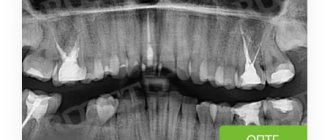
Many patients in dental clinics are already well acquainted with orthopantomography - a diagnostic radiographic examination that allows one to assess the condition of the dental system. A panoramic digital dental photograph is taken by rotating two x-ray-emitting and x-ray-receiving plates in opposite directions around a person's head. In this case, a flat panoramic image of both jaws is obtained on film or on a computer monitor.
Benefits of orthopantomography
- During the study, the patient receives a minimal dose of radiation - the same as he could receive in 30 minutes of travel along one of the trolleybus routes in Moscow.
- A quick and absolutely painless diagnosis has no contraindications.
- After a short period of time required to type the text of the report and print it out, the result is given to the patient.
- If necessary, you can get prompt advice from a specialist on site.
Detailed visualization of bone tissue and teeth makes it easy to diagnose existing pathologies and prescribe adequate treatment for teeth and gums. What information is revealed in the image to a specialist?
What does an MRI photo of the spine look like?
MRI of the thoracic spine (sagittal projection, T1 VI)
Magnetic resonance imaging images display the internal structures of the area of interest in three planes. Each image represents one slice; there are several of them on a printed MRI photo.
Normally, the vertebrae are smooth and there are no injuries. The fibrocartilaginous discs, which act as shock absorbers, do not protrude, have a standard height, and have no signs of degeneration. The spinal cord looks like a white cord in the photo without visible distortions or other changes.
The spinal column includes: cervical, thoracic, lumbar, sacral and coccyx. The pathological process can develop in any area or cause total damage.
MRI of the spine is performed to make a diagnosis, as part of dynamic monitoring of the disease, as a preoperative assessment of anatomical features, etc. Magnetic resonance imaging has advantages over CT in identifying changes in soft tissue structures: ligaments, synovium (inner lining of the articular membrane), cartilage, nerve trunks, muscles.
MRI of the spinal column: disc herniation L4-L5 (sagittal plane, T2 VI)
In pathological processes, images may show:
- curvature of the spinal column - scoliosis, lordosis, kyphosis;
- malignant and benign neoplasms (a biopsy is performed to verify the tumor);
- metastasis to the vertebrae;
- cystic cavities;
- vertebral displacements and fractures, sprains, long-term consequences of injury;
- protrusions, degenerative changes (spondylodiscitis, osteochondrosis, etc.), hernias, signs of involvement of spinal roots in the pathological process;
- endplate damage;
- myeloischemia;
- areas of narrowing of the spinal canal, compression or damage to the spinal cord, etc.
Magnetic resonance scanning of the lumbosacral spine: multiple hemangiomas (sagittal plane, T1 VI)
Interpretation of MRI results includes assessment of:
- lesions with a pathological MR signal (in areas of subchondral sclerosis, with disc prolapse, narrowing of the intervertebral foramina, damage to the nerve roots, in the area of edema, inflammation, etc.);
- density of the posterior longitudinal ligament;
- configurations of the bodies of the visualized vertebrae: - height, structure, surface (absence of osteophytes - bone growths, Schmorl's hernias), condition of the supporting platforms, etc.;
- dural sac (protective membrane of the spinal cord);
- spinal axis at the level being studied;
MRI: intervertebral disc herniation L4-5 (axial projection, T2 VI)
- dimensions of the spinal canal;
- facet joint gaps;
- structures, contours, diameter of the spinal cord;
- condition of paravertebral soft tissues, ligamentous apparatus;
- blood supply to the spinal cord, etc.
When deciphering the results of an MRI of the spine, changes in neighboring organs may come into view; the doctor will necessarily reflect this information in the study protocol.
What does an orthopantomogram show?
The overview photograph is a mirror image of the dental system: its right side is shown on the left, and the left side on the right. To facilitate orientation, the image is often marked: L and R (left, right).
To number the teeth, the image is divided into 4 segments. The 2 top ones - left and right, are “tens” and “twenties”, and the 2 bottom ones, the same left and right, are “thirties” and “forties”. The teeth are numbered starting from the center of the dentition, so in the center at the top there are incisors 11 and 21, and at the bottom - 41 and 31, and the row ends, as a rule, with wisdom teeth with numbers 18 and 28 at the top and 48 and 38 at the bottom.
