Dentinogenesis imperfecta type I
Pathology is always combined with osteogenesis imperfecta. It occurs more often in men, frequency - 1:50,000. General clinical signs may vary depending on the type of inheritance. Teeth wear out quickly and become more intensely colored, and are sometimes affected by caries. In permanent teeth, the clinical picture varies. On examination, the bulbous shape of the teeth and root fractures are noticeable.
The diagnosis is confirmed by x-ray. The image shows thinning of the cortical layer of the jaw and the coarse structure of the spongy substance. After eruption, obliteration of the roots begins, which slowly progresses.
The main pathological signs are:
- normal enamel structure;
- enamel-dentin junction in the form of a straight line;
- a decrease in the number of dentinal tubules in the peripulp dentin, their uneven diameter, narrowing and obliteration;
- deficiency of dentin mineralization;
- absence of conversion of precollagen fibers into collagen fibers.
Classification
Since amelogenesis imperfecta belongs to a genetically and clinically heterogeneous group, its classification was not easy to create. The first systematization was based on phenotype and had 2 types of disease. Then scientists identified 5 groups of pathology, and later presented four main types, which were based on phenotype, as well as inheritance. The comprehensive latest systematization takes into account the type of inheritance, molecular defect, phenotype, and biochemical analysis. The occurrence of the form of AN depends on the disturbances that occur in the enamel matrix.
Hypoplastic
The genetic type of this disease is the main one. It is characterized by the correct stage of formation of the enamel layer. But he's not thick enough. The affected areas are often on the surface of the buccal areas. Oval depressions or pits of varying depths, as well as grooves of varying lengths, are clearly visible. The layer is quite hard. Its surface can be rough, smooth, or granular. Healthy areas retain their shine. The depth of the defects affects the color intensity. With deep lesions, dentin is exposed.
Hypomaturation
With this form, the enamel has normal thickness, despite problems in matrix maturation. But the layer quickly becomes insufficiently hard, and the surfaces of the crowns lose their shine.
Hypomineralized
Qualitative changes occur when the matrix is mineralized. This is a rare group of pathologies that is detected in 3 percent of patients. After the eruption of the chewing organs, the thickness of the enamel is normal, the surface of the crowns is smooth.
Hypomaturation with taurodontism and hypoplasia
With such a defect, a failure occurs during tissue differentiation, as well as during the layering of the enamel matrix.
For any form of anomaly, patients should use the services of a dental clinic. Only a modern clinic with advanced equipment will help the patient get rid of the problem. The sooner you see a doctor, the easier the treatment will be, the faster the recovery period will end.
Type II dentinogenesis imperfecta
This pathology is otherwise called hereditary opalescent dentin, or “crownless teeth.” It occurs with a frequency of 1:8000, develops in an autosomal dominant pattern and has another name: Stainton-Candepont syndrome. As a rule, the disease is not combined with general diseases.
The enamel turns watery gray, amber or purple-blue, and the teeth become translucent. Sometimes the crowns take on a purple hue and are shaped like an onion. 2-4 years after teething, the enamel begins to actively chip off. The occlusal surface of the teeth is characterized by increased abrasion, and exposed dentin turns brown.
Additional clinical signs include increased electrical excitability of the pulp and a possible delay in root resorption of primary teeth. In some patients, on the contrary, early replacement of milk teeth with permanent teeth is observed, and caries is rare with this pathology.
X-ray signs:
- the roots may be shortened, with hypercementosis, with foci of clearing in the apical area;
- dental cavities are reduced, the canals are narrow or obliterated, which is a consequence of progressive calcification;
- the height of the crowns is reduced due to rapid abrasion;
- There are areas of rarefaction of bone tissue in the area of the root apexes.
Pathomorphological features:
- The structure of the enamel is disrupted, the tissue becomes thinner, the number of organic plates increases, and areas of structureless enamel are noticeable.
- At the enamel-dentin junction there is a straight line.
