Periodontal disease is a fairly rare disease of non-inflammatory origin, characterized by systemic damage to the periodontal tissues (periodontium), which is often difficult to diagnose in the early stages. Its appearance, as a rule, is associated with a hereditary predisposition or systemic diseases of certain organs.
There is often an erroneous spelling of this term - periodontal disease. In order to dispel all doubts, let us turn to the etymology, which covers two words in ancient Greek: πᾰρά (para - “near, located near”) and ὀδόντος (odóntos is the genitive case of the word ὀδούς - odus, translated means “tooth”).
Consequently, from the ancient Greek language this term is translated as “near the tooth” or “located next to the tooth.”
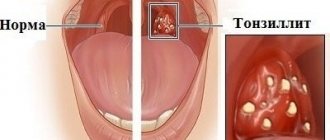
There are cases when even doctors mistakenly call periodontal disease a completely different disease - periodontitis, which is in fact a completely different phenomenon due not only to its inflammatory origin, but also to other features.
Diagnosis of periodontal disease
To identify signs of periodontal disease in adults, the following diagnostic procedures are usually performed:
- inspection;
- probing of the gingival sulcus;
- assessment of tooth mobility;
- X-ray examination (orthopantomography);
- biomicroscopy of the gums to determine the degree of microcirculation impairment.
The patient will also need observation from a general practitioner and endocrinologist to detect and treat general somatic pathology.
After a diagnosis of “dental disease periodontal disease” is made, further examination should be aimed at finding the causes of disturbances in the processes of cellular tissue nutrition, predicting the further development of the disease and the likelihood of inflammatory complications.
Diagnostics
Only an experienced dentist can diagnose periodontal disease, since at an early stage the symptoms are similar to those of other diseases, so it is extremely important to make a correct differential diagnosis from other diseases with similar symptoms.
When making a diagnosis, the doctor must examine the patient, carefully ask him about symptoms, well-being, and the presence of diseases, especially systemic problems with the endocrine system. You should also indicate the degree of development of periodontal disease, the depth of the gum pockets, the type of atrophy, and the degree of exposure of the necks of the teeth. All this will help to correctly identify the causes and prescribe treatment.
When diagnosing periodontal disease, a variety of functional diagnostic methods are used. With their help, it is possible to detect initial vascular changes, which makes it possible to make a diagnosis at an early stage.
- Using the modern method of rheoparodontography, it is possible to diagnose the early stage of development even in young people, when symptoms practically do not appear.
- Using the polarography method, it is possible to detect even a slight decrease in the level of oxygen in the gum tissue.
- It is impossible to make a correct diagnosis without modern X-ray examination. It is the radiograph that allows us to determine the degree of atrophy of the alveolar process, which allows us to correctly determine the stage of development.
- With periodontal disease, ROE increases, as there is constant intoxication of the entire body with decay products and vital activity of pathogenic microorganisms. The leukocyte count shifts to the left, the patient may complain of low-grade fever for a long time. Therefore, when making a diagnosis, it is also important to order a general blood test of the patient.
It should be noted that periodontal disease is a disease that lasts for years. And sometimes years pass from the appearance of the first symptom to a visit to the dentist. Therefore, doctors are often faced with advanced conditions of teeth and gums. With careful oral hygiene and following all the recommendations and instructions of the dentist, it is possible to keep teeth and gums healthy into old age.
Symptoms of dental periodontal disease
The main symptom of the disease is detected during x-ray diagnosis of periodontal disease. The image shows a uniform decrease in the height of the interdental septa with alternating foci of osteosclerosis and osteoporosis in the deep parts of the alveolar process and the body of the jaw, as well as in other bones of the skeleton. Traditionally, changes are accompanied by the presence of diseases of the cardiovascular or endocrine systems and metabolic disorders.
There are other symptoms of severe periodontal disease that are more noticeable to the patient and others:
- gum retraction;
- exposure of the necks and roots of the teeth;
- pale gum color;
- lesions of teeth of non-carious origin (wedge-shaped defects, hyperesthesia).
