Indications for the use of antibiotics in dentistry
The need for treatment with antibiotics depends on the nature of the infection and the body's ability to withstand the course. The main reasons for prescribing antibiotics include:
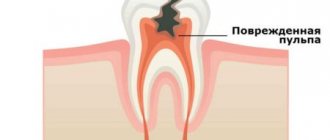
- When advanced caries threatens pulpitis, the dentist may prescribe antibiotics to limit the spread of the pathological process. The patient is prescribed antihistamines to complement the effectiveness of antibiotics.
- With the development of an inflammatory process of periodontal tissue (periodontitis), antibiotic therapy allows the destruction of protozoa, gram-negative anaerobes in the oral cavity. Various dosage forms of drugs are used for treatment: gels, ointments, intramuscular and intravenous injections, tablets.
- The proliferation of pathogens, poor immunity, caries and dense plaque can lead to the development of gingivitis. After laboratory detection of the sensitivity of microbes to the antibiotic, a course of treatment is prescribed. Antibiotic drugs are mainly used for catarrhal gingivitis.
- The appearance of purulent accumulations inside the oral mucosa provokes the appearance of a fistula. The process occurs due to the proliferation of anaerobic gram-negative bacteria, streptococci, staphylococci, Pseudomonas aeruginosa or Escherichia coli. A doctor-prescribed course of antibiotics, which are also used for dental implantation, will help cope with the infection.
- Inflammation of the connective tissue around the root of the tooth is called periodontitis. The occurrence of the disease is a consequence of dental trauma, a complication of pulpitis, caries, or an error in dental treatment. If the process is not stopped, pus may appear. The effectiveness of antibiotics for periodontal disease is felt after preliminary cleaning of the periodontal tissue.
- The result of inflammation of various origins can be a granuloma - a cavity of granulation tissue filled with fluid. Location: on the gum near the root of the tooth. It is important to start treating granuloma in the early stages. The use of antibiotics facilitates the opening of the granulosa vesicle and suppresses the infection accumulated in it, and serves to prevent infection. Self-medication with antibacterial drugs is unacceptable.
How is pulpitis treated surgically?
As we have already noted, there are two possible options for surgical intervention:
- treatment of pulpitis using the amputation method with partial preservation of the pulp;
- treatment with complete removal of soft tissues, blood vessels, and nerves.
If there is an objective possibility, the doctor will remove only the top of the pulp - from the crown, leaving the root part. The blood supply and sensitivity (innervation) of the tooth will be preserved. The technique is used in the treatment of children - for milk or permanent teeth that have not yet fully grown. This allows them to form normally in the future. Treatment for pulpitis can be carried out in one visit.
Types of antibiotics for toothache
Doctors use antibiotics in dentistry, which have a wide range of applications, to stop the growth and reproduction of mixed bacterial infections in the oral cavity. Drugs are divided into the following types:
Should I take an antibiotic for dental inflammation?
What to do if the gums become inflamed after the removal of a wisdom tooth, due to trauma, or with advanced caries? How to treat a complicated form of periostitis and periodontitis? The effectiveness of therapy largely depends on the selection of the optimal type of antibacterial drug to suppress the pathological process. It is useful to know when an antibiotic is prescribed for dental inflammation, which groups of drugs are most often used in dental practice.
How to use an antibiotic for tooth inflammation with pus
At the first stage, while the pathological process is less active, rinses with an antibacterial effect are carried out as prescribed by the dentist.
Local medications act directly on the affected area and are less absorbed into the systemic circulation, which reduces the risk of side effects.
You need to crush the tablets of Lincomycin, Azithromycin or Tetracycline, combine them with lukewarm (not hot) boiled water, and rinse your mouth with the solution. The proportions of the components are selected by the dentist.
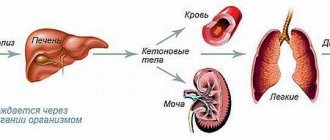
Active inflammatory process in the periosteum and gums after removal of the problem unit, with infection from the outside or hematogenously, flux is an indication for the prescription of antimicrobial compounds. It is important to prevent complications that develop when purulent masses accumulate or exudate exits into the oral cavity through the fistula. With the flow of blood and lymph, infectious agents penetrate into other parts of the body.
Periodontitis and periostitis in acute or chronic form are dangerous diseases. To heal the wound, the dental surgeon first cleans the affected area, removes a thick mass containing pathogens, particles of blood and mucus. The second stage is the prescription of antibacterial drugs. For purulent inflammation, penicillins show high effectiveness: Amoxicillin, Amoxiclav. Depending on the severity of the pathological process, antibiotics are taken orally or given injections.
If an odontogenic infection is detected, against which the gums fester, the use of the drugs Gentamicin, Grammidin C, Ciprofloxacin, Cifran is indicated.