- The structure of dentin is heterogeneous.
- The number of tubes in the peripulpar dentin is reduced; they are short, curved, expanded and grouped in several pieces.
- The amount of interglobular dentin increases.
- In dentin, the amount of mineral substances decreases (60%), while the amount of water (25%) and organic substances (15%) increases.
- Hydroxyapatite crystals are replaced by an amorphous structure.
- The dentin matrix has an atypical structure, and predentin is expanded.
- The number of odontoblasts decreases, the shape of the cell and nucleus changes, processes are absent, and in some cases the odontoblasts themselves are absent.
- The pulp has few vessels, but many denticles and fibers.
- Degenerative changes in the cement are noticeable.
Diagnostics
One of the most important stages in diagnosing this pathology is collecting an anamnesis coupled with identifying unfavorable hereditary factors. The clinical manifestations of the disease directly depend on its form.
On physical examination, a change in the shade of tooth enamel is observed. The crown takes on a spherical shape and noticeably narrows in the neck area. Additionally, severe abrasion is detected in combination with a “decrease in the lower third of the face.”
It is necessary to differentiate dentinogenesis imperfecta not only from amelogenesis imperfecta, dentin dysplasia, acid necrosis, anomalies of tooth development, but also from other pathological changes in dentin associated with a number of other, more rare diseases. In particular, it is necessary to mention brachioskeletogenital syndrome, marble disease, hypophosphatasia, and Ehlers-Danlos syndrome.
In order to identify genetic factors in the occurrence of pathology, a medical genetic consultation may be indicated.
Type III dentinogenesis imperfecta
This form is rare and is considered an isolated hereditary form of wine opalescent dentin. With it, the crowns of the teeth take on the shape of a bell. Multiple openings are noticeable in primary teeth. The x-ray shows a contrasting contour of the tooth with internal enlightenment. This is explained by the fact that after the formation of the outer covering layer, dentin production ends.
Symptoms
Clinical manifestations are directly related to the type of disease. In patients, the enamel layer becomes thinner, the shade of the crowns changes, and their transparency is impaired. Depressions in the enamel or its absence are diagnosed. In details:
- With a hypoplastic type of pathology, the shape of the units is normal, and the thickness is slightly reduced. Cup-shaped depressions on molars lead to chipping of the cusps, a decrease in the height of occlusion, and less often to displacement of the head of the jaw joint. The shade of enamel is yellow or brown. Hyperesthesia to hot or cold is noted, tremors sometimes appear, and the eruption of units is often delayed.
- The hypomaturation type is characterized by a reduced content of minerals in the enamel layer, an amber or matte white tint of the crowns, vertical stripes, and small dots on the surface. High abrasion and chipping cause hyperesthesia. The clinic resembles fluorosis.
- With the hypocalcification form, the color of the crowns changes, there is no shine, and the structure of hard tissues is disrupted. Over time, soft enamel separates from the dentin. Defects are often localized on the front incisors, as well as on the cusps of molars.
- With hypomaturation with hypoplasia, opaque dots on the enamel are visible. There is a difference in color between the deciduous and primary units. Due to chips, the shape of the chewing organs becomes different: cone-shaped, cylindrical, rounded.
Associated symptoms may include bleached hair, thickened skull bone, and enlarged pulp chambers. Such patients are afraid of light in childhood, and their central visual acuity may decrease.
Treatment of dentinogenesis imperfecta
Unlike the treatment of pulpitis of baby teeth or caries, with this diagnosis, mainly orthopedic rather than therapeutic dentistry is possible. If the primary teeth are completely worn down, complete plate-type dentures are made and placed over the roots. With their help, they monitor the functional load when chewing, and also provide optimal conditions for changing the bite to a permanent one. The prosthesis also maintains the myodynamic balance of the masticatory muscles, the height of the bite at the beginning of its formation, and compensates for aesthetic defects.
