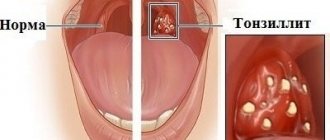
Increased body temperature, painful sensations in the throat, weakness, headache - people usually attribute these symptoms in the spring-winter period to a common cold. However, often such signs indicate the development of a dangerous infectious disease, which doctors call purulent tonsillitis. The disease is manifested by severe inflammation of the tonsils (glands), located in the nasopharynx. The infection primarily affects the parenchyma and lymphoid tissue lining the tonsils. The disease is dangerous due to severe complications that develop when symptoms are ignored and there is no proper treatment.
If you suspect that you have a sore throat and need to consult a doctor, call +7 (499) 653-58-25 - we will definitely help you. Reception is carried out both in the clinic and with a visit to the patient’s home. To register online, fill out the form on the website.
Causes
Inflammation of the palatine tonsils is provoked by infections transmitted by airborne droplets. Less commonly, infection occurs through contact and household contact (through shared dishes, towels, bed linen). The most common causative agent of purulent sore throat is hemolytic streptococcus. However, if a person’s immune system works normally, bacteria of this group die immediately after entering the body. The development of pathology is facilitated by weakened immunity and provoking factors.
Indirect causes of purulent sore throat include:
- severe hypothermia;
- chronic diseases of the upper respiratory tract;
- oral infections;
- alcoholism and smoking history;
- stress, overwork, strong emotional tension;
- living in areas with difficult environmental conditions;
- deficiency of vitamins and nutrients;
- mechanical damage to the tonsils (trauma, surgery).
The disease is diagnosed with equal frequency in adults and children.
Prerequisites for the development of tonsillitis
The palatine tonsils, nasopharyngeal tonsil, lingual and tubal tonsils form a protective ring (lymphoepithelial ring of Pirogov) - a powerful barrier to the air and food entering the body. The tonsils do a great job - they recognize dangerous viruses and bacteria in the air and food and trigger an immune reaction.
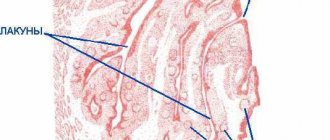
When examining the tonsil on its surface, you can see depressions and openings with narrow, winding and deep passages (the so-called tonsil lacunae).
| 1 - crypt (lacuna); 2 - lymphoid follicles; 3 - connective tissue capsule; 4 - mouth of the lacuna (crypt). | |
The existence of deep lacunae creates the prerequisites for the development of chronic inflammation of the tonsils. Remains of food, dead immune cells, etc. settle in the gaps, which are an excellent breeding ground for the proliferation of pathogenic microorganisms.
Incubation period
The period from the moment the pathogen enters the body until the appearance of the first characteristic symptoms can range from 2 to 6 days. During the first few days, the sick person is still unaware of his condition, becoming a source of infection for others. During the incubation period, the infection is actively transmitted by airborne droplets (through coughing, sneezing, kissing, talking). The onset of the disease is manifested by a feeling of chills, increased body temperature, weakness and headache. The sooner the patient sees a doctor, the easier the treatment is.
Features of the chronic form of the disease
Chronic inflammation of the tonsils can have several clinical variants:
- Latent form, when the patient does not experience significant discomfort in the throat and does not experience signs of exacerbation of the disease. Such people consider themselves healthy and are not aware of the dormant infectious-inflammatory focus in their throat.
- Periodically relapsing type of disease. Sluggish exacerbations and episodes of clearly defined inflammation of the tonsil itself, adjacent palatine arches and the pharyngeal wall are possible. Between periods of exacerbation, the inflammatory process subsides, but is not completely eliminated.
In chronic tonsillitis, the drainage and natural self-cleaning of crypts (folds) and lacunae (recesses) are disrupted in the tonsils; pus, living and dead bacteria, and toxins are constantly stored in their depths. This maintains constant inflammation, overstimulates sentinel immune cells, and provokes toxic-allergic reactions.
The immune response that forms during chronic tonsillitis is not sufficient to completely suppress the infectious process; it only restrains the activity of pathogens. Disruption of this delicate balance leads to exacerbation of the disease or triggers immune disorders.