In addition to the dentition, the following images are clearly visible in the panoramic image:
- mandibular canal with neurovascular bundle;
- maxillary sinuses and nasal passages;
- TMJ - temporomandibular joints;
- fillings and sealed canals (for this purpose, radiopaque components are introduced into the filling materials);
- wisdom teeth, supernumerary teeth, and in a child’s photograph - the rudiments of permanent teeth;
- hard palate with zygomatic bones, hyoid bone, nasal septum, conchae and other structures.
What program should I use to open MRI images?
MRI: fracture of the odontoid process of the second cervical vertebra (sagittal plane, T2 VI)
To open MRI images, you will need a special program (DICOM Viewer, RadiAnt, etc.), which can be downloaded on the Internet. Sometimes there is a file on the electronic media to install the application: run it following the instructions.
You must insert the CD into the drive or memory card into the appropriate slot on the computer. With the latter, a problem may arise due to the lack of a suitable connector; in such a situation, additional components will be required - a card reader and a USB cable.
After connecting the electronic media, you need to wait a while - the operating system must detect the disk or card and install the driver. An autorun program will appear on the screen in which you should open the folder to view files. If this does not happen, go to the “Start” menu, select “My Computer”, after the window appears, find “Devices with removable storage” and left-click on it.
You can view photos of an MR procedure as individual images or as a series of frames.
“The doctor can describe the study wherever it is convenient for him”
"IT'S A BOTTLE NECK"
– The order states that the feasibility of having a radiologist position in the clinic is determined by the head.
Does this mean that radiologists will begin to be transferred en masse to remote centers and will the staff of doctors be reduced in this case? - No, quite the opposite. All radiation diagnostics worked according to order No. 132 of 1991. They have been trying to write a new regulation for the last eight years, there were a lot of discussions, and finally the order appeared. The document establishes the possibility of licensing a department that does not provide emergency care, but operates in primary care without the presence of a radiologist.
For example, a dental clinic has X-ray equipment, but de facto there is no radiologist there at the moment. Is a radiologist needed for examinations? No. We all know that a huge number of dental X-ray examinations are done without a doctor - in most cases they are carried out not by a dentist, but by a nurse. In relation to dental clinics, all this has been working for a very long time. But the order clarified that the study should be described in the recording of a consultation with a specialized specialist. This practice can be used in other areas of medicine.
– That is, the presence of a radiologist during research is not always necessary?
- Exactly. When a patient comes for a fluorography or mammogram, in most cases the doctor is not there. When a patient comes for a computed tomography or magnetic resonance imaging scan, in at least half of the cases there is no doctor there either. The doctor may be located somewhere in an adjacent room or remotely. And this practice is already widespread in federal, private and municipal clinics.
For the first time, the order of the Ministry of Health recorded the possibility of conducting research by an x-ray technician - at the same time, we were preparing a professional standard for such a specialist, and the document has already been released. The professional standard clearly states that the x-ray technician conducts the examination and, among other things, administers the contrast agent. We are making up for what was lost in previous years.
I have repeatedly observed in medical organizations how a doctor himself performs a study on a device, and then goes to describe this study. This is a bottleneck: in this way it is impossible to ensure the utilization of equipment, nor to maintain the normal quality of research and descriptions, nor to train doctors in anything else. Because they are overly busy, working both for the laboratory assistant and for themselves.
At the Moscow Radiation Diagnostics Reference Center there are many elderly doctors who find it really difficult to work in clinics. And here an older doctor works, describes research, earns as much as he can describe. And people calmly understand both the workstation and the software. Therefore, telemedicine is also an opportunity to provide a workplace for both elderly specialists and people with disabilities. This is a huge advantage.
– How will the distribution of responsibilities between the radiologist and the x-ray technician change after the order comes into force?
– Previously, everything was focused on the radiologist, which from an economic point of view is unjustified and expensive. In fact, radiologists in a huge number of areas have not been directly involved in research for a long time.
Life has changed. And the new order of the Ministry of Health officially records what actually exists in practice - conducting research independently by x-ray technicians and describing the research by radiologists. There is an absolutely correct redistribution of the load among functional responsibilities. The radiologist primarily does what he was trained to do—interpret the results of the study.