Symptoms
The first “bells” appear when diagnosing dental plaque, sensitivity of the gums, and too pale color of the oral mucosa.
Visually, the symptoms manifest themselves in a gradual decrease in the height of the gums, which occurs due to the progression of the sclerotic process and dystrophy. External inflammation may not appear, but the roots of the teeth are exposed, which indicates the development of the disease.
An examination by a dentist will help identify the initial stage of the disease.
Stages of periodontal disease
In modern dentistry, there are three degrees of severity of periodontal disease.
Mild degree
How does periodontal disease begin? In the early stages, the disease occurs without pronounced symptoms with gradual atrophy of the gum edge and bone tissue. With periodontal disease of the anterior teeth, a slight exposure of the dental necks occurs; in some cases, patients experience increased sensitivity of teeth to food irritants (hot and cold, sweet and sour). On X-ray images, the onset of periodontal disease is indicated by the first signs of bone tissue atrophy.
Average degree
With an exacerbation of periodontal disease, not only the necks, but also the roots of the teeth are exposed - by 2 - 3 millimeters. X-ray images show destruction of bone tissue along half the length of the root and the presence of foci of sclerosis.
Severe degree
With severe periodontal disease, exposure of the roots of the teeth reaches 4–5 millimeters, bone tissue atrophy on X-ray photographs covers two-thirds of the root.
Signs of periodontal disease
The disease has an asymptomatic period of development, the symptoms become pronounced after the transition to moderate severity, when the periodontal tissues become very thin. Visual detection of symptoms is complicated by the presence of tartar, which hides the necks of the teeth and does not allow assessing their condition. A diagnosis can only be made after professional cleaning by a dentist.
The number and severity of symptoms depend on the stage. Signs of the disease include:
- exposure of tooth roots;
- the appearance of a pale tint in the gum tissue;
- increased sensitivity of the patient’s teeth to cold and hot foods;
- darkening of tooth enamel;
- development of sclerotic changes in bone tissue;
- the appearance of gaps between teeth;
- discomfort and itching in the gum area;
- loss of stability, loosening of teeth.
Inflammation and bleeding of the gums during periodontal disease are rare and are present in advanced stages of the disease.
To make a diagnosis, the dentist prescribes an x-ray examination, which allows you to determine the presence of sclerosis of bone tissue, the degree of development of gum atrophy and identify foci of osteoporosis.
Periodontal disease – what to do?
At the initial stage of periodontal disease, you should consult a periodontist. No folk remedies will help get rid of the disease. Only a specialist will be able to carry out the necessary diagnostic procedures and prescribe, based on the identified symptoms of periodontal disease, treatment aimed at slowing down degeneration in periodontal tissues and preventing inflammatory complications. It is also necessary to eliminate non-carious dental lesions and undergo a thorough examination by a therapist to diagnose and treat common diseases that provoke the development of periodontal disease.
Complex therapy of periodontal disease involves the following measures:
- Timely removal of dental plaque.
- Normalization of occlusal relationships (grinding teeth, prosthetics, splinting).
- The use of vitamins and agents that improve microcirculation (nicotinic acid, aloe extract, heparin).
Is it possible to cure periodontal disease forever?
Treatment of the disease is carried out comprehensively with the involvement of specialists in the field of dentistry, immunology, endocrinology, gastroenterology, and therapy. The essence of treatment is to eliminate symptoms, strengthen teeth and prevent relapses. Additionally, restoration of lost tissue is carried out.
It is problematic to cure periodontal disease in the last stage, but contacting competent doctors will help get rid of unpleasant sensations and stop the further development of the disease, preserving your teeth.
Splinting
A treatment method used to strengthen loose teeth. Splinting involves combining individual teeth into a single orthopedic structure in the form of a block to reduce their mobility.
Prosthetics
Prosthetics for periodontal disease are carried out in combination with other treatment methods; it is possible to install several types of dentures, depending on the condition of the gums. Removable prosthetics helps reduce the load on areas affected by periodontal disease: installing clasp, nylon dentures that do not rub the mucous membranes and have a fastening system that does not damage the supporting teeth.