If the teeth are not completely worn down, individual thin-walled stamped crowns are made to maintain the height of the bite. They also cover permanent molars and incisors that have just erupted. These actions are aimed at stopping the abrasion of hard tooth tissues and increasing the height of the bite.
Once the permanent teeth have fully erupted, the temporary crowns are replaced with permanent ones. Due to obliteration of the root canals, the manufacture of pin structures is excluded, however, parapulp pins and composite materials can be used to build up missing tissues before prosthetics.
Causes
The disease is hereditary. Problems arise as a result of a genetic mutation. Paths of inheritance: autosomal dominant, X-linked, autosomal recessive. The anomaly is observed when the patient's maxillary arch is narrowed, as well as when its growth is vertical. The pathology is diagnosed when the patient has an open skeletal occlusion, with a reverse Spee curve. Amelogenesis imperfecta in children is associated with disorders that occur during the formation of the enamel layer by ameloblasts. The layer can be very thin or completely absent; small teeth with a gray or brown tint are formed. When the milk organ changes to a permanent one and new dentin appears, the yellowness of the crowns increases.
Transfer of mutated material can occur via the X chromosome or autosome. The probability of a defect occurring is 25-50%. Pathological activity of the KLK4 gene leads to the formation of crystals of smaller thickness. The formation of an enzyme such as calcium-dependent proteinosis is encoded by the MMP-20 gene, which has a negative effect during the formation of the organic matrix. Osteogenesis is regulated by the DLX3 gene. When it is damaged, amelogenesis does not proceed properly, and taurodontism may occur.
Treatment of dental fluorosis in children
Treatment methods depend on how far the process of destruction of the enamel or the tooth itself has progressed.
- For streaked and spotted forms of fluorosis, dentists use microabrasion and remineralizing therapy of tooth enamel.
- If the integrity of the enamel is noticeably damaged, the surface is restored by filling and/or microprosthetics.
- In case of erosive and destructive forms (deep damage to dental tissues), it is necessary to use metal and ceramic crowns, as well as structures to fix the remaining part of the tooth.
Dental hypoplasia in children: causes
Hypoplasia of primary teeth in children often develops due to the condition of the mother during pregnancy and disruptions in the process of formation of tooth buds in the fetus. Particularly dangerous are diseases such as toxoplasmosis, rubella, severe forms of toxicosis, and Rhesus conflict. Prematurity and illnesses suffered immediately after birth can also subsequently cause systemic enamel hypoplasia.
A special cause of severe systemic hypoplasia is the use of the antibiotic tetracycline by a woman during pregnancy or by a child in infancy. In this case, the teeth darken, the enamel is destroyed, and sometimes it may be completely absent (enamel aplasia).
Hypoplasia of permanent teeth in children develops due to diseases suffered at the age of 6-18 months, when the rudiments of future teeth are formed:
- Severe ARVI;
- Intestinal infections;
- Digestive pathologies;
- Vitamin D deficiency, rickets;
- Dystrophy, lack of nutrients.
Provoking factors
Since dentinogenesis imperfecta is a hereditary disease, gene mutations that manifest themselves at the stage of bone formation, blood vessels and dentin formation in the fetus act as provoking factors.
The role of other risk factors for the development of pathology is unclear. However, it is obvious that the general state of health, immune status, quality of nutrition and oral care, injuries, and lack of planned sanitation of the oral cavity have a negative impact on the development and severity of the disease.
Therefore, the role of preventive measures against any dental diseases remains important in this case.
07/31/2015 Causes of tooth discoloration
The reasons for tooth discoloration can vary. What to do in this or that case, what result to expect, what treatment plan to suggest so that the patient does not suffer disappointment? This article reflects all possible options for color changes, and understanding the mechanism of discoloration will help you choose one or another treatment tactic. Discolors are divided into:
- internal
- external
- acquired
In the ICD-C classification, tooth color changes are divided into two groups - those occurring before and after teething.