The doctor can do this while being directly next to the device. But this is optional. The practice is very different. Somewhere there are complex patients with whom the radiologist finds something out on the spot, somewhere there is a standard examination, and the radiologist on the spot has nothing to do. Accordingly, a doctor can describe studies, including remotely - from a neighboring office, from another floor, from another building and even from another medical institution, from another legal entity. The creation of such a structure as a center for remote descriptions is also included in the order.
From an economic point of view, it is absolutely correct when simpler functions are performed by specialists with secondary medical education, that is, x-ray technicians, and expert functions that require communication with clinicians and discussion of complex patients are performed by doctors.
– The order makes it possible to appoint an ultrasound diagnostic doctor to the position of head of the radiology department. What motivated this maneuver?
– This practice is already spreading very widely, which is very correct, since it leads to greater teamwork and a more rational choice of diagnostic methods. The separation of X-rays and ultrasound is irrational: radiologists did something, ultrasound doctors did something, and then the doctor who referred the patient for examination begins to compare all this with each other, to understand everything. When all this is done in one department, the internal work of analyzing and choosing methods begins - when, who and what is best done. And the head of such a complex department becomes responsible precisely for the rational selection of diagnostic methods for referring doctors.
I believe that ultrasound diagnostic doctors should have basic skills in interpreting X-ray and CT examinations according to the professional standard. The radiologist, in turn, must be able to do a basic ultrasound examination so that, for example, in the emergency department he can conduct both an X-ray examination and an ultrasound scan for a seriously ill patient.
“WE WILL COME TO LICENSING THE WORKPLACE”
– How much will radiation diagnostics itself change in connection with the creation of a network of reference centers provided for in the order?
– Using the reference center model will not reduce the number of doctors. The volume of research is still growing, and doctors are simply starting to do their core work. They stop spinning like a squirrel in a wheel - they wish they could process even more research faster - no, they start doing exactly what they understand in accordance with their specialization. Some people know better the pathology of the lungs, others know the pathology of the abdominal cavity, others are closer to the study of the temporal bones and sinuses of the brain. There are already up to ten subspecializations within radiology in the world. In Europe, there is an official specialization called “neuroradiology” or “neuroradiology” - those who are narrowly involved in the study of the brain and spinal cord. There are official specializations: “oncoradiology”, “radiation diagnostics of the head and neck”, “cardiothoracic” and so on.
The reference center and remote reporting model allows the study to be transferred to a doctor who has a better understanding of a particular topic. The point of this entire event is to provide each patient with an expert opinion.
This is the teleradiological model. It won't replace everything. This does not mean that in the future all doctors will move to reference centers. A reference center is a resource complex that can work in several regions and serve a large number of organizations. There are radiologists who work in hospitals, in-patient departments, in clinics using analog equipment, using scopic equipment - where it is necessary to do an examination of the esophagus or stomach, which is actually done by a doctor. And a significant part of doctors work remotely.
Gradually, I think, we will also come to a model where workplaces, including remote ones, will be licensed. This is important not only for radiation diagnostics, but also for remote interpretation of ECG and functional diagnostics.
Now you can license a specific site, a specific building, obtain a sanitary and epidemiological certificate, and in some regions they still require you to first obtain a SEZ for the radiation source and only then - a SEZ for the type of activity “radiology”. Moscow Rospotrebnadzor is sympathetic to the development of technology, and we, for example, at the Moscow Reference Center received a sanitary and epidemiological certificate for activities without a source.
Gradually, the following is happening in medicine: all diagnostic methods are moving closer to the patient - what is called the point of care, that is, where the patient is, we do the diagnosis. Many mobile devices are appearing. For example, in reserve hospitals launched for patients with a new coronavirus infection at hospital sites, there are mobile CT scanners and mobile X-ray machines. And at the same time, the doctor’s functions, thanks to telemedicine technologies, also go to where the doctor is. All? No, of course not all. But this is one of the very important components in medicine, when the patient is examined where he is, and the doctor can describe the examination where it is convenient for him.
– How do remote consultation centers conduct quality control of radiology departments?