In some cases, permanent bridge structures are used to strengthen a number of teeth located one behind the other.
Prosthetics does not eliminate the cause of the disease. Without an integrated approach, tissue reduction will continue, and after 3-5 years the patient will need replacement prostheses.
Treatment methods
Methods and procedures used to treat periodontal disease in dentistry:
- exposure to high pressure oxygen in hyperbaric chambers;
- electrophoresis;
- diadynamic currents;
- amplipulse therapy;
- darsonvalization of gums;
- UHF therapy;
- gum massage;
- local hypo- and hyperthermia;
- ultrasound therapy.
Psychosomatics of periodontal disease
Based on the results of many years of research, American scientists have come to the conclusion that dental diseases such as periodontal disease are directly related to high anxiety, depression and an acute sense of loneliness. This is explained by the fact that increased levels of the stress hormone - cortisol - in the blood negatively affect the condition of the gums and jaw bones. In addition, during periods of nervous tension, people begin to pay less attention to oral hygiene and increase the doses of alcoholic beverages, nicotine and medications, which also contributes to the development of various diseases.
Treatment
The treatment procedure depends on the stage of the disease and includes the following steps:
- Diagnostics at the dentist, making a diagnosis and taking an x-ray of the jaw;
- In-office dental cleaning to remove hard deposits, antibacterial therapy of the oral cavity;
- Orthopedic treatment of loose teeth to strengthen them. Splinting and prosthetic techniques are used to reduce the load on damaged teeth;
- Physiotherapeutic treatment - procedures to restore blood circulation to the gums and prevent relapses of the disease;
- Gum tissue augmentation is carried out when the necks of the teeth are severely exposed.
Self-treatment is impossible. Home remedies are not able to get rid of the causes of the disease. If you notice the first symptoms, contact your dentist.
Consequences of periodontal disease - why is it dangerous?
- Firstly, due to the absence of pronounced symptoms, this disease can progress unnoticed over many years and lead to total destruction of the teeth and jawbone - and then teeth fall out with periodontal disease.
- Secondly, the destruction of bone tissue leads to disturbances in the functioning of the gastrointestinal tract with the subsequent occurrence of diseases of the digestive system.
- Thirdly, advanced periodontal disease can provoke periodontitis - acute inflammation of the tissue and tooth loss.
In addition to the above consequences, generalized periodontal disease in an advanced stage causes another dangerous disease - osteomyelitis, that is, purulent bone damage.
Prevention
Doctors always warn: prevention is much more effective than subsequent treatment. Therefore, it is much more important to prevent the development of periodontal disease, because treatment can last a very, very long time.
The main preventive measures include careful oral hygiene. It is necessary to thoroughly brush your teeth twice a day with a special toothpaste, and also use rinses that help strengthen your gums and protect them from inflammation. It is also necessary to adhere to the principles of a healthy diet and limit the consumption of sweets.
Periodontal disease - contagious or not?
To the questions “Is periodontal disease contagious?” or “Is periodontal disease transmitted by airborne droplets?” Doctors answer unequivocally in the negative. Therefore, you should not believe various dubious articles on the Internet about how periodontal disease is transmitted. The disease is associated with metabolic disorders, and not with the spread of bacteria. Therefore, those who believe that periodontal disease can be contracted or that the disease is transmitted through a kiss are deeply mistaken. However, despite this, we must not forget about the rules of daily oral hygiene in order to prevent the occurrence of other problems with teeth and gums.
How does periodontal disease occur?
Periodontal disease is a systemic disease of the periodontal tissue, or periodontium. Refers to inflammatory gum diseases.
The causes of periodontal disease are pathogenic microbes living in dental plaque, under the influence of which inflammation occurs. That is, in fact, the main reason for the occurrence is insufficient oral hygiene and the constant presence of dental plaque.
Periodontal disease at the initial stage is confused with gingivitis or periodontitis.