Symptoms of purulent sore throat
In most patients, the first signs of purulent tonsillitis appear 2-3 days after the pathogen enters the body. When the patient's immunity is weakened, the clinical picture is most pronounced. In adult patients, the following symptoms are observed:
- the appearance of noticeable white or yellowish spots of pus on the tonsils;
- high body temperature (in the range of 39-40 ° C);
- intense pain in the throat that increases during swallowing;
- significant enlargement of the lymph nodes located under the lower jaw;
- easily removable whitish coating on the tongue;
- severe headaches;
- feeling weak and overwhelmed;
- loss of appetite;
- aching joints.
In adults, with timely treatment, the acute stage of the disease rarely lasts longer than a week. If the patient does not seek help from specialists, there is a risk of complications.
Why is tonsillitis dangerous?
Chronic tonsillitis is very dangerous: if you do not consult a specialist in a timely manner and self-medicate, complications may develop, among which the most dangerous are diseases of the heart and blood vessels, and rheumatic joint damage.
Tonsillitis in adults often leads to damage to the kidneys ( tonsillorenal syndrome ) and heart ( tonsillocardiac syndrome ). This is due to the fact that infectious and toxic factors that damage internal organs enter the body from the palatine tonsils. Streptococcus, for example, secretes a toxin, the effects of which can cause myocardial dystrophy and heart disease or rheumatism . In addition, purulent contents entering the gastrointestinal tract from the lacunae of the tonsils can provoke dysbacteriosis.
Stages of disease development
The disease progresses rapidly. This is especially true in children and adults with a weakened immune response. Symptoms depend on the current state of the body, age, concomitant diseases and the stage of infectious tissue damage.
Signs of the development of the disease at different stages from the moment of infection:
- 2-3 days.
This stage is characterized by the maximum severity of the symptomatic picture. The patient's tonsils increase significantly in size and white or yellowish ulcers appear on their surface. The inflammatory process covers the entire surface of the tonsils. The patient notes deterioration in health, weakness, loss of appetite and signs of fever, including an increase in body temperature to 39-40 ° C. The patient also experiences excruciating pain in the throat, which gets worse when swallowing. - Day 4
The ulcers that form on the tonsils begin to spontaneously open, releasing the contents (pus). In their place, lacunae are formed - characteristic depressions. If at this stage the patient follows the doctor’s recommendations, the lacunae quickly close. - 5-6 day
. At this stage, patients feel a noticeable improvement in their condition - body temperature normalizes, headaches go away, strength and appetite are restored. - 7-10 day
. The last pathological sign – sore throat – recedes. The size of the lymph nodes located under the lower jaw also decreases. The patient ceases to feel pain and discomfort in this area.
Competent and timely therapy allows you to avoid serious complications.
Classification of tonsillitis
The disease can be acute or chronic. In the first case, signs of infection disappear within 7 to 10 days. In a chronic course, pathogens remain in the tissues of the tonsils, causing periodic exacerbations. Treatment of chronic tonsillitis is a complex task that only experienced otolaryngologists can handle.
Chronic tonsillitis has 2 forms - simple and toxic-allergic. In the latter case, there are 2 degrees of severity of pathological changes.
The simple form is characterized by only local symptoms. With the toxic-allergic variant, the following pathological processes occur:
- microbial toxins that enter the blood cause sensitization (altered reactivity) of the body;
- they act directly on the tissues of internal organs;
- toxins also lead to the development of allergic and autoimmune reactions.
To treat tonsillitis in this case, a complex effect on the entire body is necessary.
Forms of the disease
The form of purulent tonsillitis depends on many associated factors and conditions. The most common three forms of development are follicular, lacunar and ulcerative-membranous (necrotic). Each type is characterized by characteristics of the course, specific lesions of the tonsil tissue and varying duration.