Complications of alveolitis
If alveolitis is not treated in a timely manner, the following complications may develop:
- Odontogenic sinusitis is an inflammation of the maxillary sinus caused by the spread of infection from the inflamed sockets after the removal of premolars or molars of the upper jaw;
- Phlegmon - purulent inflammation spreads to the surrounding soft tissues;
- Acute periostitis - pus accumulates in the periosteum area;
- Odontogenic osteomyelitis is a purulent-necrotic lesion of the jaw bone;
- Sepsis - an infection enters the bloodstream, causing it to become infected.
Alveolitis itself is not so dangerous, but its complications are life-threatening. Therefore, if you notice symptoms of alveolitis, contact your doctor immediately.
Names of antibiotics used for inflammation of the dental nerve and root
The dentist prescribes medications to suppress infection based on the results of an examination of the problem area. When the nerve is inflamed, it is difficult to eat and drink; throbbing or aching pain accompanies a person throughout the day and intensifies at night.
Before starting therapy, the doctor conducts an allergy test and interviews the patient to identify contraindications.
Antibiotics help eliminate inflammation of the root and dental nerve:
- Ciprofloxacin.
- Azithromycin.
- Amoxiclav.
- Azithromycin.
- Ampiox.
- Doxycycline.
- Digital
Is it painful to treat pulpitis?
Many patients believe that treatment for pulpitis is painful. In fact, pain accompanies the disease itself, and not the procedure for its treatment. The pulp tissue and nerves become inflamed, which causes unbearable painful sensations comparable to an electric shock. Pulp removal is absolutely comfortable, because high-quality anesthetics completely relieve the patient of pain while the doctor prepares the canals. During treatment or after treatment of pulpitis, the tooth hurts when the internal tissues are severely inflamed. Then safe painkillers are prescribed while healing occurs (1 - 3 days).
List of effective antibacterial agents for dental infections under the crown
After endoprosthetics and implant installation, some patients complain of discomfort. Pain and inflammation are a consequence of a violation of the technology for fixing artificial teeth and crowns: the dentist did not completely fill the cavity inside the problem unit or mechanical damage to the canal walls occurred. If the implantologist is poorly qualified, the pin may be installed incorrectly. Perhaps the smallest parts from dental instruments remain inside the canal.
There are several causes of the pathological process and pain syndrome:
- swollen gums or gumboil (acute inflammation);
- cyst - a cavity with fluid near the root of a problematic unit of the dentition;
- inflammation of the submandibular salivary glands;
- dental granuloma;
- a fistula on the gum is a hole through which purulent masses are released.
With the development of inflammation in periodontal tissues, an abscess forms at the root apex. Painful sensations are a consequence of the active accumulation of exudate and pressure on neighboring areas.
The main condition for eliminating discomfort is a timely visit to the dentist to remove the crown, clean the root canals, and eliminate the cause of the inflammatory process. Uncontrolled use of antibiotics can harm the body.
Before treating the canals, the doctor makes an injection into the gum, removes the prosthesis, and examines the affected area.
Effective antibiotics are prescribed to suppress the infection:
After the removal of a wisdom tooth, there is an increased risk of not only inflammation, but also bleeding from the socket.
If the patient takes the drug Warfarin to prevent thrombosis, then you need to warn the dentist: the doctor temporarily stops taking the medication for several days before and after the extraction of the “eight”, be sure to coordinate this action with the cardiologist.
It is important to know how to combine an antithrombotic agent with antimicrobial compounds.
What is a dental cyst?
Tooth cyst - what is it? An odontogenic cyst is a pathological neoplasm that occurs in the upper part of the tooth root. The internal cavity of the cyst is filled with liquid or mushy purulent contents; it is enveloped by a dense layer of epithelium.
The size of the cyst starts from a few millimeters, with rapid development reaching several centimeters in circumference. Most often, the pathological process affects the upper jaw, since the roots of its teeth have a more porous structure.
In order to understand what a dental cyst is and how to treat it, you need to know why such a phenomenon occurs. The formation of cysts occurs as a result of inflammation, thus the body restricts healthy tissue from the affected areas, clogging them along with bacteria into bubbles.
The use of antibiotic therapy during pregnancy and lactation
Most antimicrobial agents are prohibited for use by expectant mothers and during breastfeeding. When prescribing antibiotics to suppress the purulent-inflammatory process in the gums and periosteum, the doctor takes into account the benefits for the woman and the possible risk for the developing fetus.
With the active spread of infection, suppuration, development of sepsis, severe complications against the background of the pathological process, it is possible to take certain groups of antibacterial agents. The new generation of antibiotics is less toxic to the fetus.
Under strict medical supervision, in the minimum effective dose, the following is prescribed:
- Ornidazole;
- Metronidazole;
- Josamycin;
- Azithromycin;
- Clarithromycin;
- Clindamycin;
- Cefepime;
- Ceftaroline.
The list of approved drugs is indicated by the dentist. The best option is to additionally consult with a gynecologist managing the pregnancy.
