Wisdom tooth extraction is a surgical procedure during which the third molar is removed from the dental socket.
This surgical intervention in uncomplicated cases is not particularly different from the removal of other teeth. The only thing that complicates it is the presence of a winding and long root system. The operation itself, with the exception of rare cases, is not a complex surgical procedure.
Wisdom teeth are considered rudiments, since they do not take part in the process of chewing food, due to changes in the diet of modern man.
They erupt at the age of 18 to 24 years. Previously, there were four of them in the jaw. Recently, cases have become increasingly common when molars are partially embedded or absent in the jaw altogether.
Cleaning them, due to their inaccessible location, is difficult. This contributes to the accumulation of plaque, which subsequently provokes the development of caries, damage to neighboring teeth, as well as various inflammatory processes in adjacent tissues.
Symptoms and signs
Symptoms that patients themselves complain about when problems with wisdom teeth occur:
- redness and swelling in the gum area;
- sharp or aching pain localized at the site of tooth eruption;
- the jaw opens poorly, the process is accompanied by nagging pain;
- feeling of discomfort when chewing food;
- bad breath;
- increased body temperature;
- painful swallowing.
If such symptoms occur, you must immediately consult a doctor who will conduct an examination, assess the situation and, if necessary, prescribe an x-ray.
Untimely treatment is fraught with aggravation of the situation, complicated by eruption or an inflammatory process in the area where the wisdom tooth is located. All this can lead to extensive abscess, phlegmon and osteomyelitis of the jaw.
Indications for surgery
There are a number of indications for wisdom tooth removal. Operations can be carried out planned or urgently.
Scheduled deletion
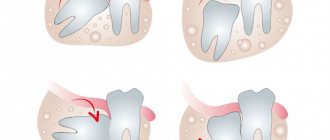
- Incorrect eruption. In this situation, the molars grow at an angle or horizontally. This can cause injury to the root system of teeth located nearby or to the gum tissue. In these cases, to preserve the chewing teeth, the wisdom tooth is removed.
- Cyst . The presence of a cyst near a wisdom tooth is an indication for its planned removal.
- Absence of an antagonist tooth . Also, a wisdom tooth is removed in cases where there is no “figure eight” on the opposite jaw. Because of this, a difference in pressure is created on the teeth, which is a risk of tooth protrusion.
- Caries . Often wisdom teeth emerge that are already affected by caries. These are the only teeth that no attempt is made to preserve in this disease. They are immediately removed.
- Partial or complete failure to erupt . A wisdom tooth embedded in the lower or upper jaw, but unerupted or not fully erupted, must also be removed.
- Inflammatory processes . Inflammation of wisdom teeth, due to their location, often spreads to the cheeks. A concomitant symptom is the formation of small ulcers on the mucous membrane around the tooth itself, followed by their growth.
Unscheduled surgery
Cases of immediate surgical intervention:
- severe wisdom tooth infection caused by a large abscess in the lower or upper jaw;
- tooth fractures due to mechanical impact.
Contraindications
Removal of wisdom teeth has its contraindications. These include:
- acute infectious diseases, for example, pneumonia, tuberculosis, tonsillitis, etc.;
- strokes, heart attacks, ischemic attacks, hypertensive crises (if a similar condition was observed in the patient not so long ago, the removal of the wisdom tooth should be postponed until the condition normalizes);
- blood clotting disorder (the operation can be performed after certain preparation).
In most cases, wisdom teeth are not removed for pregnant women, since during this period the use of antibiotics and analgesics is limited (due to the risk to the fetus).
Is it painful to have wisdom teeth removed?
Removing any teeth is a painful procedure and is always performed under anesthesia. Wisdom teeth are no exception, especially considering the fact that they have a lot of roots, so in the case of a simple removal, you will be offered local anesthesia; if complex removal of the “eight” is necessary, you will be offered general anesthesia or sedation.
The use of general anesthesia or sedation helps to carry out the procedure with minimal discomfort for the patient. You will sleep and will not feel pain, fear or stress. The patient is removed from sedation or anesthesia after complete completion of all manipulations to remove the wisdom tooth.
Diagnostics
Before removing a wisdom tooth, the surgeon needs to see a complete and accurate picture of its location. This is especially true in cases where the tooth has not erupted.
The specialist must prescribe an x-ray or orthopantomogram.
Before the operation:
- inspection;
- taking anamnesis;
- analysis of the received images.
Treatment
Depending on the picture and accompanying symptoms, the process of wisdom tooth removal is conventionally divided into simple and complex.
Easy removal
The operation begins with the administration of anesthesia.
During removal, specialists use forceps and elevators. No incisions are made for this type of intervention. The process of extracting a tooth from bone tissue lasts 2 to 10 minutes, depending on the location of the roots.
The resulting wound is treated with an antiseptic. If it is large, stitches are placed to reduce the risk of infection in the wound. A bandage with an anesthetic is applied to the area of manipulation, this is done to reduce bleeding.
Difficult removal
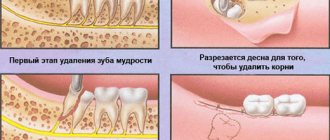
In the case of a complex operation to remove wisdom teeth, the necessary data is also collected and analyzed, and anesthesia is administered.
The operation is accompanied by dissection of the gums with a scalpel. To remove the tooth itself, it is cut into pieces using a drill. This is done to make it easier to remove. After removal, the resulting wound is treated with an antiseptic and then sutured.
Depending on the location of the tooth, the operation can take from 15 minutes to an hour and a half.
After the manipulations, regardless of their complexity, the doctor must consult the patient on wound treatment and, if necessary, prescribe medication.