Follicular
Follicular tonsillitis is manifested by pinpoint purulent lesions of the parenchyma of lymphoid tissue and follicles of the tonsils. The disease in 85% of cases is caused by group A streptococci. The remaining cases of infection are associated with staphylococcal infection, Haemophilus influenzae, pneumococcus, and adenovirus. This form of pathology is accompanied by a rapid increase in the symptom complex, severe hyperthermia, sweating, loss of sleep and appetite. Intense pain in the throat can radiate to the ear.
Lacunarnaya
This type of disease causes severe inflammatory damage to the tissues of the peripharyngeal ring. The opening of abscesses is accompanied by the formation of specific perforations on the surface of the tonsils - lacunae. The acute phase of the disease is manifested by an increase in the size of the tonsils, up to difficulty breathing. Along with other symptoms, a characteristic sign of the lacunar type of pathology is bad breath. Sometimes doctors note a noticeable change in voice and diction problems. Inadequate therapy can lead to the development of a paratonsillar or retropharyngeal abscess.
Necrotic
Necrotizing ulcerative tonsillitis is rare (about 5-6% of cases). The main cause of the development of this type of disease is fusospirochetous infection. The rapid development of the infectious-inflammatory process causes the formation of histological changes in the tissues of the palatine tonsils. Violations of vascular permeability, associated with the active production of histamine and cytokines, lead to hypertrophy and sometimes tissue necrosis. The first sign of the disease is the feeling of a “lump in the throat.” Later, a sharp, unpleasant putrid odor appears from the mouth and salivation increases.
Therapeutic tactics for tonsillitis
If we consider that chronic tonsillitis is only a long-term inflammatory process in the tonsils, then it is unlikely that this disease should have received so much attention from other medical specialties. Therefore, the very definition of tonsil disease as chronic tonsillitis requires clarification. This will make the motivation for different types of conservative or surgical treatment clearer. So, chronic tonsillitis is a process of constant interaction between lymphoid tissue and the contents of the lacunae of the palatine tonsils (purulent detritus with elements of foreign protein, toxins as a result of the vital activity of pathogenic flora, microorganisms themselves, dead epithelial cells from the walls of the lacunae of the palatine tonsils, nutritional particles). The discharge in the lacunae can be purulent, caseous, accumulate in narrow lacunae convoluted with spurs, and form so-called fetid plugs. This process, which takes place in the lacunae of the palatine tonsils, is under the control of the body until a certain time, i.e. There is constant active and passive drainage of tonsil lacunae along with the activity of macrophages, which, preventing inflammation of the palatine tonsil, contributes to the development of immunity to many microorganisms that enter the oral cavity and pharynx along with air and food.
This kind of balance between the vital activity of pathogenic active flora and the protective capabilities of the body can be disturbed for many reasons, as a result of which inflammation of varying intensity develops (it captures only the covering epithelium of the oral surface of the tonsils without its destruction), which passes to the epithelial cover of the lacunae of the tonsils with its destruction and formation necrotic plaques; suppuration of the tonsil follicles. Catarrhal, lacunar or follicular tonsillitis develops
.
In foreign literature, they tend to combine two diseases of the oropharynx and designate inflammation of the tonsils and pharyngeal mucosa as “tonsillopharyngitis.” However, experts in Russia quite reasonably believe that such a combination of two nosological units is possible only in cases of a combination of acute catarrhal pharyngitis and catarrhal tonsillitis. Lacunar and follicular tonsillitis have their own clearly defined clinical, morphological and microbiological aspects
, and they cannot be confused with manifestations of pharyngitis, especially from the point of view of the approach to treatment.
According to modern concepts, angina is an acute infectious-allergic disease, and it is necessary to approach the treatment of a patient with angina from this point of view.
As was said, the presence and persistent preservation of purulent detritus in the lacunae of the palatine tonsils is a determining factor both in making the diagnosis of “chronic tonsillitis” and in choosing the appropriate method of treatment - conservative or surgical.
A sore throat with destruction of the integumentary epithelium of the lacunae promotes the formation of scars in their lumen, which subsequently complicates the drainage of the lacunae of the tonsils. A kind of vicious circle arises - sore throat develops under the influence of pathogenic flora against the background of sensitization by a foreign protein due to a violation of the epithelial cover of the lacunae. Moreover, a sore throat can occur both under the influence of a pathogenic infection and as a result of nonspecific irritation (general hypothermia, drinking cold water).