– The traditional quality control organization is structure, processes and results. The Moscow Center for Diagnostics and Telemedicine, formed back in 1996, is gradually mastering all these functions. What is structure quality assurance? This means the right equipment, settings, consumables, properly trained specialists, the right directions for research, information systems. Our center has been involved in the design of diagnostic departments and in monitoring equipment after it has been assembled and installed for decades.
The center contains an accredited testing laboratory in its structure. We are involved in checking the quality of projects, in calculating doses - this ensures the safety of diagnostics, we calculate doses in adjacent rooms and directly at the workplace, that is, we make sure that the device is installed correctly, the room is designed correctly and is not a danger to others.
The development of infrastructure through the information system is also something the center does. That is, we work hard to ensure that the structure and base of diagnostic departments are effective. One of the new achievements of Moscow healthcare is the standard of equipment for clinics and hospitals. Magnificent absolutely standard, well-developed. For the first time in several decades, such a clear management scheme for the distribution of all kinds of equipment has been formed at the regional level. With equipment requirements, with calculation of needs. The standard has already been published, it includes requirements for all types of diagnostic equipment. And according to this standard, procurement takes place according to the life cycle model.
Secondly, processes – we touch upon information systems. This is the description template that the doctor uses. This is the same ERIS system that provides business processes, because any informatization is the digitization of business processes. The laboratory technician did the research, it is automatically transferred to the doctor for description, and then the quality of this description is monitored - selectively or totally, depending on the level of the specialist.
Processes also include methodological recommendations, which we also develop in large quantities; they are approved by the Moscow Department of Health and are further transmitted through educational programs. Processes are SOPs, standard operating procedures that X-ray technicians use, these are checklists.
Finally, the results are the percentage of correct diagnoses, and we monitor this through the X-ray audit system. The results include the number of cancer tumors detected and what we do in screening programs. The results also include the correctness of the research descriptions and their compliance with the template, that is, a certain standard. The results, in the end, are the loading of the equipment and how rationally it was selected. The results are the waiting times for the studies by patients.
For example, in 2015, the average turnaround time for CT and MRI scans in Moscow clinics was four to five days. Apparently, the doctor came to the clinic once a week and described the accumulated studies. Now, with the help of the reference center, it takes doctors less than an hour to describe the study, because there is no dependence on the availability of a doctor on site in the medical organization. This is a huge step forward.
When the goal at the federal level is to reduce the duration of diagnosis, it is impossible to simply say to everyone: “Let’s work faster.” But when there is an information system and a clear research life cycle appears, then you can begin to customize this life cycle.
– How are things going with the implementation of remote advisory centers in the regions?
– There are regions that create the so-called CAMI – Central Archives of Medical Images. But this model is not very functional for teleradiology, because it usually involves the creation of a single repository into which everything “falls”, but to which doctors do not have access. These are the problems faced by many regions that believe that for radiological diagnostics it is enough to create a CAMI. But this is not always effective.
There is also, for example, PACS - a system for storing and transmitting medical images. Above the PACS there is a radiological information system - RIS, in which radiologists and x-ray technicians interact. In RIS, you can create conclusions in collaboration, form first and second opinions. There are description templates and remote audit functionality. Various automatic analysis algorithms can be connected to the RIS; the system has reference books and nomenclatures of types of research, and so on. This is a very large information system. And in the regions, very often they only make PACS, a “storage room”, as they say. And all functionality for interaction is omitted. And it turns out that the system does not work as it should.
Some regions - Krasnodar Territory, Krasnoyarsk Territory, Sverdlovsk Region, Tatarstan, Sakhalin - are creating systems specifically for remote interaction between doctors. All this is gradually developing. Regional information systems are also appearing, in which doctors are starting to work, for example, in the Voronezh region. There are perfectly set up processes when the results of laboratory tests are brought from regional clinics to the central clinical diagnostic center. Or even the samples taken from patients were first brought to the central CDC, and then they began to transport X-rays from small clinics. Then they introduced an information system and began transmitting laboratory tests, ECGs, and radiology images.
Such systems are gradually appearing in the regions. The problem is that after they are installed, sometimes the system provider changes, and then everything changes. Because the PACS manufacturer is changing, devices are being reconnected, and the interface is completely changing. It also turns out that the new provider that won the tender cannot provide all the functionality. This is a huge difficulty, which, apparently, will be solved for the regions by the Ministry of Health through the creation of uniform functional requirements for such information systems.
