Treatment methods for bacterial tonsillitis
Modern medicine uses two methods of treating bacterial tonsillitis - surgical and conservative.
Regardless of the stage and type of disease, you should not self-medicate. Since the drugs that helped cope with the disease once, the next time they may not cope with the infection. Therefore, you should definitely consult a doctor. The doctor at the ENT clinic will conduct an examination, prescribe the necessary tests (culture of flora from the throat) and prescribe a prescription for effective medications.
Bacterial tonsillitis in adults can only be cured with complex therapy, which combines various drugs for symptomatic therapy. In addition to drugs aimed at combating pathogens, medications are also prescribed that help reduce the intensity of accompanying symptoms, for example, to reduce body temperature and eliminate headaches.
In order to reduce a fairly high temperature (above 38.50C), you need to take one of the following medications:
- Ibuprofen;
- Paracetamol and others;
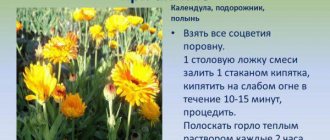
In a child, hyperthermia is often accompanied by nausea and vomiting. Traditional methods will help cope with hyperthermia - wiping the face and body with a damp towel or alcohol solution. During treatment of bacterial tonsillitis, bed rest and a gentle diet are mandatory. In case of intoxication, it is recommended to drink a lot of fluids (herbal infusions, compotes, milk, teas).
Based on the results of an analysis of the throat flora, the pathogen is determined and an antibiotic is prescribed, the action of which is aimed at combating this particular bacterium. For severe headaches accompanying bacterial tonsillitis, painkillers are prescribed - Aspirin, Ketonal, Nimesulide, Analgin.
Painful sensations in the throat are dulled and the tonsils are simultaneously disinfected when using the following medications:
- Givalex;
- Yox;
- Theraflu;
- Hexoral;
- Inhalipt.
Lollipops that reduce inflammation - Grammidin, Neo-angin, Decathylene, Strepsils - also cope well with this task. Solutions for gargling the mucous membranes of the throat - Chlorhexidine, Furacillin solution.
The surgical treatment for bacterial tonsillitis involves surgical removal of the tonsils. It should be borne in mind that these organs are of great importance for immunity.
Forms and classification of tonsillitis in children5
It should be noted that there is fundamentally no difference between adult and child forms.
The disease is divided according to:
- By shape
- By pathogen
- According to the form of the lesion
| CLASSIFICATION | A COMMENT | ||
| classification: | According to the form they are distinguished: | a comment: | - acute tonsillitis or sore throat - chronic tonsillitis |
| classification: | According to the causative agent, tonsillitis can be: | a comment: | Bacterial: - beta-hemolytic streptococcus A and other groups - staphylococcus - pneumococcus - moxarella Viral: — Influenza and parainfluenza virus — adenovirus — coronavirus — Epstein-Barr virus — enteroviruses — Coxsackie virus — herpes virus types I and II Fungal: mold fungus Candida albicans. As noted above, tonsillitis may be a manifestation of another disease: — measles — rubella — scarlet fever — mononucleosis |
| classification: | According to the form of the lesion: | a comment: | - catarrhal - follicular - lacunar - phlegmonous - ulcerative-necrotic - mixed form |
Most often, children suffer from the viral form of tonsillitis.6
treatment of bacterial tonsillitis at the clinic of Dr. Sichinava
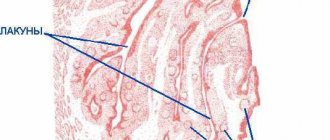
The specialized ENT clinic of Otto Sichinava uses advanced methods of treating bacterial tonsillitis without surgery. The procedure consists of washing the lacunae of the tonsils with an antiseptic solution. For this, a special gun with a thin tip (author’s development) is used, which delivers the solution directly into the lacuna.
Treating bacterial tonsillitis in children is much easier if the child does not feel pain. The advantages of this method are absolute painlessness and effectiveness. Treatment of bacterial tonsillitis consists of 10 procedures, after which the swelling and hyperemia of the tonsils decreases, and the appearance returns to physiological norms.