- Changes that occur before tooth eruption are considered in category K00.8 “Other disorders of dental development.” The following nosological forms are distinguished in this category:
- K00.80 Change in tooth color during formation due to
- blood group incompatibility
- K00.81 Change in tooth color during formation due to congenital
- biliary system defect
- K00.82 Change in tooth color during formation due to porphyria
- K00.83 Change in tooth color during the formation process due to use
- tetracycline
- K00.88 Other specified disorders of dental development
Here we will look at internal and acquired color changes, because... external ones can be easily removed by polishing.
Internal color changes. Systemic reasons.
Genetic defects:
Alkaptonuria is a hereditary disease caused by loss of functions of homogentisic acid oxidase and characterized by a disorder of tyrosine metabolism and excretion of large amounts of homogentisic acid in the urine. Often, patients with alkaptonuria develop pigmentation of the sclera and auricles, which is associated with the deposition of deposits of homogentisic acid in them. The intensity of such deposits may vary. These changes usually do not bother patients, but are one of the signs of this disease that have important diagnostic significance.
In the oral cavity, a bluish discoloration of the crowns of the teeth is observed on 1/2 crowns. There is increased dentin density with a yellow-brown change in the cervical half of the teeth.
Congenital erythropoietic porphyria develops with the birth of a child or in the first year of his life. Sometimes the initial signs of the disease can appear at the age of 3-4 years and older. The disease occurs equally in men and women. Red urine is the initial sign of the disease. Characterized by overdeveloped hair (hypertrichosis, thick eyebrows, long eyelashes), pinkish-brown staining of teeth (erythrodontia) due to the deposition of porphyrins in the enamel and dentin. When examined under ultraviolet rays, teeth give off a bright purple-red glow.
Congenital hyperbilirubinemia is a group of hereditary enzymopathies characterized by impaired bilirubin metabolism and manifested by persistent or intermittent jaundice in the absence of pronounced changes in the structure and function of the liver, obvious signs of hemolysis and cholestasis. An increased content of bilirubin in the blood leads to its accumulation and subsequent decay in the tissues of temporary teeth (mainly dentin), causing them to stain in various colors - yellow, greenish-blue, brown. Bilirubin can also influence histogenesis, leading to the development of systemic hypoplasia of primary teeth. The absence of hypoplasia with discolored crowns of primary teeth, which developed as a result of hemolytic jaundice, can be explained by the low titer of antibodies in the mother’s body and the treatment of the newborn with fractional blood transfusions. Over time, the intensity of tooth coloring gradually decreases, which is especially noticeable on the front teeth.
Amelogenesis imperfecta is a severe hereditary disorder of enamel formation, in which the structure and mineralization of both temporary and permanent teeth are disrupted, which leads to discoloration and partial or complete loss of tooth enamel, while dentin remains unchanged.
Amelogenesis imperfecta is divided into 4 main types:
- hypoplastic,
- hypomaturation,
- hypocalcified,
- hypomaturation-hypoplastic with taurodontism.
The hypoplastic form is characterized by insufficient formation of the protein matrix and a disorderly arrangement of enamel prisms. Clinically, it appears as thinned, rough enamel, ranging from smooth to roughly rough. The size of the crowns can vary from normal to small, without contact points between the teeth. The color varies from normal to light yellow-brown.
Hypomaturation forms of defective amelogenesis are clinically characterized by the presence of enamel covered with specks and having a brown-yellow color. The enamel is usually of normal thickness, but is softer than normal and tends to chip away from the dentin. In men, permanent teeth are mottled and yellow-white in color, but with age they may darken due to the adsorption of stains. The thickness of the enamel is approaching normal. The enamel is soft, and the tip of the probe can pierce its surface. Although these teeth are more prone to chipping and wear than healthy teeth, enamel loss occurs slowly. The appearance of baby teeth in boys resembles ground-in frosted white glass. Sometimes there is a slight yellowing of primary teeth. The surface of the teeth is relatively smooth. In women, alternating vertical stripes of dull white enamel and normal translucent enamel are visible on both primary and permanent teeth. These stripes come in different widths and are randomly distributed along the crown. There is no symmetry of homologous teeth on the right and left.