Each previous angina, especially lacunar, follicular, can contribute to the development of conditions for relapse of inflammation, accompanied by otitis, sinusitis, and bronchitis.
The main reason for this is the viruses that cause most respiratory tract infections, which can weaken the body's defenses. Viruses reduce the ability of macrophages and granulocytes to absorb infectious agents. In this way, the epithelium of the mucous membrane is damaged, which impedes the activity of the epithelial villi and leads to stagnation of mucus. Weakening of local protective mechanisms in many cases leads to infection of the upper and lower respiratory tract with bacteria Haemophilus influenzae, Streptococcus pneumoniae and Staphilococcus aureus, which are usually found in the oral cavity and trachea.
The chronic nature of infections is an indicator that the body's immune system is unable to cope with its functions. Constant but insufficient activation of nonspecific defense mechanisms often causes an inflammatory response, but this is not enough to suppress infectious agents.
Undoubtedly, the nature of the pathogenic flora plays a big role in the occurrence of a particular sore throat,
but the background against which it occurs also influences the clinical picture of the disease. Therefore, therapy should be prescribed and carried out taking into account all identified features in each case (time from the onset of angina, age of the patient, frequency of exacerbations, concomitant diseases: general and from the ENT organs, clinical manifestations, including in the oropharynx, nature of the flora , previous treatment, its effectiveness).
Currently, much attention is paid to the role of group A streptococcus in the occurrence of acute tonsillitis and pharyngitis, although b-hemolytic streptococcus still occupies a leading position among bacterial pathogens. Thus, it is believed that in late autumn and spring it is group A streptococci that cause disease in 40% of children and 10% of adults. Along with this, there is an opinion that in the vast majority of cases, the incidence of the lymphadenoid ring of the pharynx in children is determined by a viral infection, the features of which are a protracted and recurrent course, insufficient effectiveness of conservative anti-inflammatory measures, and a tendency to hyperplasia of the palatine and pharyngeal tonsils. Usually, the doctor diagnoses a sore throat “by eye,” only on the basis of clinical experience, and prescribes antibacterial treatment without taking into account the advisability of antiviral therapy. This not only slows down the healing process, but can also contribute to a decrease in the protective properties of the pharyngeal mucosa, since under the influence of antibiotics a-hemolytic streptococcus, which produces bactericin, a natural antibiotic, disappears. It is penicillins
to a greater extent than cephalosporins, they suppress this beneficial flora of the oropharynx and allow pathogenic streptococci to take its place on the epithelium of both the tonsils and the entire pharynx. Therefore, irrational (too early and without taking into account the flora) prescription of antibiotics leads to a decrease in antibacterial immunity and contributes to relapses of sore throat.
Based on the foregoing, the treatment tactics for patients with acute and chronic tonsillitis should consist of an accurate determination of the nature of the inflammatory process (acute, exacerbation of chronic or its sluggish course), justification of the type of inflammation (catarrhal, purulent, phlegmonous), determination of the type of pathogen (streptococcus, spirochete, bacillus , virus, mushrooms). To this it is necessary to add that all sore throats can be divided into two groups
- primary tonsillitis, as a self-developing acute inflammatory process in the tonsils, and secondary tonsillitis, as a symptom of the underlying disease, for example, in blood diseases. Only the correct diagnosis, taking into account the general condition of the patient, determines the choice of treatment tactics.
Acute sore throat
Catarrhal tonsillitis is the mildest form of tonsillitis, which affects the mucous membrane of the tonsils, sometimes in combination with inflammation of the mucous membrane of the oropharynx (mainly the area of its posterior wall), which gives a mixed picture of tonsillitis and pharyngitis. The main complaint is pain when swallowing food and saliva (with pharyngitis, swallowing saliva is more painful - “empty swallow”). The general condition is satisfactory, the disease lasts 6-7 days, body temperature is within the subfebrile range. Treatment involves the widespread use of physiotherapeutic procedures, frequent rinsing with warm disinfectant solutions, a gentle diet, plenty of warm drinks, and the use of salicylates. Prescribing antibiotics for identified catarrhal tonsillitis is considered inappropriate, especially without a clear idea of the causative agent
.