By seeking help from the clinic of Dr. Otto Sichinava in Moscow, you are guaranteed to be cured of pathological processes in the tonsils.
Prevention of tonsillitis in children
Regular walks in the fresh air, sports and hardening.
The children's diet must contain a large amount of fresh vegetables and fruits, herbs, and low-fat protein foods. Eating fatty, fried foods, fast food, and fast carbohydrates is not recommended for children.
Parents need to carefully monitor their child’s personal hygiene: regularly wash their hands and brush their teeth.
At home, it is recommended to maintain optimal humidity (50-60%) and air temperature (no more than 21 degrees) and carry out daily wet cleaning with room ventilation.
What symptoms indicate a child has a sore throat?
To assume that a child has a dangerous form of streptococcal tonsillitis, one or more of the following symptoms must be present:
- Temperature ≥ 38.3°C
- Season: late autumn, winter or early spring.
- The child does not have a cough
- The child's age is from 5 to 15 years.
- Recent exposure to someone with a sore throat
- Difficulty breathing or swallowing
- The child's voice sounds muffled
- Stiffness in the neck or difficulty opening the mouth
What is "angina"?
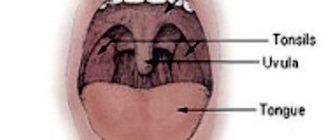
Immunity is the body’s ability to recognize “strangers” and fight them. “Strangers” are cancer cells and infectious agents. In the body there are groups of cells that perform certain common and similar functions; these cells are called tissue. Examples of tissues are bone, muscle, nervous, glandular. There are cells responsible for the production of immunity and form the so-called lymphoid tissue. Lymphoid tissue is present in the intestines (both small and large), in the bone marrow, and the thymus gland is entirely composed of it. It is not difficult to see lymphoid tissue. To do this, you need to go to the mirror and open your mouth wide. In the depths of the oral cavity, behind the arches that limit the entrance to the pharynx, there are semicircular formations - tonsils.
Tonsils consist of lymphoid tissue, are one of the main organs of the lymphoid system, participate in the development of immunity and very often become inflamed. Why often? Yes, because all substances that enter our body - both air and food - come into contact, first of all, with the tonsils. Here, in the oral cavity, to the esophagus and stomach, to the larynx and lungs - the tonsils are the vanguard of the immune system. It is not surprising that this squad has a great time and often gets it.
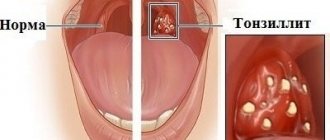
Inflammation of the tonsils is called tonsillitis (tonsilla in Latin). The most common cause of tonsillitis is the well-known acute respiratory viral infections, the common symptoms of which, in addition to fever, cough and runny nose, are a “red” throat and pain when swallowing.
The number of microorganisms that can cause an inflammatory process in the tonsils is in the dozens. It is not surprising that tonsillitis is a common symptom of many infectious diseases.
At the same time, there are two microorganisms - streptococcus and staphylococcus, which affect the tonsils especially often and in a special way. The disease begins very quickly, with a high temperature, sharp pain in the throat, and pustules (plaques) appear on the surface of the tonsils. This is a sore throat. The frequency with which these two microbes cause it is approximately as follows: 80% - streptococcus, 10% - staphylococcus and 10% - staphylococcus + streptococcus.
Once again the symptoms of a sore throat:
- acute onset, fever;
- general intoxication (weakness, chills, sweating, loss of appetite, headache);
- inflammation of the tonsils - increase in size, redness, plaque, pain in the pharynx, sharply increasing when swallowing;
- enlargement and tenderness of the lymph nodes - anterior cervical (down from the ear), near the angle and under the lower jaw.
In all organs and tissues, in addition to blood vessels (veins and arteries), there are lymphatic vessels that collect a special interstitial fluid - lymph. No part of the human body can even approximately compare with the tonsils in terms of the number of lymphatic vessels. It is not surprising that the purulent inflammatory process is immediately accompanied by a pronounced reaction of those lymph nodes that collect the lymph flowing from the tonsils.