Removal using ultrasound
In some cases, and with the appropriate equipment, a tooth can be removed using an ultrasonic scalpel. It allows for contactless intervention. Wounds with these manipulations heal faster, and the risk of complications is reduced.
Excision of a dental pocket with preservation of the tooth
There is a disease of the wisdom tooth in which its removal is called into question. This is an inflammation of the dental pocket, which is caused by bacteria that get under the gums. With this pathology, the doctor dissects the hood without affecting the tooth itself. The area of inflammation is treated with antiseptics.
The process of tissue healing and restoration, as a rule, proceeds quickly and the need for removal disappears. If the so-called pericoronitis has reached the stage at which ulcers form on the mucous membrane, the wisdom tooth is removed.
Mechanism of nerve injury
There are several types of nerve injury. The first and most common complication is direct mechanical injury from the instrument. Trying to remove the broken tip of the tooth, the doctor unnecessarily expands the boundaries of the hole with a drill and often touches the perineurium with a cutter. Also, strong pressure from the elevator on the bottom of the socket, working with root elevators “towards oneself” and “from oneself” leads to destruction of the wall of the mandibular canal and nerve injury. Clinically, at the time of injury, the patient experiences unbearable pain that can be compared to an electric shock with pain radiating to the teeth and lower lip. This type of injury leads to persistent paresthesia, which will last for several months; in some cases, complete restoration of sensitivity is not observed.
Another mechanism of nerve injury is associated with its compression (squeezing) by the tooth root during its luxation and traction. This mechanism is associated with the anatomically close, contact, location of the tooth root and the mandibular canal. In such patients, clinically and radiologically, the root of the impacted molar is part of the wall of the mandibular canal (Fig. 1,2). The root of the tooth in these cases can be the side wall of the canal, the upper wall, or surround the canal with a root bifurcation. The author had to observe a case when the mandibular canal passed through an impacted tooth, while all the walls of the mandibular canal were represented exclusively by the tissues of the tooth root. When the tooth root is in contact with the mandibular canal, removal often leads to compression of the neurovascular bundle. The patient experiences postoperative paresthesia of the teeth and lower lip, which lasts on average from one to six months. It is important to note that paresthesia in these cases requires treatment, the prescription of neurotropic drugs and physical therapy. If, after the removal of the third molar, the doctor observes in the tooth socket an open area of the neurovascular bundle not covered by bone, it is important not to curettage the bottom of the socket, not to use antiseptics, or to tightly tamponade the socket. The main symptom of nerve compression during extraction is pain when the instrument impacts the tooth root. It is important to distinguish between pain from incomplete anesthesia and pain from nerve compression. If, when dividing a tooth with a drill into a crown and roots (contact with the pulp), the patient did not experience pain, but when removing the roots, he feels acute pain - most likely there was compression of the wall of the mandibular canal and compression of the neurovascular bundle. Most often, such cases occur when the nerve passes on the side of the root of the third molar (usually with one root). In this position, tooth dislocation in the bucco-lingual direction leads to compression. If loosening of a tooth in one direction is painful for the patient, the tooth socket should be expanded on the opposite side and traction should be applied in the direction opposite to the area of compression.
Rice. 1. Contact location of the mandibular canal and the root of an impacted tooth (CBCT). The tooth has a recess through which the neurovascular bundle passes. When removing such a tooth, there is a high risk of nerve compression.
Rice. 2. Anatomical notch in the root through which the neurovascular bundle passes.
Postoperative period
Based on the patient’s condition, the doctor can prescribe antibacterial therapy 9 both locally and orally). To relieve toothache and generally normalize your health, painkillers may be prescribed. It is also possible to take medications that reduce fever.
After the operation, the doctor may additionally prescribe physiotherapeutic procedures using ultrasound. After them, swelling and inflammation decrease, which leads to the disappearance of painful sensations.
After the operation, it is necessary to exclude any thermal exposure: do not drink hot water and drinks, do not take a bath or other procedures that promote vasodilation.
The gauze pad that the specialist places on the wound must be removed after 20 minutes.
Eating is prohibited for several hours after tooth extraction.
You cannot rinse the socket intensively so as not to wash out the blood clot, as it promotes tissue fusion.
You should not use your tongue, brush, dental floss, toothpick, etc., into the hole formed after tooth extraction.
In case of severe swelling and pain, ice is applied to the side where the tooth was removed.
Prevention of complications after tooth extraction
- Responsible choice of clinic and doctor is one of the most important conditions for successful treatment.
- X-ray monitoring of all performed manipulations allows timely detection and prevention of complications.
- Compliance with all dentist recommendations for oral care after surgery.
- Timely installation of an implant helps to avoid changes in bite.
- A thorough medical history allows you to choose the right anesthesia and calculate its dosage.
- Reducing treatment time, a comfortable environment and a friendly attitude allow you to avoid most common complications.
- Compliance with the rules of asepsis and antisepsis prevents and stops the development of inflammatory and purulent pathologies.
Tooth extraction is a surgical operation; this procedure must be handled responsibly. An informed and careful choice of clinic and doctor will help avoid most complications. Competent patient management and a friendly atmosphere will leave only positive emotions about treatment at the dentist, contrary to prevailing stereotypes.
Sources used in writing the article:
- “Outpatient surgical dentistry”, Bezrukov V.M.
- "Surgical dentistry", T.G. Robustova.
- “Guide to maxillofacial surgery and surgical dentistry”, A.A. Timofeev.
Please rate this article
Stanislav Mezheritsky
Chief physician, surgeon, orthopedist
The author of the article is Stanislav Mezheritsky, a practicing dentist with 19 years of experience, chief physician and one of the founders of the Matisse Dent clinic. The main focus is orthopedic and surgical dentistry. Author of numerous publications, regular participant in specialized seminars.