Hypocalcified amelogenesis is characterized by normal-thick enamel on newly erupted teeth. The enamel is soft and can be lost soon after eruption, leaving a crown composed only of dentin. The enamel has a caseous surface and can be scraped down to the dentin. As a consequence, open bite was recorded in more than 60% of observed cases. Hypocalcified amelogenesis is the most common type of enamel dysplasia, occurring in approximately one in 20,000 people (Witkop and Sauk, 1976). Large masses of supragingival calculus are observed and are often associated with severe gingivitis or periodontitis (Winter and Brook, 1975).
In the hypomaturation-hypoplastic form with taurodontism, teeth with an enlarged and elongated tooth cavity are observed, the thickness of the enamel is reduced with zones of hypomineralization and pits. Clinically, the molars have a taurodontic (“bull tooth”) shape, and the teeth may have white, yellow-brown spots and contact points may be absent.
Dentinogenesis imperfecta represents a group of hereditary changes that are characterized by pathological formation of dentin. These changes are genetically and clinically heterogeneous and may affect only the teeth or may be associated with osteogenesis imperfecta. With dentinogenesis imperfecta, only dentin is affected, but the enamel may also be somewhat thinner.
Dentinogenesis imperfecta is divided into 3 types: Type I (associated with osteogenesis imperfecta) is characterized by insufficient synthesis of type I collagen. As a result, the proper development and structure of bone tissue and dentin is disrupted. Bones become more fragile and brittle. The roots of the teeth are underdeveloped, the pulp chamber is greatly reduced by a factor of
Type II is not associated with osteogenesis imperfecta; there is a defect in sialophosphoprotein synthesis. No bone changes are observed; dental symptoms are similar to type I.
Type III has a large pulp chamber, very thin dentin, convex crowns, and reduced root structure.
Teeth with dentinogenesis imperfecta have a variety of colors ranging from yellow to blue-gray. Colors change depending on lighting and direction of light. They also show a high degree of translucency (similar to amber). Without proper support, enamel can break and chip. Once the dentin is exposed, the teeth quickly turn brown, presumably due to the absorption of chromogenic substances by the porous dentin.
Osteogenesis imperfecta is a group of genetic disorders that primarily affect the bones. In people with this pathology, the bones are very fragile and break easily, often from moderate trauma or for no obvious reason. In more mild cases, only a few fractures may occur during a person's lifetime. There is a blue or gray tint to the sclera of the eyes, and hearing loss may develop with age. Teeth, both temporary and permanent, are of normal size and regular shape. The color of dental crowns varies. It ranges from blue to blue-gray or yellowish-brown with a high degree of translucency. The same patient has different groups of teeth, as well as the same teeth have different degrees of staining. The second temporary and first permanent molars are lighter in color than the others. There is pathological abrasion of both temporary and permanent teeth. The degree of wear varies from child to child: primary teeth are worn to a greater extent than permanent teeth. The abrasion of hard tissues is more pronounced in incisors and first molars.
Discolorations caused by taking medications or high levels of trace elements in water and food: Tetracycline. The use of tetracycline group drugs in medical practice began in 1950, and the associated dental pathology (“tetracycline teeth”) was first described in 1956. The cause of this pathology is the use of tetracycline group drugs during the period of calcification of temporary or permanent teeth. This is due to the ability of tetracyclines to penetrate the placental barrier and be deposited in dentin and, to a lesser extent, in tooth enamel (the critical dose is believed to be 21-26 mg/kg and above). In this case, a tetracycline-calcium-orthophosphate complex is formed, which under the influence of ultraviolet rays acquires a darker color. This process occurs mainly on the vestibular surfaces of the front teeth, which are exposed to sunlight when smiling and talking. The color of the molars and oral surfaces of the front teeth remains virtually unchanged. The color of the teeth varies from yellow to brown and from gray to black tones.