“DIAGNOSTICS SHOULD BECOME A COMPREHENSIVE SPECIALTY”
– How are research fees sent to a remote advisory center for decoding charged?
– In 2022, the Ministry of Health included remote description in the nomenclature of studies, created such a reserve of X-ray studies so that tariffs could be made for them. Not all regions took advantage of this.
In some regions, tariffs have appeared, although they are still very different - in some places it can be 180 rubles, in others 400 rubles for the description of one study. But in total, less than a dozen regions in Russia are following a similar path. This is a very complex, huge scientific and methodological work.
That is, tariffs according to which research is transferred to remote description have appeared. But this only emphasizes that what is happening is not a reduction in the number of specialties, but a redistribution of functions for describing research from one organization to another. Radiologists still remain a specialty in short supply.
- Why?
– For many years, it was believed that radiologists were in short supply because they worked and continue to work for x-ray technicians. I'm talking about Russia in general. And since they work for laboratory assistants, they are in short supply. Because they are not engaged in their work, but in the functions of paramedical personnel.
But x-ray technicians are also in great demand; clinics are looking for them. The labor market, one might say, has stirred up, because more functional requirements have appeared for the head of the department, and there is a need for doctors who can actually form expert opinions and work with a pool of modern technologies.
– The order states that one of the main functions of the X-ray department is to conduct hybrid studies. Does this involve performing positron emission tomography?
- Certainly. This is not yet obvious in the legislation, but where is practice heading? Firstly, historically there were departments of radiology or radionuclide diagnostics, in which radiologists worked. Those who work with radioisotopes and conduct various studies of the heart, thyroid gland, and skeletal bones. This specialty has always remained quite isolated.
Hybrid methods began to appear. It is logical that hybrid departments should gradually appear, in which there is both equipment, for example, PET/CT. Of course, not all radiologists will like this definition, but for me PET/CT is still CT/PET. In the first place there is a CT scan - a full scan of the patient’s entire body, including with contrast agents, and with an additional PET image, which helps to more accurately determine a particular metastasis and how much of the body is damaged in a person. The competencies required for this are knowledge of the basics of CT scanning, the ability to interpret various changes in the body, and at the same time an understanding of the principles of distribution of various radiopharmaceuticals, for example, fluorodeoxyglucose, which is now used in approximately 95% of all PET studies. Basically, in ordinary practice, this is done by a radiologist who studies the dynamics of an oncological patient. And a radiologist can additionally master the specialty of “radiology” in order to interpret PET. I did this myself - I trained in radiology to understand PET, in addition to my CT knowledge. And now I know many radiologists who specialize in radiology.
Accordingly, when such equipment appears, it is correct that all this is collected where oncology patients come. Not “go to another department,” but “come, they will do everything for you here.” And these results will be interpreted comprehensively, and a radiologist can do this: look at PET/CT, MRI studies, compare them and give the oncologist a full conclusion on the tumor board. Already now, absolutely officially, according to orders, decisions regarding the treatment of cancer patients are made by the tumor board. This means that the radiologist must submit a comprehensive report to the tumor board. There should not be such a thing that an ultrasound doctor gives one thing, a CT and MRI doctor gives another, and a PET/CT doctor gives a third. No, the radiologist must provide all this data.
Therefore, it is possible that PET interpretation for the subspecialization “oncoradiology” will appear in the professional standard of a radiologist. On the other hand, the interpretation of CT scans should appear in the professional standard of a radiologist. That is, there will be cross-skills. And the department can contain both traditional X-ray and hybrid equipment. For what? For the convenience of the patient, for the quality of diagnosis, for uniform examination of cancer patients.
– So the next update to the regulatory framework may be related to regulating the activities of the radiology department?
- Yes. There are no rules for radiology yet. They have been prepared, but not yet approved, and are under consideration by the Ministry of Health. And so far the specialists are largely scattered. But this is all diagnostics, and it should act as a comprehensive specialty. Because it is categorically inconvenient, for example, for an oncologist, to refer a patient separately for ultrasound, CT, MRI, PET/CT and then collect all these conclusions and compare them with each other. There must be unity.