If you suddenly have a severe toothache and the pain is throbbing, sharp, unbearable, then such symptoms may indicate tooth pulpitis. What kind of disease is pulpitis, why does it appear, how can it be cured and the tooth saved? We will answer all these questions in detail in this article. After reading the material, you will learn how tooth pulpitis occurs, what methods of its treatment are used in modern dentistry, and whether it is possible to cure tooth pulpitis at home or not.
Pulpitis of the tooth and its treatment
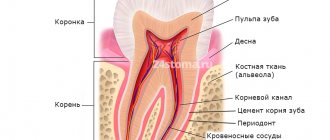
A characteristic sign of this pathology is inflammation in the pulp, which is located inside the tooth cavity, where blood vessels and nerves are concentrated. The cause of inflammation is the penetration of harmful bacteria into the cavity due to damage to the external dental tissues (enamel and dentin). This is the destruction that we most often owe to untimely treatment of deep dental caries: pulpitis becomes a consequence of the carious process. Much less often, it appears due to mechanical damage to the pulp, poor preparation of the tooth for filling, and unprofessional installation of orthopedic structures.
Treatment methods for pulpitis
In dentistry, two main methods are used to treat dental pulpitis in adults and children:
- biological - drug treatment of pulpitis with antibiotics and medications;
- surgical - treatment of pulpitis by amputation (partial removal of the pulp) or extirpation (in which the nerve of the tooth is completely removed).
The choice of technique remains with the dentist. The doctor studies X-ray diagnostic data, interviews and examines the patient. Based on these data, he selects the most rational method of treating pulpitis for a particular case.
Causes
Treatment of the disease primarily depends on the causes of its occurrence. Factors that often lead to inflammation:
- Untreated caries in a timely manner. In a mild form, the disease does not affect the pulp in any way, since the carious lesion extends only to the superficial tissues. As the crown is destroyed, caries affects all cellular structures and reaches the roots.
- Chronic periodontitis (except for mild forms). Deep periodontal pockets that form with this pathology reach the root plexuses. Pathogenic microorganisms that multiply in these cavities spread throughout the tooth and reach the pulp.
- Injury. Impact, bruise and other external influences contribute to the disruption of the established blood supply process and lead to a pathological process.
- Poor quality dental treatment. If the dentist did not clean the tooth cavity well before placing the filling, leaving carious particles, they will spread into deeper layers and reach the neurovascular bundle. Also, due to the fault of the doctor, the patient may receive a thermal burn of the pulp if the specialist neglected the rules while drilling the crown and did not cool it enough with water. The disease is also provoked by overdrying of the dentinal tubules by air flow.
- Exposure to acids, alkalis, medications, toxic filling compounds and other chemicals.
- Blood infection. Infection can penetrate into the pulp not only through carious holes, but also during sepsis.
- The patient's individual predisposition to tooth wear and the formation of mineral deposits in the pulp chamber.
Types of pathology
There are 2 main forms of the disease: acute and chronic. In the first case, a person suddenly experiences a sharp, paroxysmal pain (most often at night), which does not depend on external factors and does not go away when the irritants are eliminated. At first, a dark hole appears on the enamel, which grows over time and affects deep tissues, including reaching the canals.
If the inflammation does not go away after 3 weeks, the disease becomes chronic. Dull aching pains appear with a certain frequency and are disturbing not only at night.
Types of acute pulpitis:
- Focal. It is observed only for a few days. The pain lasts up to 20 minutes, with the intervals between attacks being about 2-3 hours. There is swelling of the gums.
- Diffuse. It extends to the coronal part, nerve endings and root. There is a disruption in the blood supply to tissues. The pain becomes throbbing and lasts much longer than with the focal form.
- Purulent. The cavity of the affected unit fills with pus. A painful pulsation is felt. The patient's condition is constantly deteriorating.
- Serous. Most often, this type is observed in children (pulpitis of temporary teeth). This is a pathology of infectious etiology, which is accompanied by short attacks of pain.