Anti-tuberculosis antibiotics are allowed to be used by pregnant women in combination with other drugs according to a specific regimen for a long period.
Contraindications to treatment with antibacterial drugs
Compositions for suppressing the inflammatory process in gingival and bone tissue during toothache are not suitable for all patients. Restrictions for use are related to age, body reactions, and special conditions. Most antibacterial drugs should not be used by nursing mothers or pregnant women.
Main contraindications for antibiotic therapy:
- allergic reactions;
- liver and kidney failure;
- intolerance to the active substance: you need to choose a substitute with another active ingredient;
- myasthenia gravis;
- damage to the optic nerve;
- severe diseases of the gastrointestinal tract;
- the patient is taking medications that are incompatible with a certain group of antibiotics;
- tendinitis;
- epilepsy;
- children's age (restrictions are indicated in the instructions for the drug).
A limited range of antibacterial compounds are used in pediatric practice.
It is important to clarify in the instructions the age of the child for safe antibiotic therapy for acute inflammation of tissues in the oral cavity.
In case of purulent inflammation, the development of periostitis and periodontitis, when the gums are swollen, the dentist selects effective antibacterial compounds. Many inexpensive antibiotics work well for dental inflammation and quickly suppress the pathological process. New generation drugs with a minimal list of contraindications and side effects are safer.
Antibiotics for toothache.
Many people consider antibiotics a panacea for all ills and, at the first problem with their teeth, begin to take them intensively. However, such self-medication can cause irreparable harm to other organs and systems of the body, without improving the condition of the teeth. Prescribing antibiotics is the exclusive prerogative of the doctor. In what cases are these medications prescribed?
Are antibiotics effective?
Before starting a course of antibiotics, you should determine the cause of your toothache. There are two main factors that provoke it:
- Caries that has developed to pulpitis. When the carious process affects the nerve, the tooth begins to react to various irritants: sour, sweet, cold, hot. Since in this case the pain is provoked by an intradental inflammatory process, antibiotics will be completely useless. For such pain, anti-inflammatory drugs, for example, Ibuprofen, are relevant. In addition to drug treatment, it is also planned to remove the affected tissue and fill the dental canals.
- An infection localized in a “dead” tooth. In such a situation, after removal of the nerve, the tooth does not react to sour, sweet and other irritants, but at the same time it hurts - and more and more every day. It's all about microbes that multiply either in an unfilled canal or in some tiny crack in the root. As a result, a purulent abscess or gumboil develops near the root of the tooth. The latter, by the way, is deadly. If such inflammation of the tooth root occurs, antibiotics are prescribed, but before taking them the patient will have to undergo the procedure of opening the abscess.
Before pinning any hopes on antibiotics, you should understand a few facts about this group of drugs:
- antibiotics help in treating the disease that provokes toothache, and do not relieve the pain itself (there are analgesics for this purpose);
- different antibiotics have different effects on pathogens, so it is almost impossible to successfully select such a medicine on your own;
- the effectiveness of taking antibiotics without concomitant dental treatment tends to zero.
The course of antibiotic treatment should not be interrupted prematurely: incomplete therapy will not lead to the desired result.
Diagnosis of tooth root cyst
To make a diagnosis and carry out appropriate treatment, the dentist collects and analyzes the medical history. During the initial diagnosis, many patients report the fact of endodontic treatment performed to eliminate periodontitis or pulpitis. Some patients indicate an exacerbation of the disease after intraoral dissection.
Radiography is used as the main diagnostic method. Below is a photo and x-ray of a dental cyst.
To obtain an x-ray, several methods are used, the first method is based on contact intraoral x-ray, the advantages of this technique:
- determining the degree of destruction of the jaw bones;
- assessment of the condition of the tooth root and tooth canal;
- assessment of the quality of canal filling;
- identifying the presence of perforations and fragments of instruments and materials in the tooth canal;
- determination of the relationship between the cyst and the roots located near the teeth.
The second method of performing radiography is an orthopantogram; the procedure is a panoramic photograph of both jaws and the maxillary sinuses of the upper jaw.
Another method of the procedure is a survey X-ray in the nasomental projection; the X-ray covers the bones of the skull from the nose to the chin; using the image, the doctor assesses the condition of the maxillary sinuses and detects cysts that have grown into the nasal cavity.
In addition to radiography, to detect a tumor, the patient may be prescribed an electroodontic diagnostic procedure. This technique helps to assess the degree of such an indicator as the electrical excitability of the teeth that are located next to the cystic tooth. If the value exceeds 60 microamps, the dentist prescribes endodontic treatment to the patient.
For diagnostic purposes, histological and cytological studies are used to determine whether the neoplasm is benign or malignant.
Diagnosing a dental cyst is not difficult, but only qualified dentists can carry it out in a hospital setting; under no circumstances try to independently determine the presence of a cyst and do not take therapeutic measures; strictly follow the doctor’s recommendations.