Occlusion of the femoral artery is a violation of its patency (blockage).
As a result of the occlusion, arterial, oxygenated blood stops flowing to the lower leg. Ischemia develops (local anemia).
Femoral artery occlusion occurs mainly in men. Persons over 50 years of age account for up to 75% of cases of the disease.
Femoral artery occlusion can be:
- segmental, affecting only a limited area of the artery;
- complete, when the entire artery is affected;
- combined with occlusions of other arteries of the lower extremities.
Causes
Vascular occlusions are associated with a state of vascular insufficiency. The occlusion process occurs:
- as a result of injuries, if the artery is compressed.
- due to the fact that the lumen is blocked by a thrombus or embolus.
The formation of blood clots is promoted by a chronic disease - vascular atherosclerosis. As atheromatous plaques grow and increase in diameter, they interfere with normal blood flow. Atherosclerotic plaque leads to blood clotting and blood clot formation. Occlusion is caused by separated plaque fragments that move freely along the vascular bed. In addition, as a result of atherosclerosis, the walls of blood vessels lose their elasticity, become thinner and stratify under blood pressure, which causes the formation of aneurysms. Thrombosis or embolism is likely to occur in the area of the vessel where the dilatation has appeared.
Forecast and preventive recommendations
If the arterial lumen is blocked by half, the disease may occur without obvious signs. With such a picture, the risk of developing apoplexy is 10% of all cases within five years. A 75% vascular blockage leads to a 6% stroke rate in the first year. Complete thrombosis of the canal leads to inevitable neurological damage in 40% of incidents. Preventive surgical intervention with or without prosthetics makes it possible to reduce these risks to a minimum.
To prevent the closure of vascular walls, it is recommended to get rid of bad habits, balance your diet, and monitor weight gain. The lipid composition of the blood is determined by regular testing. If necessary, therapeutic recommendations help adjust the composition of the blood solution. If cardiac abnormalities are present, supportive treatment should be provided promptly. In case of congenital diseases of the cardiovascular system, it is also recommended to undergo regular examination as prescribed by a cardiologist.
Occlusion of cardiac vessels
A dangerous condition is considered to be acute occlusion of the coronary arteries, which supply blood to the heart muscle. This occurs as a result of atherosclerosis of the coronary arteries and coronary heart disease. If, during the chronic course of the disease, a person experiences angina pectoris, then the acute form is fraught with a heart attack and even death of the patient. Typical signs of cardiac vascular occlusion are chest pain that lasts more than 10 minutes and does not go away with rest or after taking nitroglycerin. In this case, the concept of acute coronary syndrome is used: a patient with such symptoms should be immediately hospitalized.
The danger lies in the fact that a person initially ignores the symptoms of coronary artery disease or simply does not feel them without taking any measures. Vascular occlusion is characterized by suddenness and unexpectedness, so at the first signs of developing coronary artery disease, consult a doctor immediately.
Occlusion and bite
Why does a patient come to the orthodontist? That's right: straighten your teeth and correct your bite... We have already talked about this (see here)
But what a bite is and what it is eaten with (especially what is a regular and incorrect bite of teeth) the patient usually does not have the slightest idea. For another patient, for example, what the bite and what the taste is unambiguous. That’s how they formulate it: “We’re... about this at Vkus ... like straightening it out.” Many of my colleagues are not far behind them: out of ten dentists I interviewed from different specialties (orthodontists, orthopedists, surgeons, therapists), only four were able to more or less clearly formulate what a bite . And on the question (desire) to justify and clarify the meaning of the concepts of occlusion and occlusion, every single one floated. How...
But such concepts as bite and occlusion are key not only in orthodontics, but in dentistry in general. Therefore, together with you and my colleagues, I would like to speculate on this topic and finally decide on the concepts of what kind of bite this is (which sometimes you really want to correct). And what exactly is correct and incorrect bite?
Dental occlusion is any (any) closure of the teeth of the upper and lower jaws. The key word here (both in the concept of occlusion and in the concept of occlusion) is closure . If there is no closure, this is no longer an occlusion. This is disocclusion (its absence).
Depending on the position of the lower jaw (and as you and I know, it is mobile), several types of occlusion are distinguished: central , anterior , posterior and lateral .