Due to the fact that even without the use of antibiotics all the symptoms of the disease disappear quite quickly (on the 2-3rd day), early prescription of antibiotics in cases of catarrhal tonsillitis leads to the fact that patients stop taking them without observing the course dose. In addition, complete suppression, for example, by phenoxymethylpenicillin, amoxicillin (the most commonly used antibiotics), group A streptococci (and with them a-hemolytic streptococcus, which resists pathogenic flora) leads to the fact that the person returning to the normal environment (home, school and etc.) the recovered patient again encounters this flora, but already capable of transmission, i.e. the possibility of relapse of inflammation of the tonsils increases - natural immunity is suppressed. When prescribing antibiotics in the first days of a sore throat, it is also necessary to remember about the possible resistance of a number of strains of streptococci to the prescribed antibiotics, for example, to macrolides such as erythromycin, clarithromycin. Therefore, the most rational prescription of antibiotics in the treatment of mild forms of sore throat is after laboratory confirmation of the sensitivity of the flora to them
. These provisions are classics, but in practice, for many reasons, they are not always observed, which will ultimately lead humanity to complete disarmament in the face of transforming strains of pathogens, including those that cause sore throat.
Severe forms of angina - lacunar, follicular
- require the prescription of antibiotics, but also in compliance with the rules for combating infection and taking into account all factors: diagnosis, flora, somatic status, the need to prevent complications, the full course of taking an antibiotic.
Chronic tonsillitis
What are the treatment tactics for recurrent tonsillitis, recurring 2 times a year or more often?
In these cases, the disease is defined as “chronic tonsillitis,” however, for it, the frequency of relapses of tonsillitis may not always be the determining factor, since the concept of “chronic tonsillitis” also includes other parameters that support the diagnosis. These are, first of all, complications clearly associated with it from other organs and systems of the body.
For a practicing physician, both a general practitioner and an otorhinolaryngologist, after making a diagnosis of “chronic tonsillitis,” it is important to choose the tactics of treating the patient and decide the question: in which cases is surgery indicated, and in which - conservative therapy.
We divide chronic tonsillitis into only two forms: chronic tonsillitis I and chronic tonsillitis II
. In the first case, conservative treatment is required, in the second - surgical treatment. The determining factor is the combination of local signs of tonsillitis with complications and features of the course.
Conservative treatment
Conservative treatment involves, first of all, systematic sanitation of the lacunae of the palatine tonsils while preserving the lymphoid tissue of the tonsils.
as an immune, to a certain extent, organ. Conservative treatment is indicated for uncomplicated chronic tonsillitis in cases where surgery can be delayed due to the general condition of the patient; if the patient has not previously received any therapy or is mainly concerned about local manifestations of tonsillitis - purulent plugs in the tonsils, bad breath, etc.
Among the methods of conservative treatment for chronic tonsillitis, the most effective are the following: washing the lacunae of the tonsils and removing purulent plugs and detritus (carrying out repeated courses using the “Tonsilor” apparatus, when simultaneously washing the lacunae of the tonsils with a disinfectant solution, suctioning out the pathological contents from them and ultrasonic exposure with low-frequency ultrasound on the tonsil tissue), as well as the introduction of various medications into the tonsil using phonophoresis. Physiotherapeutic treatment – KUF, “Yakhont-F”.
Both for sore throat and for accompanying pharyngitis, gargling, inhalation, and irrigation of the mucous membrane with disinfectant solutions are indicated.
Increasing the effectiveness of treatment can be achieved by prescribing immunostimulating plant extracts. Tonsilgon N
is a combination preparation of plant origin. The chamomile, marshmallow and horsetail components included in its composition stimulate the body's defense mechanisms by increasing the phagocytic activity of macrophages and granulocytes. The drug has anti-inflammatory, immunostimulating, anti-edematous and antiviral effects, accelerates the healing process and shortens the duration of the disease; can be used in the future to prevent relapse of the disease. There were no side effects when using the drug.