The word “angina” itself owes its origin to ancient Greek doctors (ango - to choke, squeeze). The ancient Greeks had no idea about viruses and bacteria; by the word “angina” they understood all diseases accompanied by inflammation of the tissues of the pharynx and accompanied by impaired swallowing and breathing. Modern doctors treat viral and bacterial infections differently. Each specific disease accompanied by tonsillitis has its own specific methods of therapy.
That is why it is absolutely illiterate to call a sore throat any disease in which there is redness of the throat and pain when swallowing.
SOLISH is an acute infectious (contagious!) disease. It is the damage to the tonsils that determines the severity of the disease in angina.
Sore throat is a certain complex of symptoms, and we described this complex above. And redness in the throat, and pain, and plaque on the surface of the tonsils, and the reaction of the lymph nodes, i.e., all the symptoms typical of sore throat, can occur with diphtheria. The same symptoms can occur with a not at all rare viral disease - infectious mononucleosis. But in addition to the symptoms described, diphtheria affects the heart, kidneys, and nervous system; for infectious mononucleosis - all lymph nodes, liver, spleen. Sore throat is treated with antibiotics, diphtheria with anti-diphtheria serum; for infectious mononucleosis, neither antibiotics nor serum are effective.
The significance of the information provided is to once again emphasize: tonsillitis is not a bunch of all sorts of different diseases, tonsillitis is a specific disease that has specific symptoms and is caused by a specific microbe (usually streptococcus).
It is very important to note that angina is an acute disease. It cannot last for months, you cannot have it every month. People get infected with tonsillitis - from a person with tonsillitis or from a carrier of streptococcus. You can't get a sore throat just by getting your feet wet. You must first get your feet wet, and then find a person from whom you can get infected (of course, it is easier to get infected after hypothermia).
Sore throat, like any acute streptococcal infection, has two important features:
- tonsillitis can be treated very successfully and fairly quickly with the correct and timely administration of antibiotics;
- A sore throat that is not treated at all or that is treated incorrectly very often gives complications, since it is streptococcus that affects the heart, joints and kidneys.
Once again, please note: almost 100% of all rheumatic diseases and glomerulonephritis are a consequence of “ordinary” sore throat!
What studies confirm that a child has a sore throat?
If there is a suspicion that the child may have streptococcal or the child may have streptococcal tonsillitis or scarlet fever, tests may be carried out to confirm the diagnosis: a rapid test (Strep test) and culture. For both types of tests, the doctor takes a swab from the back and sides of the child's throat. The results of the rapid test are obtained within a few minutes, and the culture will be ready within two days. If the research confirms the streptococcal nature of the disease, the child is prescribed antibiotic therapy. If the result of the Strep test is negative, then an additional culture is done to avoid false negative results.
Specific features of bacterial sore throat
It is often difficult for parents to distinguish bacterial tonsillitis from other types of acute tonsillitis. Because of this, the patient’s condition often worsens.
- A sore throat caused by bacteria can be recognized by the following clinical picture:
- The lymph nodes in the neck and lower jaw become inflamed. On palpation they are sharply painful.
- There is no mucus or redness on the back of the throat.
- Pus accumulates on the tonsils in the form of white or gray-green dots, but it does not extend beyond them. With a viral sore throat, pus spreads over the entire surface of the throat and surface of the mouth.
Sore throat caused by bacteria differs from other types of acute tonsillitis in that the runny nose and cough are mild, diarrhea, nausea, vomiting and indigestion are absent.
Description of the disease
Tonsillitis is an inflammatory disease common in childhood, in which the source of inflammation is localized in the palatine tonsils.
Most often the disease occurs in children 5-10 years old, but it can also develop at an older/younger age. Tonsillitis is infectious in nature, that is, it occurs when bacteria, viruses and (less often) fungi enter the child’s body. There are two forms of tonsillitis - acute and chronic. Acute tonsillitis is nothing more than a common sore throat. The pathology is characterized by a rapid course and pronounced symptoms. The chronic form of tonsillitis has an asymptomatic clinical picture and occurs with frequently recurring inflammation of the tonsils or as a result of untreated tonsillitis.