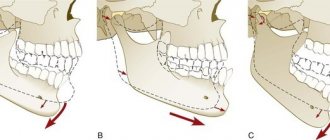
a ) Central occlusion; b ) Posterior (distal) occlusion; c ) Anterior (sagittal) occlusion
Central occlusion (CO) is something of an ideal or template. In life and practice, the practically unattainable, or rather, often simply not achievable (for various reasons). It is generally accepted that CO is characterized by three (although later we will understand that it is far from three) main factors: dental , articular and muscular .
Well, with the dental factor everything is clear: the teeth must close together. And preferably not anyhow, but in a clear order. But I’ll tell you about this a little later, when we talk about bite . What about the other two factors? Let me explain.
Joint factor CO (central occlusion). You and I know that the position of the lower jaw can be determined by the position of the articular heads of the temporomandibular joint (TMJ). Well, with central occlusion, the articular heads stand most evenly and correctly, reflecting the ideal position of the lower jaw relative to the upper jaw.
Let me remind you: the upper jaw, unlike the lower jaw, is practically motionless. It is tightly nailed (and in some cases screwed) to the skull. JOKE! We will have a separate conversation about fixing the upper jaw to the skull... Everything there is also very interesting and not so simple.
The ideally even placement of the articular heads of the lower jaw in the articular fossa of the temporal bone should be ensured by the most uniform and balanced work of certain muscles of the maxillofacial area. After all, it is the muscles that ensure the position of the lower jaw in space (in fact, like any other bone). Here you have the muscle factor .
I repeat once again - CO (central occlusion) is like a certain ideal that everyone seems to strive for, but getting it is something with something (does everyone, and does it always succeed?). Because just imagine how many confusing factors (and you can’t even imagine how many) are preventing you from achieving this ideal. Well, we'll talk about this later.
What about other types of occlusion? Everything is simpler here. He moved the jaw forward - anterior occlusion . Pushed it back (it's not that easy, right?) - you get posterior occlusion . The jaw is turned to the right and left (the only thing is that the teeth must be in contact) - this is lateral occlusion .
the
occlusion . What is a bite ?
“Bite is the closure of the teeth in the usual, static position of the lower jaw” (L.S. Persin)
Based on the very formulation of the concept of occlusion, its main feature is the closure of the teeth (occlusion) or the absence of their closure (disocclusion). And the connection to the position of the lower jaw (and it is this, as we have already said, that determines the type of occlusion), allows us to say that a bite is the closure of the teeth in the usual occlusion. Those. occlusion is a very special case of occlusion. And it turns out that it is purely individual.
Someone’s teeth may be perfectly straight and seem to fit together correctly (i.e., have the most multiple and dense contacts). Those. The bite is basically there. But the lower jaw (and the articular heads clearly show this) is shifted, for example, into lateral occlusion. And for a person this closure will be habitual (teeth close together better than ever). And it is this habitual closure that will be his bite. Individual. Which, by the way, due to the incorrect position of the lower jaw, it would be nice to correct it... Despite the possible complete “Hollywood” with teeth.
So it turns out that when the bite (the habitual closing of the teeth) coincides with the central position of the jaws (central occlusion), the bite is physiological. And with anomalies of occlusion, the usual position of the lower jaw does not coincide with the CO. And then the type of bite is determined by the position of the lower jaw, which is familiar to a person.
This is how a physiological bite is distinguished from an abnormal one .
The concepts of physiological occlusion and physiological occlusion are identical. In the case when there is a problem with the closure of the teeth, but their closure still takes place, we can talk about an malocclusion (occlusion). For example: distal occlusion, mesial occlusion, etc. Those. There is closure of the dentition, it’s just disturbed. When there is no closure of teeth at all, then they don’t talk about bite. In this case it simply does not exist. Just as there is no occlusion. Therefore, for example, it is wrong to diagnose “open bite.” If there is no bite, it means disocclusion.