Tonsilgon N is available in two forms: in the form of drops for oral administration and in the form of tablets. For adults, the drug is prescribed 25 drops or 2 tablets 5-6 times a day, for children under 5 years old - 5-10 drops, for children 5-10 years old - 15 drops, for teenagers 10-16 years old - 20 drops 5-6 times a day. day. After the disappearance of acute manifestations of the disease, the frequency of taking Tonsilgon N is reduced to 3 times a day. The duration of basic therapy is 4-6 weeks.
The prescription of systemic antibiotic therapy for uncomplicated forms of tonsillitis of non-streptococcal etiology is not always justified. In this case, local prescription of antimicrobial drugs is more rational (from the first day of the disease until the results of a microbiological study are obtained). The main requirements for local antibacterial agents are a wide spectrum of antimicrobial action, including the most typical pathogens, lack of absorption from the mucous membrane, and low allergenicity.
Fusafyungin (Bioparox) has the most optimal combination of the above requirements.
- inhaled antibiotic with anti-inflammatory properties. The wide spectrum of antibacterial action of fusafyungin, the absence of resistant strains of microorganisms, and the drug’s own anti-inflammatory properties make it especially effective in the treatment of tonsillitis of non-streptococcal etiology. The most optimal is to use 4 doses of the drug every 4 hours for 10 days.
Other drugs used in the treatment of sore throats and exacerbations of chronic tonsillitis are:
Clarithromycin
- 1 tablet 2 times a day.
Coldrex
- 2 tablets 2 times a day. Children 6-12 years old - 1 tablet 4 times a day.
Tonsillotren
(lozenges) - 1 tablet every hour.
Treatment of tonsillitis such as agranulocytic and monocytic requires the participation of a hematologist.
Surgery
Indications for surgical intervention:
1. Frequent (2-4 times a year) sore throats, accompanied by high body temperature; pathological purulent detritus is noted in the lacunae; there is one or another complication associated with an exacerbation of the process (polyarthritis, pyelonephritis, etc.).
2. Frequent sore throats (2-4 times a year or more often), accompanied by high body temperature, local signs of chronic tonsillitis are observed, without identified complications. Frequently recurring sore throats indicate a weakened immune system.
3. As a result of one of the rare cases of tonsillitis (once every 5-7 years), some complication of the heart, joints, etc. developed. Local signs of chronic tonsillitis, adenitis of the lymph nodes in the area of the angle of the lower jaw.
4. There were no cases of tonsillitis, however, against the background of emerging diseases of the heart, joints, etc., local signs of chronic tonsillitis are revealed, mainly the accumulation of purulent contents in the lacunae of the tonsils.
Fuzafyungin –
Bioparox (trade name)
(Servier)
Combined preparation of herbal origin –
Tonsilgon N (trade name)
(BIONORICA Arzneimittel GmbH)
| Applications to the article |
| Chronic tonsillitis is a process of constant interaction between lymphoid tissue and the contents of the lacunae of the palatine tonsils. |
| After making a diagnosis of chronic tonsillitis, it is important to choose a treatment strategy for the patient and decide the question: in which cases is surgery indicated, and in which - conservative therapy. |
Diagnosis and treatment
To make a diagnosis and determine treatment approaches, you need to consult an otolaryngologist. Diagnostics is carried out according to the following algorithm:
- collection of medical history and complaints;
- examination of the pharynx using special lighting (pharyngoscopy);
- general and biochemical blood test;
- bacteriological examination of a smear with the preparation of an antibiogram.
How to treat a purulent sore throat is determined by an ENT specialist. In severe cases, hospitalization is required. General medical recommendations include bed rest, drinking plenty of fluids, taking vitamins and restorative medications.
Specific treatment of the disease is a complex of procedures and medications:
- Drug treatment of the oral cavity.
Complex therapy necessarily includes gargling with antiseptic solutions. For this purpose, solutions of furatsilin, manganese, hydrogen peroxide, sea salt, and natural herbal decoctions (chamomile, calendula) are used. This procedure is aimed at removing pathogenic microorganisms from the throat and mouth. - Taking systemic antibacterial drugs.