Classification of chronic dental pulpitis:
- Fibrous. Is a consequence of acute. It can proceed latently for several months with periodic periods of exacerbation. The gums are not swollen, the pain is aching and occurs infrequently.
- Gangrenous. This is a complication of acute fibrotic disease, in which the death of pulp tissue and destruction of the coronal part occurs.
- Hypertrophic. In the carious cavity, tissues of a bright red hue are clearly visible, which constantly bleed, especially when pressed.
Symptoms
Despite the fact that each type of disease has its own distinctive features, there is a list of symptoms characteristic of all forms of pathology. At the initial stage of the disease, the tooth begins to react painfully to cold and hot, as well as to other irritants. Then a sharp throbbing pain appears, which intensifies at night and when lying down. Soreness occurs spontaneously or under the influence of irritating factors.
External manifestations of the disease, regardless of its type:
- darkening of the enamel;
- tooth mobility;
- bleeding;
- redness of the gums;
- swelling of the tissues around the diseased tooth;
The chronic form of pulpitis can be asymptomatic. It is characterized by a putrid odor from the mouth and aching pain.
Important! Very often the patient cannot understand which tooth hurts. The pain may radiate to the neck or ears. To determine the location of inflammation, a doctor’s examination and additional diagnostic tests are necessary.
Diagnostic methods
To make an accurate diagnosis, the dentist conducts and prescribes the following studies:
- inspection of the damaged cavity using a mirror and probe;
- checking the tooth’s reaction to temperature fluctuations (thermometry);
- exposure of the crown to a weak electric current (electroodontodiagnosis), with the help of which one can distinguish the disease from deep caries and determine in what form it occurs;
- X-ray.
Features of treatment
The therapeutic regimen directly depends on the stage of the disease and the location of inflammation. Treatment methods for pulpitis used in dentistry:
- Biological. Only the source of infection is eliminated, the progression of the disease is stopped, and the inflammation gradually goes away. Medicines are introduced into the cavity, which stop the growth and reproduction of pathogenic microflora and help eliminate inflammation.
- Conservative (vitalization). The doctor preserves the living pulp, but removes its coronal part. The tooth is completely preserved, while its functioning is restored.
- Devitalization. A special paste is placed into the drilled hole, which promotes the complete death of the pulp. The neurovascular bundle is removed, then the specialist places a temporary filling. When tissue inflammation completely disappears, the filling material is replaced with a permanent one. Devitalizing paste is used by pediatric dentists for tooth pulpitis in a child.
- Surgical. Surgical removal is divided into amputation (partial removal of pulp tissue) and extirpation (the pulp is completely removed).
Attention! The sooner the patient contacts the dentist, the higher the likelihood that the tooth can be saved. A qualified doctor will be able not only to cope with swelling and inflammation, but also to restore the integrity of the crown and restore the lost whiteness of the enamel.
Is it possible to cure a disease with folk remedies?
Pulpitis requires qualified medical care and cannot be treated on its own. Home methods for relieving pain and reducing inflammation can only temporarily alleviate the patient’s condition. Without timely conservative or surgical treatment, severe complications are possible.
Possible complications
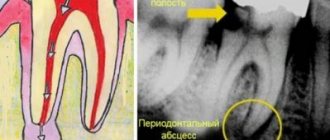
If you do not receive treatment on time or do it incorrectly, the risk of complications increases, such as:
- periodontitis (damage to hard tissues around the tooth root with pulpitis);
- periostitis (inflammation of the periosteum, or flux);
- abscess (purulent inflammation accompanied by intoxication of the body);
- sepsis (blood poisoning);
- chronic pathologies of internal organs and systems.
Preventive measures
In order to avoid long-term treatment and surgical intervention, you need to take care of the prevention of pulpitis by adhering to the following rules:
- brush your teeth 2 times a day, rinse your mouth after eating, remove plaque and tartar in a timely manner;
- visit the dentist for preventive examinations at least once every six months;
- do not use toothpicks or other traumatic devices;
- eat a balanced diet, ensure that the body receives a sufficient amount of vitamins and minerals;
- give up bad habits (smoking, drinking alcohol), large amounts of sugar and junk food;
- treat caries and other dental pathologies in a timely manner, without bringing them to severe stages.