Physiological occlusion has a number of signs:
Fig.1:
Fig. 1: The upper lateral teeth overlap the lower ones to the depth of the longitudinal fissure (b) , and in the anterior section the upper incisors overlap the lower ones by no more than 1/3 of the height of their crowns (a)
Fig.2:
Fig. 2 : Each tooth intersects with two antagonist teeth (a) . In addition to the lower central incisors and the upper last teeth (they have one antagonist each) (b)
Fig.3:
Fig. 3: Each upper tooth intersects with the lower and posterior lower teeth of the same name (a) . And each lower one has the same upper and front upper teeth (b)
Fig.4:
Fig. 4: The midline should pass between the central incisors
Fig.5:
Fig.5:
• On the upper jaw, the dental arch is larger in diameter than the alveolar arch, and the alveolar arch is larger than the basal (jaw)
• On the lower jaw it’s the opposite: the basal arch is the widest, then the alveolar, and the narrowest is the dental
Fig.6:
Fig. 6: The teeth of one jaw are in contact with each other pointwise, on approximal (lateral for incisors and canines, and anterior-posterior for premolars and molars) surfaces
Fig.7:
Fig. 7: The height of the tooth crowns decreases from the central incisors to the molars, with the exception of the canines. The upper teeth are inclined outward (vestibular), and the lower teeth are vertical
Fig.8:
Fig. 8: The first molars, with their mesial-buccal cusp, enter the intercuspal fissure of the lower molar of the same name
Now we understand what, what closure (as a result of treatment) we should strive for? Although this is just the “external” part of the occlusion (bite). And in the modern interpretation, occlusion (occlusion) is not only the teeth and their closure. Everything there is much deeper and more interesting. But we'll talk about this a little later...
There are also closure of baby teeth ( deciduous occlusion ), closure of permanent teeth ( permanent dentition ) and mixed occlusion (closing of teeth during the period of change of baby teeth to permanent ones).
Well, we seem to have determined the guidelines for the “correct” bite. Have you read it? Remember. Great. Now... forget it. Why? Yes, because the landmarks here are the teeth. Only teeth. And teeth are a very superficial and very unreliable guide. Dependent on many other guiding factors. This means that it is at least unreasonable to determine the “correctness” or “incorrectness” of a bite only by the closure of the teeth. This is unreliable. Not exactly. It is fraught with errors and problems, which we see almost every day.
Unfortunately, in the vast majority of cases, all orthodontic treatment is based on these “unsteady”, unreliable “purely dental” guidelines. Yes, not only orthodontic, but dental in general. Prosthetics, implantation, and dental restoration also rely on the teeth themselves. Only on the teeth. In fact, the goals and objectives of dental (and orthodontic, including) treatment very often boil down only to “attracting” teeth to each other. And a prosthetic device is inserted into the lung and implanted. Getting a certain external effect, the appearance of a “correct” bite, the illusion of successful treatment. And then comes the reckoning...
Expensive crowns and bridges break for no apparent reason. The implants fall out or become inflamed. And crooked teeth are corrected in the wrong direction. And with the temporomandibular joint, the problem suddenly pops up out of the blue. And this, by the way, is really a problem, since you won’t find specialists in TMJ during the day. No, of course there is a lot of advertising and show-off. Has anyone seen the results?
Or even more abruptly: problems of a different order begin, seemingly far from the teeth: the lower back aches, the head hurts, the pressure jumps, the body somehow reacts negatively to the weather... And endless trips to neurologists, neurologists, psychotherapists, osteopaths, and other “atams” begin ", "-istam", and "-ologam". Endless, because these specialists usually also see nothing except “their” sore.
And it is not known that these troubles, including the incorrect formulation of the concepts of occlusion and occlusion, are to blame. But naturally, it is the patient who pays for this “broken aim.” Not with money (or rather, not only with money). The main thing, and the saddest thing, is your health. And often without even realizing that the cause of many (oh, many) sores is an incorrect, and sometimes incorrectly corrected, bite. And why all? Yes, because the attitudes and dogmas on which modern dentistry exists have not changed, by and large, for a hundred and fifty years. And what then is the “modernity” of today’s dentistry? Only in the fruits of technological progress? It turns out to be some kind of “race in width”. You look at the topics of training seminars and it makes you feel sick. What are they talking about: “which braces are cooler...”, “which fillings are better...”, “which ceramics are more beautiful...”. And what? Just spend your life on this? Is it hard to dig deep?