Tonsillitis brings significant discomfort to the child - the patient suffers from severe sore throat, high body temperature, and the inability to eat and drink normally. In addition, in the absence of treatment, a number of complications can occur in the organs and systems of the body: sepsis, rheumatic diseases, myocarditis, pyelonephritis, vasculitis, etc.
A-STREPTOCOCCAL TONSILLITIS: clinical significance, issues of antibacterial therapy
What is meant by acute tonsillitis? Why is antibacterial therapy necessary for GABHS tonsillitis? Which antibacterial agents to choose?
Acute tonsillitis (tonsillitis)1 is a disease that is characterized by acute inflammation of one or more lymphoid formations of the pharyngeal ring (usually the tonsils) and is one of the widespread infections of the upper respiratory tract.
The most significant bacterial causative agent of acute tonsillitis is group A β-hemolytic streptococcus (Streptococcus pyogenes, GABHS). Less commonly, acute tonsillitis is caused by viruses, streptococci of groups C and G, Arcanobacterium haemolyticum, Neisseria gonorrhoeae, Corynebacterium diphtheria (diphtheria), anaerobes and spirochetes (Simanovsky-Plaut-Vincent angina), extremely rarely - mycoplasma and chlamydia.
GABHS is transmitted by airborne droplets. Sources of infection are sick and less often asymptomatic carriers. The likelihood of infection increases with a high degree of contamination and close contact with the patient. Outbreaks of acute GABHS tonsillitis most often occur in organized groups (in preschool institutions, schools, military units, etc.). Mostly children aged 5-15 years are affected, as well as people of young working age. The highest incidence is observed in the winter-spring period.
The high incidence of the disease, the contagiousness of the infection, large labor losses entailing economic damage, the possibility of developing serious complications - all this indicates that the problem of GABHS tonsillitis is still quite acute in both scientific and practical aspects.
Clinical picture. The incubation period for acute GABHS tonsillitis ranges from several hours to 2-4 days. This disease is characterized by an acute onset with an increase in temperature to 37.5–39 ° C, chills or chills, headache, general malaise, sore throat, aggravated by swallowing; Arthralgia and myalgia are common. Children may have nausea, vomiting, and abdominal pain. A detailed clinical picture is observed, as a rule, on the second day from the onset of the disease, when the general symptoms reach their maximum severity. Upon examination, redness of the palatine arches, uvula, and posterior wall of the pharynx is revealed. The tonsils are hyperemic, swollen, often with a yellowish-white purulent coating. The plaque is loose, porous, and can be easily removed with a spatula from the surface of the tonsils without a bleeding defect. All patients experience thickening, enlargement and pain on palpation of the cervical lymph nodes at the level of the angle of the lower jaw (regional lymphadenitis). Blood tests show increased leukocytosis (9-12 109/l), a shift in the leukocyte formula to the left, accelerated ESR (sometimes up to 40-50 mm/h), the appearance of C-reactive protein. The duration of the peak period (without treatment) is approximately 5-7 days. Subsequently, in the absence of complications, the main clinical manifestations of the disease (fever, symptoms of intoxication, inflammatory changes in the tonsils) quickly disappear, and the peripheral blood picture normalizes. Symptoms of regional lymphadenitis can last up to 10-12 days.
The diagnosis of GABHS tonsillitis is confirmed by microbiological examination of a smear from the surface of the tonsils and/or the posterior wall of the pharynx. If the rules of sampling technique are followed, the sensitivity of the method reaches 90%, and the specificity - 95-99%. Methods of express diagnostics of A-streptococcal antigen in throat swabs, popular abroad, make it possible to get an answer in 15-20 minutes. At the same time, it should be emphasized that the cultural method does not allow differentiating an active infection from GABHS carriage, and modern rapid tests, despite their high specificity (95-100%), are characterized by relatively low sensitivity (60-80%), then there is a negative result of rapid diagnosis does not exclude streptococcal etiology of the disease.