Sharp pain radiating to the neck, temples or ears is a reason to urgently visit a dental clinic. If treatment is not started in time, serious complications are possible, including complete tooth loss and a septic process.
By following preventive measures, you can protect yourself from the occurrence of pulpitis and other oral diseases.
Biological method of treating pulpitis
If the disease has become chronic, a biological method or conservative treatment of pulpitis with calcium is used. The process involves applying therapeutic pads containing calcium preparations. The technique is also used in the following cases:
- if the pulp was accidentally exposed during the caries treatment procedure;
- when you need to strengthen the bone partition between tooth enamel and pulp.
The specialist applies a drug for the treatment of pulpitis to the site of thinning bone tissue and thereby strengthens it. Next, the tooth is filled and monitored over time, conducting X-ray examinations at certain time intervals. The method is suitable:
- children with baby teeth;
- patients under 30 years of age during the treatment of reversible pulpitis;
- everyone who takes special care of their oral cavity.
If, after treatment of pulpitis, the tooth aches, hurts when pressed or bitten, and the pain remains for a long time, intensifies at night, and becomes long-lasting, you must return to the clinic. Aching pain during the treatment of pulpitis indicates that more radical, that is, surgical, methods are needed.
How is pulpitis treated surgically?
As we have already noted, there are two possible options for surgical intervention:
- treatment of pulpitis using the amputation method with partial preservation of the pulp;
- treatment with complete removal of soft tissues, blood vessels, and nerves.
If there is an objective possibility, the doctor will remove only the top of the pulp - from the crown, leaving the root part. The blood supply and sensitivity (innervation) of the tooth will be preserved. The technique is used in the treatment of children - for milk or permanent teeth that have not yet fully grown. This allows them to form normally in the future. Treatment for pulpitis can be carried out in one visit.
Pulp - what is it for?
The pulp is a fibrous connective tissue penetrated by nerve endings and blood vessels.
Its shape completely follows the tooth, and is located in the center of the root part, filling the entire cavity. On top, the pulp is protected by a hard enamel layer, which prevents injury from the outside.
Main functions of the dental nerve:
- responsible for the formation, proper growth of teeth and blood supply;
- protects channels from pathogenic microbes;
- supplies the tooth with useful micro- and macroelements.
In addition, the pulp is responsible for the sensitivity of the tooth, that is, for its reaction upon contact with hot, cold, sour, sweet, and so on.
Reference! The dental pulp in adults is thinner than in children. This is due to age-related changes and a slowdown in regeneration processes. The older a person is, the thinner and weaker the nerve becomes, and the tooth begins to experience a deficiency of nutrients.
Treatment of acute pulpitis
The above methods are ineffective in treating exacerbations of chronic pulpitis, an acute disease when the tooth becomes a source of unbearable pain radiating to the ear, temple, and back of the head. With these symptoms, endodontic treatment of pulpitis is carried out - with cleaning of the root canals and complete removal of the pulp.
In dentistry, two modern methods of treating tooth canals for pulpitis are used: devital and vital.
- Treatment of pulpitis using the vital amputation method is carried out by removing the nerve, washing, cleaning and filling the canal.
- Devital treatment of pulpitis involves the use of medicinal pastes and requires several sessions.
These treatment methods are most often used for pulpitis on permanent teeth.
How long does pulp removal take?
On average, it takes about 40-50 minutes for pain relief, nerve removal, and root canal treatment. If the doctor administers high-quality anesthesia, it will take effect almost immediately, and the patient will not feel pain throughout the entire process. If the effect of anesthesia weakens during depulpation, an additional injection is given.
Reference! Before administering an injection with anesthesia, the doctor treats the soft tissue with a special freezing agent. That is, the patient will not experience pain either when inserting a needle into the tissue or during the process of removing the dental nerve.
Stages and stages of tooth treatment for pulpitis using the devital method
- Stage I.