And the very formulation of the concepts of occlusion and occlusion , as the main guidelines in dental treatment, is high time to change. Otherwise we will remain Neanderthals. Savages armed with modern equipment. Incapable, with all their “weapons”, of competent treatment, of real help.
Are you upset? Understand. But let's figure it out...
So let’s start right away with the formulation of the bite. Remember what it sounds like? “Closing of teeth in habitual occlusion.”
Closing teeth . Where do teeth come from? That's right - from the jaws . And if, say, the jaw is in the wrong position, or is deformed, will this affect the closure of the teeth or not? Of course yes.
And where does the jaw (let’s take the upper one) grow from? Let's remember the anatomy... That's right - it is attached to the skull . To the very base of the skull. And if the cranial bones are deformed, or are in the wrong position (displaced as a result of injury), can this be reflected in the position of the upper jaw? Maybe. And therefore, such a displacement will also affect the closure of the teeth (bite). How interesting, right?
What about the lower jaw? In general, it also seems to be “attached” to the skull. Through the temporomandibular joint (TMJ). And an integral part of the joint is the temporal bone (skull bone!!!). More precisely, its articular fossa. And if the temporal bone is, for example, in some kind of external rotation (and this is quite common), do you think this will have any negative consequences for the lower jaw and lower teeth (and further for occlusion)? And there is no need to think - the answer is obvious.
In addition, the lower jaw (its position) is directly dependent on the position of the upper jaw. The dependence is approximately the same as a door depends on the door jamb: the jamb is smooth and the door does not creak. And it opens normally. And the jamb is crooked - and the door is also incorrectly positioned, which leads to problems with its opening and closing...
And it’s the same with the jaws: if the upper jaw is deformed or incorrectly positioned in space (by itself or due to “distortions” of the cranial bones), then the lower jaw is forced to adapt to the “wrong” upper jaw. And how is the adjustment (forced position) ultimately ensured and carried out? Yes, the teeth are compensatory and incorrectly positioned. Here you go: get the wrong bite.
Go ahead. And what does the skull “contact” with anatomically? That's right - with the spine. This means that any problem with posture (scoliosis of some kind) will immediately cause a compensatory restructuring of the bones of the skull. And with them the upper jaw. And then, as in the fairy tale about the turnip: the spine bent - the skull “moved” - followed by the upper jaw, followed by the lower jaw. Plus, the dentition is compensatory deformed... (read the mechanism above). The “exit” is, again, the problem of teeth closing.
One thing needs to be understood: teeth are part of the skeleton . And the skeleton is a closed kinematic system. Everything in it is built on compensation (to maintain balance). And we still treat flat feet separately. Separately, we “correct” the posture. And we are separately trying to solve the problem of teeth closing (occlusion). And we are also surprised when something “not very good” comes out.
Or on the other hand... Imagine if you thoughtlessly “correct your bite” and “straighten” your teeth. As many people think, put on braces and wear them for a year and a half. That's all. Happiness will arrive. And the fact that by “correcting” the bite we have “corked” all the skeletal distortions (unaccounted for), as if with a cork – how is that? What then is the treatment? And how (what problem) will the patient pay for straight teeth?
Even a hedgehog has long understood that the closure of teeth depends on many “non-dental” factors. And that the bite is not just teeth. That is why there is a need (long overdue) to expand our understanding of what occlusion and dental occlusion . And give a more precise formulation of these concepts.
READ CONTINUED…
Sign up for diagnostics
Social Like
Comments for the site
Cackl e
Peripheral vascular occlusion
Large arteries of the extremities, more often the lower ones, are susceptible to vascular occlusion. Occlusions are an unpleasant consequence of vascular diseases of the legs. At the same time, the threat of an acute occlusive process in this area is dangerous due to the development of tissue necrosis, which leads to amputation of the affected limb. Characteristic signs of thromboangiitis obliterans, atherosclerosis of leg vessels and other common pathologies are:
- pain in the legs that does not go away with rest;
- pallor of the skin of the extremities;
- coldness in the legs;
- tingling sensation, numbness in the limb;
- impairment of motor functions of the limb.
If these symptoms appear, it is recommended to immediately examine and treat the vessels of the extremities: the slightest delay can result in the development of gangrene. In the early stages of the development of the disease, treatment of obliterating atherosclerosis of the lower extremities and other pathologies of sclerotic origin is carried out using conservative methods, whereas in an advanced form it is difficult to fight the disease.