Differential diagnosis of acute GABHS tonsillitis, based only on clinical signs, is often quite a difficult task even for experienced doctors. However, it should be noted that the presence of respiratory symptoms (cough, rhinitis, hoarseness, etc.), as well as concomitant conjunctivitis, stomatitis or diarrhea, indicate a viral etiology of acute tonsillitis. Unlike scarlet fever, acute GABHS tonsillitis is not characterized by any types of rashes on the skin and mucous membranes. With localized diphtheria of the oropharynx, plaque from the tonsils is difficult to remove, does not rub on a glass slide, does not dissolve in water, but slowly settles to the bottom of the vessel; After plaque removal, bleeding of the underlying tissues is observed. The anginal form of infectious mononucleosis, as a rule, begins with widespread damage to the lymph nodes (cervical, occipital, axillary, abdominal, inguinal), the symptoms of tonsillitis develop on the 3-5th day of illness, and a study of peripheral blood reveals leukocytosis with a predominance of mononuclear cells (up to 60 -80%). Simanovsky-Plaut-Vincent tonsillitis is characterized by mild signs of general intoxication and symptoms of unilateral ulcerative-necrotic tonsillitis, while the necrotic process may spread to the soft and hard palate, gums, posterior wall of the pharynx and larynx.
Since GABHS tonsillitis is inherently a self-limiting disease and can result in complete recovery (even in the absence of treatment) without any complications, some doctors still have doubts about the thorough supervision of such patients. It is completely unreasonable to give preference to local treatment (rinses, inhalations, etc.) to the detriment of systemic antibiotic therapy. This approach is in no way justified and can lead to very sad consequences for the patient.
Numerous literature data indicate that at the end of the 20th century there were significant changes in the epidemiology of GABHS infections of the upper respiratory tract and, most importantly, their complications, caused by the “revival” of highly virulent A-streptococcal strains. Thus, in the mid-1980s, in the United States, a country with the most favorable medical and statistical indicators, an outbreak of acute rheumatic fever (ARF) broke out, first among military recruits at a military base in San Diego (California), and a little later among children in the continental states (Utah, Ohio, Pennsylvania). Moreover, in most cases, children from families whose annual income exceeded the national average (that is, having a separate home, adequate nutrition, and the opportunity to receive qualified medical care in a timely manner) fell ill. It is noteworthy that the diagnosis of ARF was made late in most cases. Among the most likely causes of this outbreak, the so-called medical factor played a significant role. As GH Stollerman (1997) rightly noted, young doctors had never seen patients with ARF, did not imagine the possibility of streptococcus circulating in school groups, did not know about the decisive preventive value of penicillin, and often had no idea that antibiotics should be used for tonsillitis. Along with this, it turned out that in half of the cases, ARF was a consequence of GABHS tonsillitis, which occurred with an erased clinical symptom complex (satisfactory general condition, normal or subfebrile body temperature, a slight sore throat, disappearing after 1-2 days), when most patients did not sought medical help, but treated themselves without the use of appropriate antibiotics.
The results of studies of pharyngeal cultures performed in affected ARF populations in the late 1980s suggest the existence of “rheumatogenic” GABHS strains that have a number of specific properties. Among them, of particular importance is the presence in M-protein molecules of epitopes that cross-react with various tissues of the host macroorganism: myosin, synovium, brain, sarcolemmal membrane. These data support the concept of molecular mimicry as the main pathogenetic mechanism of streptococcal infection in ARF due to the fact that antibodies formed in response to streptococcal antigens react with the host's autoantigens. On the other hand, M protein has the properties of a superantigen that induces the effect of autoimmunity. The acquired autoimmune response may in turn be enhanced by subsequent infection with rheumatogenic strains containing cross-reactive epitopes.
In the late 1980s and early 1990s, reports of extremely severe invasive GABHS infection, accompanied by hypotension, coagulopathy, and multiorgan functional failure, began to be received from the United States and several Western European countries. The term “streptococcal toxic shock-like syndrome” was proposed to refer to this condition, by analogy with staphylococcal toxic shock. And although the main “entry gates” for this life-threatening GABHS infection were the skin and soft tissues, in 10-20% of cases the disease was associated with a primary focus localized in the lymphoid structures of the nasopharynx. In an analysis of invasive GABHS infections carried out in the United States in 1985-1992, it was found that the incidence curves of ARF and toxic shock syndrome of streptococcal origin were very similar in both time and amplitude.