The tooth is anesthetized and the carious cavity is cleaned. The pulp cavity is opened. - Stage II.
A devitalizing paste is placed into the exposed pulp and the tooth is filled for 3 to 7 days. People still call the paste “arsenic,” although it has nothing to do with this substance. - Stage III.
During your next visit, your dentist will clean the root canals according to medical protocol. - Stage IV.
If there is a risk that the tooth will crack, it is covered with a crown. If the hard tissues are well preserved or only slightly damaged, they are restored. The tooth is strengthened with a fiberglass or metal anchor pin and securely filled with photopolymer material.
The treatment time for pulpitis depends on how damaged the tooth is, the age of the patient, whether there are complications, and how many root canals should be treated.
Is it painful to treat pulpitis?
Many patients believe that treatment for pulpitis is painful. In fact, pain accompanies the disease itself, and not the procedure for its treatment. The pulp tissue and nerves become inflamed, which causes unbearable painful sensations comparable to an electric shock. Pulp removal is absolutely comfortable, because high-quality anesthetics completely relieve the patient of pain while the doctor prepares the canals. During treatment or after treatment of pulpitis, the tooth hurts when the internal tissues are severely inflamed. Then safe painkillers are prescribed while healing occurs (1 - 3 days).
Removal process
Depulping or removing a nerve always begins with preparation. To do this, the doctor must conduct a thorough examination of the oral cavity, collect information about the person’s health, and take the necessary tests. Only after this can he begin the nerve removal procedure, which is a simple operation lasting about 1 hour.
The first stage involves the administration of an anesthetic instead of surgery. Its effect begins after about 10 minutes and lasts for 1-2 hours, depending on the dose. General anesthesia, usually in the form of a sleeping gas, may also be used. The action begins literally in 1-3 minutes.
After this, the doctor begins preparing the working area, isolating the tooth from saliva, opening it and other manipulations. Only after this does the nerve extraction procedure begin. It is carried out using a pulp extractor - a dental needle in the form of a spiral. Next, the pulp chamber is filled with an antiseptic, the canals are carefully sealed, a control photograph of the patient’s jaw is taken, and a permanent filling is fixed.
previous post
Is it possible to build up a front tooth?
next entry
Possible complications
If you delay visiting the dentist, inflammation can spread to the bone tissue of the tooth - periodontium. This is how one of the most common and dangerous complications of this disease begins - periodontitis, which can lead to tooth extraction. Periodontitis also occurs due to an unskilled approach to cleaning root canals.
If you are concerned about an elevated temperature after treatment for pulpitis, urgently contact a more reputable dentist, as the inflammation is progressing. Professional clinics use modern methods of canal treatment using microscopes, binoculars, visiographs, endomotors, and apex locators. These instruments prevent the risk of complications.
Unfortunately, pulpitis remains a common occurrence after caries treatment. The reason for its appearance is the same - the unprofessional actions of a doctor who violated medical protocols and made mistakes when filling. Perhaps he accidentally opened the pulp and gave bacteria access to it.
What is pulp and does it need to be removed?
The pulp, or dental nerve, is the connective tissue that fills the tooth cavity. It consists of fibers, nerve endings, lymphatic and blood vessels. The dental nerve supplies bone tissue with nutrients, is responsible for the proper development of the tooth and protects it from infection.
If the pulp is damaged, an inflammatory process begins, and the person experiences severe pain. After removal of the nerve, the tooth becomes “dead,” but with professional manipulation by a doctor, it fully retains its functions.
How much does tooth treatment for pulpitis cost?
The final cost of pulpitis treatment is influenced by many factors: the degree of destruction of hard tissue, the number of canals in the tooth, the presence of complications, concomitant diseases, and the chosen treatment method. If the tooth is permanent and has one canal, then the procedure in Moscow clinics will cost from 5,000 rubles. This amount includes a full range of services: x-ray diagnostics, application of anesthetic, installation of a rubber dam, treatment of caries, treatment of dental canals with cleaning, installation of a filling. Price may change if multiple sessions are required.