Occlusive processes occur in the arteries of the kidneys, resulting in the development of renovascular hypertension and kidney dysfunction. The aorta is also affected, since it is the largest vessel. Read about the consequences of aortic atherosclerosis by clicking on the link.
Signs of carotid artery occlusion
The symptoms of the disease largely depend on the location of the abnormal area, the speed of the lesion, and the anatomy of the branching of alternative blood networks that supply the brain during the period of blockage of the main ducts. Most often, pathogenic blockage develops at a slow pace, so the circulatory system has the “opportunity” to adapt to new, unfavorable conditions. The functionality of the brain regions is preserved, but chronic ischemic disease is steadily developing. Sudden blockage leads to immediate apoplexy.
If the blood “paths” are affected on both sides, the symptomatic picture is more complex, and the prognosis for subsequent recovery is less favorable. The severity of the course and manifestations is high. The first sign of carotid compression is a transient ischemic attack (TIA). The larger the area of damage to the cerebral cortex, the longer the attacks last. The patient feels numbness of the skin of the facial part on the opposite side of the abnormal zone. Fingers go numb, muscle weakness occurs in the upper limb. On the side of the disorder, there is a partial or complete loss of visual perception. Spots, “interference,” and darkening appear before the eyes until vision is completely lost for some time. Some episodes may include headache, hallucinations, swallowing dysfunction, nausea, and loss of coordination. A small percentage of patients complain of seizures or widespread epileptic seizures.
Two thirds of patients after one or more TIAs suffer an ischemic stroke, the symptoms of which are similar to the described attacks, but after time they do not go away (visual disturbances persist, numbness does not go away, neurological deficit is observed). Only correct treatment can change the situation towards alleviating symptoms.
If the alternative branches of the blood distribution system are well developed, then blockage of the carotid carotid tissue can proceed unnoticed, and degenerative lesions do not occur. Otherwise, there is a possibility of ontogenesis of bilateral closure of the walls, which leads to extensive apoplexy, coma and death.
Occlusion of blood vessels supplying blood to the brain
Occlusive processes in the arteries supplying the brain are fraught with dangerous consequences. Impairment of cerebral blood supply is fraught with the development of a stroke or ischemic cerebral infarction, and this often ends in the patient’s death, paralysis or dementia. A common cause of this is carotid artery occlusion. It is accompanied by loss of consciousness, nausea and vomiting, impaired coordination, speech and vision, weakness and numbness of the limbs. A harbinger of strokes are transient (cerebral) ischemic attacks, which we described in detail earlier.
How to diagnose pathology?
To diagnose abnormal clamping of the CC pathways, a comprehensive neurological examination is performed. The most accessible technique is ultrasound screening of head and neck vascular tissues. The most informative method confirming the initial diagnosis is angiography of cerebral vessels. Angiography is used in difficult cases, as well as before instrumental intervention (for planned surgery).
Magnetic resonance angiography is as safe and informative as possible due to the inaccessibility of other diagnostic methods. Additionally, a referral is made for a nuclear resonance scan of the brain. With joint hardware diagnostics, damage to the carotid “traces” is 100% detected.
Computer scanning helps to identify areas affected by oxygen deprivation. Color differences in degenerative areas in the resulting images help differentiate different types of ischemia. This type of disease can be determined only after 2-3 days. In the first hours of ischemia development, changes in brain tissue are not visible. Destruction can be determined only by indirect signs.
Tests and diagnostics
It is recommended to consult a doctor at the first manifestations of the disease. After examination, collecting anamnesis and assessing the manifestations of clinical symptoms, they begin diagnostics, which includes:
- CT arteriography;
- Doppler ultrasound;
- cerebral angiography;
- MR angiography;
- coagulogram;
- MRI of the brain.
Only after a comprehensive examination is appropriate treatment prescribed, which is selected individually for each patient.
Techniques for correct positioning of the lower jaw
Correct positioning of the patient's jaw in the position of central occlusion involves the use of two methods of placement: functional and instrumental.
The main condition for correct placement is muscle relaxation of the jaw muscles.
