannot be used continuously as abrasive particles damage tooth enamel.
We do not recommend using home teeth whitening complexes offered by sellers on the Internet. They usually contain aggressive components that, together with plaque, destroy tooth enamel.
Professional help
Treatment begins with diagnosis and determining the causes of the pathology. After eliminating the causes that provoke the darkening of the enamel, appropriate treatment is prescribed.
The method of treating cervical caries depends on the stage at which the pathology was noticed:
- At the dark spot stage, remineralizing therapy is used: the tooth is cleaned of soft plaque and hard dental deposits, and the affected area is covered with an application containing fluoride.
- In case of superficial and medium caries, the affected area is prepared, after which the tooth is filled.
- At the stage of deep caries, as a rule, the pulp is removed and the canals are cleaned. After this, the tooth is filled.