To date, the true reasons for the mentioned “revival” of the highly virulent GABHS infection are still not fully disclosed. In this regard, the role of an accurate diagnosis and mandatory antibiotic therapy for GABHS tonsillitis (including its low-symptomatic forms) both in controlling the spread of these infections and in preventing complications has increased even more.
Treatment. Despite the fact that GABHS still retains almost complete sensitivity to β-lactam antibiotics, in recent years certain problems have been noted in the treatment of tonsillitis caused by this microorganism. According to various authors, the failure rate of penicillin therapy for GABHS tonsillitis is 25-30%, and in some cases even 38%. One of the possible reasons for this may be the hydrolysis of penicillin by specific enzymes - β-lactamases, which are produced by microorganisms - copathogens (Staphylococcus aureus, Haemophilus influenzae, etc.) present in the deep tissues of the tonsils, especially in the presence of chronic inflammatory processes in the latter.
As can be seen from table. 1, penicillin drugs remain the means of choice only in the treatment of acute GABHS tonsillitis. Today, the optimal drug from the group of oral penicillins seems to be amoxicillin, which is similar in antistreptococcal activity to ampicillin and phenoxymethylpenicillin, but is significantly superior to them in its pharmacokinetic characteristics, characterized by greater bioavailability (95, 40 and 50%, respectively) and a lower degree of binding to serum proteins ( 17, 22 and 80%). If the patient's compliance (performance) is questionable, as well as in certain clinical and epidemiological situations, a single injection of benzathine penicillin is indicated.
It is advisable to prescribe phenoxymethylpenicillin only to young children, given the presence of the dosage form in the form of a suspension, as well as somewhat greater compliance ensured through parental control, which cannot be said about adolescents.
Along with penicillins, cefadroxil, a representative of the first generation oral cephalosporins, deserves undoubted attention; its high effectiveness in the treatment of GABHS tonsillitis, as well as its good tolerability, have been confirmed in numerous clinical studies.
In case of intolerance to β-lactam antibiotics, it is advisable to prescribe macrolides (spiramycin, azithromycin, roxithromycin, clarithromycin, midecamycin). Along with high antistreptococcal activity, the advantages of these drugs are the ability to create a high tissue concentration at the site of infection, a shorter course of treatment (in particular for azithromycin), and good tolerability. The use of erythromycin, the first representative of this class of antibiotics, has now been significantly reduced, especially in therapeutic practice, since it more often than other macrolides causes undesirable effects on the gastrointestinal tract due to the stimulating effect of erythromycin on gastric and intestinal motility.
It should be noted that in recent years, from Japan and a number of European countries, there have been increasingly reports of increasing GABHS resistance to erythromycin and other macrolides. Using the example of Finland, it was shown that the formation of resistance is a controlled process. A widespread educational campaign among doctors in this country led to a twofold decrease in the consumption of macrolides and, as a consequence, to a twofold decrease in the frequency of GABHS strains resistant to the mentioned antibiotics. At the same time, in Russia, GABHS resistance to macrolides is 13-17% (Strachunsky L. S. et al., 1997). And this fact undoubtedly deserves the most serious attention.
Lincosamine antibiotics (lincomycin, clindamycin) are prescribed for GABHS tonsillitis only in case of intolerance to both b-lactams and macrolides. It is not recommended to widely use these drugs for this nosological form. It is known that with frequent use of oral penicillins, sensitivity to them from viridans streptococci localized in the oral cavity is significantly reduced. Therefore, in this category of patients, among whom there are many patients with rheumatic heart disease, lincosamines are considered as first-line drugs for the prevention of infective endocarditis when performing various dental procedures.
In the presence of chronic recurrent GABHS tonsillitis, the probability of colonization of the site of infection by microorganisms producing b-lactamases is quite high. In this case, it is advisable to carry out a course of treatment with inhibitor-protected penicillins (amoxicillin/clavulanate) or second generation oral cephalosporins (cefuroxime - axetil), and in case of intolerance to b-lactam antibiotics - lincosamines (Table 2). These antibiotics are also considered as second-line drugs for cases where penicillin therapy for acute GABHS tonsillitis is unsuccessful (which is more common when using phenoxymethylpenicillin). A universal scheme that ensures 100% elimination of GABHS from the nasopharynx does not exist in global clinical practice.