Functional
The procedure for carrying out this method is as follows:
- the patient moves his head back slightly until the neck muscles tense, which prevents protrusion of the jaw;
- touches the tongue to the back of the palate, as close to the throat as possible;
- at this time, the specialist places his index fingers on the patient’s teeth, lightly pressing on them and at the same time slightly moving the corners of the mouth in different directions;
- the patient imitates swallowing food, which in almost 100% of cases leads to muscle relaxation and prevents jaw protrusion;
- When bringing the jaws together, the specialist touches the surfaces of the teeth and holds the corners of the mouth until it is completely closed.
In some cases, the procedure is repeated several times until complete muscle relaxation and correct reduction of both rows are achieved.
Instrumental
It is performed using specialized devices that copy jaw movements. It is used only in extremely serious situations, when bite deviations are significant and it is necessary to correct the position of the jaw using the physical efforts of a specialist.
Most often, when carrying out this method, the Larin apparatus and special orthopedic rulers are used, which make it possible to record jaw movements in several planes.
Treatment methods for central retinal artery thrombosis
Treatment of occlusion must begin literally in the first hours after complaints about the absence or decrease in vision, otherwise it will be impossible to restore it. Primary emergency care should include massage of the eyeball, which will help restore blood flow to the central nervous system. To reduce IOP, instillation of eye drops, the use of diuretics, and corneal paracentesis are recommended.
If occlusion of the central retinal artery is caused by spasm of the arterioles, pathogenetic therapy is supplemented by the appointment of vasodilators (sublingual nitroglycerin, intramuscular papaverine, intravenous aminophylline, etc.), carbogen inhalation or hyperbaric oxygenation.
In case of thrombosis of the central nervous system, it is necessary to use thrombolytic agents and anticoagulants, intravenous infusions of dextrants, and probing of the branches of the ophthalmic artery through the supraorbital artery.
Any type of central artery occlusion requires the use of antioxidants, local retrobulbar and parabulbar injections of vasodilators, and instillation of b-blockers. At the same time, corrective therapy for concomitant systemic pathology should begin.
The effectiveness of treatment of central retinal vein occlusion directly depends on the efficiency of its implementation and is especially high in the first hour from the moment of thrombosis.
General information
Vascular occlusion is a blockage (more often of arteries than veins), which is characterized by a pronounced decrease in the speed and quality of blood flow. Occlusion can cause necrosis and, as a result, lead to death.
The pathology is quite common and can affect the organs of visual perception, the central nervous system, limbs and great vessels. sepsis and peritonitis develop . Abdominal ischemic syndrome develops against the background of a lack of adequate blood circulation in the digestive tract. The pathology is associated with occlusion of the unpaired visceral branches of the abdominal aorta - the celiac trunk and mesenteric arteries (superior, inferior). Abdominal toad can develop under the influence of both internal ( thrombosis ) and external factors (traumatic occlusion).
What is an occlusive dressing?
This method of sealing the lesion is used for wounds that require maintaining sterile conditions and protection from the external environment.
Applying an occlusive dressing to the knee joint requires certain skills and technique:
- cover the wound surface with sterile gauze;
- Place the top of the scarf on the thigh area and wrap it around the waist;
- bend the bandage at the base by 2 cm;
- cross the ends under the thigh, tie knots on the thigh;
- Throw the top over the knot formed and then pass it under the knot.
Errors allowed
Creating a prosthetic structure in conditions of malocclusion is a most complex orthopedic procedure, the quality of which depends 100% on the qualifications of the specialist and a responsible approach to work.
Violations in determining the position of central occlusion can lead to the following problems:
The bite is too high
- The folds of the face are smoothed, the relief of the nasolabial zone is poorly defined;
- the patient's face looks surprised;
- the patient feels tension when closing the mouth, while closing the lips;
- the patient feels that during communication the teeth are knocking against each other.
Low bite
- The folds of the face are strongly pronounced, especially in the chin area;
- the lower third of the face visually becomes smaller;
- the patient becomes like an elderly person;
- the corners of the mouth are lowered;
- lips sink;
- uncontrolled salivation.
Permanent anterior occlusion
- There is a noticeable gap between the front incisors;
- the lateral elements do not contact normally, tubercle reduction does not occur.