A full course of antibiotic therapy allows you to get rid of pathogenic flora. Antibiotics and their dosages can only be determined and prescribed by a doctor. The most commonly used drugs are from the groups of penicillins, macrolides and cephalosporins. - Symptomatic therapy.
To alleviate the patient’s condition during the acute stage, the specialist prescribes symptomatic treatment in the form of antipyretics, antihistamines and anti-inflammatory drugs. Sometimes it is recommended to undergo physiotherapeutic procedures during the recovery period.
Correctly selected treatment helps to avoid serious consequences and ensures healing of the affected tissue areas without visible defects.
Purulent sore throat in children
If the disease develops in a child, in addition to the main symptoms, digestive disorders often appear - diarrhea, nausea, vomiting. Children may complain of abdominal pain caused by intestinal spasms. The follicular type of pathology is especially difficult for children aged 5-10 years, causing inflammation of the meninges. Young patients often experience fainting, dry cough and complaints of a feeling of a foreign object in the throat.
If parents ignore the symptoms, the pathology becomes chronic. Pediatricians call this condition chronic tonsillitis, exacerbations of which occur 2-3 times a year.
Causes, main risk factors
Up to 30 different colonies of pathogenic microbes can be sown on the surface of the tonsils of patients suffering from chronic tonsillitis. But in crypts and lacunae staphylo- or streptococcus is usually determined. A key role in the pathogenesis of chronic tonsillitis is played by beta-hemolytic strains of streptococcus (type A). Other flora - gram-negative coccal, fungal, viral - have an impact on local immunity, they support inflammation.
There are a number of factors contributing to the occurrence of the disease:
- hypothermia;
- decreased immunity;
- microtrauma of the tonsils;
- foci of inflammation in the mouth and in the head area (caries, sinusitis, adenoids, etc.);
- smoking;
- poor nutrition;
- allergy.
Viruses and bacteria that cause tonsillitis can come from the external environment.
Complications and consequences
The advanced form of the disease leads to inflammatory damage to other organs, including the heart, kidneys, and joints. The most dangerous complications include:
- mediastinitis
– inflammation of the mediastinal tissue; - chronic bronchitis
- inflammatory damage to the bronchi; - sepsis –
spread of infection through the bloodstream; - arthritis -
inflammation of the joints; - glomerulonephritis is
a dangerous kidney disease; - purulent meningitis -
damage to the meninges; - peripharyngeal abscesses
- suppuration of the lymph nodes and tissue of the peripharyngeal space.
Timely access to a medical facility allows you to avoid negative health consequences.
Complications of chronic tonsillitis
Against the background of a chronic inflammatory process in the tonsil area, various complications are possible. Therefore, it is important to know why chronic tonsillitis is dangerous. Thus, the tonsils themselves, losing their function as a barrier to infection, become its breeding ground. Inside them are pathogens with the products of their metabolism. The infection can spread throughout organs and tissues, affecting the renal parenchyma, joint and heart tissue, and liver. In addition, tonsillitis adversely affects the functioning of the immune system and can be a provocateur of collagen diseases - lupus, scleroderma, dermatomyositis, periarteritis. The skin and peripheral nerve fibers may also be affected. With prolonged intoxication against the background of the disease, damage to blood vessels (vasculitis) and platelets (purpura) is possible.
Prevention
By paying attention to preventive measures, you can reduce the risk of developing the disease. Effective prevention includes:
- avoiding hypothermia (wearing warm clothes, monitoring microclimatic indicators in the room);
- regular preventative visits to the dentist to identify the early stages of caries and stomatitis;
- giving up bad habits (smoking, drinking alcohol);
- moderate physical activity, regular walks in the fresh air;
- normalization of diet, sleep and wakefulness;
- compliance with hygiene standards and requirements, maintaining cleanliness in the home and workplace;
- limiting contacts with unfamiliar people during periods of unfavorable epidemiological conditions.
Strengthening the immune system based on leading a healthy lifestyle helps to avoid infection and make it easier to endure purulent sore throat.
If you have a sore throat, call us and we will definitely help you!