There are 3 degrees of tetracycline staining:
I. Weak yellow, gray or brown staining, evenly distributed over the entire surface of the teeth, without streaks or concentration of staining in individual areas.
II. The coloring is darker or more saturated, yellow or gray, without streaking.
III. Pronounced dark gray or blue staining in the form of horizontal stripes on the surface of the teeth.
Teeth stained yellowish with tetracycline can fluoresce under the influence of ultraviolet rays. This property can be used for differential diagnosis with discolorations caused by other reasons. Depending on the dose, tetracycline can not only change the color of the enamel, but also lead to underdevelopment of tooth enamel (hypoplasia). It has been found that even fully formed permanent teeth in adults can change their color when taking tetracycline-minocycline. This occurs due to the deposition of the antibiotic in the tertiary dentin, as well as when it dissolves in saliva (Haywood, 2000)
It should also be noted that such staining is caused by minocycline, an antibiotic of the tetracycline group. Ciprofloxacin taken in childhood can cause a greenish discoloration of teeth.
Fluorosis is caused by excess fluoride entering the body during the formation of tooth enamel.
According to the WHO classification, the following forms of fluorosis are distinguished:
- A very mild form of fluorosis. The color of the tooth enamel is practically unchanged; there may be isolated spots.
- Mild form of fluorosis. Milky-white stripes or small spots are observed on the enamel of individual teeth. In this case, the affected area does not exceed 25% of the total area of the tooth crown.
- Moderate form of fluorosis. The affected area reaches 50%.
- In the medium form, along with chalky spots and stripes, brown or yellowish spots appear. If the above forms have high resistance to caries, then with an average degree the resistance decreases sharply.
- A severe form of fluorosis affects most of the tooth crown; in addition to pigmentation, disturbances in the structure of hard tissues are added. The crown becomes deformed and the enamel is subject to wear and chipping. Bone tissue may also be affected.
Internal color changes. Local reasons.
Discolorations associated with the pulp (hemorrhages, decay products, pulp necrosis, remains of pulp tissue after endodontic treatment, drugs used for the treatment and obturation of the root canal).
In case of injury or vibration during the preparation process, internal bleeding may develop. Blood cells penetrate the dentin, causing a pink discoloration. When a tooth is injured, compensatory formation of tertiary dentin may also occur, the tooth cavity decreases in size, the amount of dentin increases and the tooth acquires a more saturated yellowish tint.
With pulp necrosis after injury, an infectious process, or due to careless removal of pulp residues during endodontic treatment, decay products penetrate into the dentinal tubules, causing a persistent dark, gray, greenish coloration.
In the process of endodontic treatment , dentists use various preparations for treating root canals, sealers for their obturation, as well as means for pulp devitalization. All of these drugs can, in one way or another, change the color of the tooth by penetrating into the dentin from the cavity of the teeth.
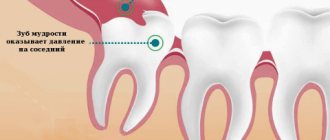
Tooth root resorption can be caused by various reasons - external or internal. Long-term inflammatory diseases of the pulp and apical periodontium of the tooth, pressure from unerupted teeth, tumors, trauma, excess pressure during orthodontic treatment, inflammatory processes in the periodontium are the main causes of tooth root resorption. The process is associated with excessive activity of osteoclasts. If root resorption is accompanied by pulp necrosis, then changes in tooth color will be corresponding. Sometimes, with internal resorption options, the tooth cavity increases, which will appear externally as a pink spot visible through the enamel.
Changing tooth color with age. With age, the tooth cavity decreases due to the formation of secondary dentin, and the thickness of the enamel decreases due to natural abrasion. At the same time, the intensity of the color increases, so with age the teeth become “darker”.
Acquired color changes.