Permanent lateral occlusion
- Overbite;
- clearance on the offset side;
- shifting the bottom row to the side.
Reasons for such problems
- Incorrect preparation of wax templates.
- Insufficient softening of the material for taking impressions and impressions.
- Violation of the integrity of wax forms due to their premature removal from the oral cavity.
- Excessive jaw pressure on the ridges during impression taking.
- Errors and violations on the part of the specialist.
- Errors in the work of the technician.
The video provides additional information on the topic of the article.
Methods used
Central occlusion is determined at the stage of manufacturing prosthetic structures when several units are lost.
This is necessary to ensure the normal functioning of the product and eliminate the occurrence of deviations and problems in the functioning of the temporomandibular joints.
In this case, the height of the lower third of the face is of great importance. However, in the absence of a large number of units, this indicator may be violated and must be restored.
If the patient has partial adentia, several options for determining the indicator are used.
The presence of antagonists on both sides
The method is used when antagonists are present in all functional areas of the jaws.
In the presence of a large number of antagonists, the height of the lower third of the face is maintained and fixed.
The occlusion index is determined based on as many contact zones as possible of the same units of the upper and lower rows.
This option is the simplest, as it does not require the additional use of occlusal ridges or specialized orthopedic templates.
Presence of three occlusion points between antagonists
This method is used if the patient still has antagonists in the three main contact zones of the rows. At the same time, the small number of antagonists does not allow normal positioning of plaster casts of the jaw in the articulator.
In this case, the natural height of the lower third of the face is disrupted, and occlusal ridges made of wax or thermoplastic polymer are used to correctly match the casts.
The roller is placed on the bottom row, after which the patient brings his jaw together. After the roller is removed from the oral cavity, imprints of the antagonist contact zones remain on it.
These prints are subsequently used by technicians in the laboratory to position the casts and create a fully functional and correct, from an orthopedic point of view, prosthesis.
Absence of antagonistic pairs
The most labor-intensive scenario is the complete absence of the same elements on both jaws.
In this situation, instead of the position of central occlusion, the central relationship of the jaws is determined .
The procedure includes the following steps:
- Work on the formation of a prosthetic plane , which is positioned along the chewing surfaces of the lateral units and is parallel to the beam. It is built from the lower point of the nasal septum to the upper edges of the ear canals.
- Determination of the normal height of the lower third of the face.
- Fixation of the mesiodistal relationship of the upper and lower jaws using wax or polymer bases with occlusal ridges.
Checking central occlusion with existing pairs of elements of the same name is carried out by closing the teeth and is carried out as follows:
- a thin strip of wax is placed on the already prepared and fitted contact surface of the occlusal roller and glued;
- the resulting structure is heated until the wax softens;
- heated templates are placed in the patient’s oral cavity;
- After bringing the jaws together, the teeth leave imprints on the wax strip.
It is these fingerprints that are used in the process of modeling central occlusion in the laboratory.
If, during the process of determining occlusion, the surfaces of the upper and lower rollers close, the specialist adjusts their contact surfaces.
Wedge-shaped cuts are made on the upper one, and a certain amount of material is cut off from the lower one, after which a wax strip is glued to the treated surface. After the rows are brought together again, the strip material is pressed into the cutouts.
The products are removed from the patient’s mouth and sent to the laboratory for subsequent production of a prosthesis.
Diet for occlusion
To restore the elasticity of the vascular wall, strengthen it and reduce the severity of occlusion, it is recommended to adhere to certain dietary rules. In case of occlusion, it is recommended to adhere to a special cholesterol-lowering diet, which includes:
- Legumes . Beans and legumes are sources of protein, iron, folic acid and contain absolutely no fatty acids.
- Whole grains (wheat bread, buckwheat, oatmeal and brown rice).
- Cabbage (all types, especially broccoli). Prevents salt deposition, normalizes the lipid spectrum of cholesterol, enriches the body with vitamins K and C.
- Asparagus . Helps lower blood pressure and reduce cholesterol in the blood.
- Persimmon . Rich in fiber and has a pronounced antioxidant effect.
- Spinach . Allows you to reduce blood pressure in hypertensive patients.
- Turmeric . It has an anti-atherosclerotic effect, reduces the volume of cholesterol plaques, and reduces the severity of the inflammatory process.