It should be noted that the use of tetracyclines, sulfonamides, co-trimoxazole and chloramphenicol for GABHS infection of the pharynx is currently not justified due to the high frequency of resistance and, consequently, low rates of treatment effectiveness.
Thus, in modern conditions, the issues of timely and high-quality diagnosis and rational antibiotic therapy for GABHS tonsillitis remain relevant. New antibacterial agents that have appeared in recent years have significantly expanded the possibilities of antimicrobial therapy for GABHS tonsillitis, but have not completely solved this problem. In this regard, many researchers have high hopes for the creation of a vaccine containing epitopes of M-proteins of rheumatogenic GABHS strains that do not cross-react with tissue antigens of the human body. Such a vaccine, in particular as part of the primary prevention of ARF, is very necessary, primarily for individuals with genetic markers indicating a predisposition to the disease.
Prescribing antibiotics for catarrhal tonsillitis and uncomplicated forms of chronic tonsillitis is not always justified, especially without a clear idea of the causative agent.
At these stages of the disease, not yet burdened by superinfection, homeopathy may be an alternative treatment. This is a regulatory therapy that affects self-regulation processes with the help of medications selected individually, taking into account the patient’s response. From the standpoint of classical homeopathy, sore throat and chronic tonsillitis are not local diseases, but private manifestations of constitutional weakness and hereditary predisposition.
The selection of components of the homeopathic drug "Tonsilotren" is based on such provisions, clinical studies of which in Russia have shown high efficiency and safety.
1 In foreign literature, the interchangeable terms “tonsillopharyngitis” and “pharyngitis” are widely used.
back
Pus plugs in the tonsils
“Congestion in the tonsils” is a separate problem, mostly hygienic, causing bad breath, sometimes also a feeling of pressure or a foreign body.
What is tonsillitis? It is a cast of food that has fallen into a lacuna (a kind of pocket) of the tonsil, tonsil epithelium and bacteria (most often fusobacterium nucelatum, the main bacterium of dental plaque). But this is not pus, since there are no dead leukocytes and bacteria underdigested by leukocytes.
The conditions for the formation of “plugs” are usually dry mucous membranes of the tonsils, which occurs when nasal breathing is impaired and/or air with low humidity.
Often, if you solve the problem with nasal breathing and the humidity of the inhaled air, then the “traffic jams” disappear by themselves.
What's the moral? If there are “traffic jams”, but no sore throat, then you should pay attention to the state of nasal breathing. And only if the problem persists even with a well-breathing nose, should you look for a solution in the palatine tonsils themselves.
Diagnosis of tonsillitis
Tonsillitis is a serious disease that requires timely diagnosis and individually selected treatment.
Self-medication can cause irreparable harm to children's health, therefore, if there is any suspicion of pathology of the upper respiratory tract, the patient should be shown to an experienced doctor. At the initial appointment, the ENT doctor will collect an anamnesis (medical history), clarify the symptoms of the disease, the duration of their presence, and any history of previous acute inflammatory processes. Then the specialist proceeds to examining the pharynx (pharyngoscopy) and palpating the lymph nodes. During the examination, the doctor uses a special instrument – a pharyngoscope, which allows a detailed examination of the condition of the child’s tonsils. If you suspect the presence of diseases concomitant with tonsillitis, you may need to consult a dentist, rheumatologist, pediatric cardiologist and other specialist doctors. To confirm the diagnosis and exclude possible complications, the small patient is sent to undergo a series of laboratory and instrumental studies:
- general and biochemical blood tests;
- general urine analysis;
- biochemical examination of a smear from the tonsils;
- radiography of the nasal sinuses;
- ECG of the heart.
The results of the research will allow the specialist to identify the true cause of the disease, determine the characteristics of the course of the disease and the presence of concomitant disorders in the child’s body.