Enamel hypoplasia develops due to amelogenesis deficiency. This may be due to an infection of baby teeth that affects anameloblasts, a lack of vitamin D during the maturation of the rudiments of permanent teeth, infectious diseases in childhood, gastrointestinal diseases, toxic dyspepsia, diseases of the endocrine system. Hypoplasia of primary teeth occurs as a result of disorders during pregnancy (toxicosis, rubella, toxoplasmosis, etc.). Hypoplasia can be systemic and limited, this is due to the influence of unfavorable factors during the formation of the rudiments of different groups of teeth at different times. According to the severity, hypoplasia can be:
- Weak degree - manifests itself in the form of spots, often white, less often yellowish in color, with clear boundaries and the same size on the teeth of the same name. Spots with hypoplasia are not stained with dyes.
- A more severe form manifests itself in the form of underdevelopment of enamel. On the surface of the enamel, depressions or grooves are found (wavy, dotted, grooved enamel). The enamel in the recesses remains dense and smooth.
- The most severe form is the complete absence of enamel in a certain area. There may be complaints of pain from thermal and chemical irritants.
Tooth wear and recession of the gum margin causes the formation of secondary dentin, which increases the color intensity of the tooth. The enamel also becomes thinner and in some areas is completely lost. These factors “make teeth darker.”
As you can see from this article, tooth discoloration can be caused by various reasons, and different options require different treatments. What to do in this or that case? Of course, consult a specialist! In the Alena network of clinics, you will be competently advised on this problem and will draw up an action plan for acquiring a snow-white smile.
Diagnostic measures
Diagnosis of dentinogenesis imperfecta involves both standard diagnostic dental procedures (examination of the oral cavity and radiography) and special ones, such as clinical and genealogical research aimed at identifying hereditary dental diseases and their characteristics.
With the help of an examination, the color and shape of the crown part, the presence of stains on it, and the degree of abrasion of the teeth are determined. In particular, the spherical shape of the crown may indicate imperfect dentinogenesis.
Based on radiographs, the condition of the root part of the tooth is determined (presence of canal obliteration, bone resorption) and the thickness of the walls of the pulp chamber.
When conducting a hereditary genealogical examination, a pedigree of family members is compiled (preferably no less than 3-4 generations) and the presence of genetically determined diseases of the jaw apparatus is determined.
The data obtained serve to clarify the diagnosis and make a prognosis for the offspring.
Characteristics of Pulposeptin paste and instructions for use in dentistry in the treatment of gangrenous pulpitis.
In this publication we will talk about the pathology called “Turner’s teeth”.
Here https://www.vash-dentist.ru/lechenie/zubyi/ultrazvuka-v-endodontii.html all about the benefits of ultrasonic expansion of the root canal of a tooth.
Reviews
Dentinogenesis imperfecta is a relatively rare, but in some of its forms, a serious disease that must be identified and treated without delay.
Moreover, in many families, due to the hereditary nature of the disease, it is not a surprise. If you or your children have been treated for dentinogenesis incomplete, please share your personal experience about this rather rare disease. You can leave a comment at the bottom of this page.
If you find an error, please select a piece of text and press Ctrl+Enter.
Tags: enamel destruction
Did you like the article? stay tuned
Previous article
The Korkhaus apparatus as the best solution in orthodontics for eliminating diastemas
Next article
Suturing the tooth socket is a simple and safe way to restore the alveolar process after extraction
Prevention
The percentage of the disease is higher among patients with acute osteogenesis, when there is a qualitative and quantitative collagen deficiency. Specific methods for preventing pathology have not yet been developed. For prevention purposes, you should carefully observe oral hygiene rules and undergo routine dental examinations. It is necessary to carry out sanitation of the oral cavity in a timely manner. It is necessary to visit the dentist at least once every six months in order to identify the disease in the early stages, as well as to begin treatment of the pathology in a timely manner. If necessary, consult a geneticist.