The insidiousness of the disease is that the patient does not even suspect its presence for a long time. The gums become sensitive and begin to bleed, but all these symptoms develop over a long period of time and gradually, so from the moment of onset until the moment when the patient begins to understand that there is something wrong with the gums, time passes and the favorable moment for treatment is missed.
If periodontal disease treatment is not started in time, a periodontal pocket forms at the root of the tooth, in which pathogenic bacteria multiply and cause destruction and resorption of the root.
Periodontal disease treatment
The treatment process must be comprehensive, under the supervision of a specialist.
Treatment methods include:
- use of UHF therapy, electrophoresis;
- gum massage and cleaning from plaque and stone, timely treatment of caries;
- timely removal of dead tissue;
- To reduce mobility, teeth splinting is used;
- in case of severe damage, the tooth is removed and prosthetics are prescribed;
- medication course: drugs that accelerate the regeneration of affected tissues, anti-inflammatory, multivitamin complexes.
How to treat gum periodontal disease
The treatment process is lengthy, and the individuality of the body, as well as all concomitant and chronic diseases, should be taken into account.
It is important to quit smoking, maintain oral hygiene, and eat a balanced diet. The specialist prescribes a comprehensive treatment regimen, depending on the stage of development of the disease. Drug treatment together with physiotherapy can stop the development of periodontal disease.
Oral care for periodontal disease
Oral hygiene is very important; timely brushing of teeth not only helps to destroy pathogenic bacteria, but also massages the gums, which increases blood circulation. You should pay attention to the stiffness of the brush and timely replacement, at least once every three months.
It is useful to use irrigators, which serve to wash hard-to-reach areas and gently remove food debris.
Periodontal disease is a dangerous disease that requires long-term treatment, constant monitoring by a specialist and comprehensive treatment.
Periodontal disease is...
According to the terminology of the Great Medical Encyclopedia, periodontal disease is a lesion of the periodontium of a dystrophic nature (periodontium is a complex of tissues surrounding the tooth and holding it in the alveolus, having a common origin and function).
Periodontal dystrophy is premature atrophy of the dental alveoli, characterized by progressive resorption of their bone tissue, leading to the formation of pathological periodontal pockets, suppuration from them, loosening of teeth and, often, the occurrence of alveolar abscesses. Let's bring some clarity to medical terminology. Dystrophy is the basis of the process, a violation of the complex of mechanisms (trophism) that ensure the metabolism (metabolic processes) of cells and intercellular substances and the preservation of their structure, as a result of which the function of the organ changes.
Bone resorption - in pathology - resorption of necrotic masses and reabsorption (absorption) of substances into blood or lymphatic vessels.
Alveolar abscess - formed on the alveolar process of the jaw as a result of apical purulent inflammation of the root periosteum of the tooth. The pus, which initially accumulates at the apex of the root, infects the cell and causes inflammation of the bone marrow of its walls.
Misconception or fact
Many people have heard that periodontal disease is contagious. Usually, the person who claims this says that he or someone he knows contracted this disease from other people.
Are these opinions a misconception or a fact? Is periodontal disease contagious or not, is it transmitted by airborne droplets, contact, fecal-oral, vector-borne (through the bites of blood-sucking insects) or other known routes of oral infection transmission? The essence and causes of the origin of this disease will help us answer these questions.
The origin of the disease is not influenced by microorganisms
Oral thrush, one of the most common forms of thrush, is a fungal infection caused by the yeast Candida that affects the mucous membranes of the mouth.
Candida is a genus of yeast. There are about 150 different species of Candida that can cause serious yeast infections. The most common cause of thrush is Candida albicans.
Typically, infectious fungi are a natural component of the skin, oral cavity, and intestinal flora. They do not cause discomfort as long as their reproduction is limited by the balance of other microorganisms and the immune system. Problems only arise when fungi overgrow or break through the natural barriers of the skin and mucous membranes, causing thrush.
Candidiasis is the common term for infections caused by this fungus. Therefore, oral thrush is called oral candidiasis or candidal stomatitis. Fungal infections traditionally occur in the mouth and areas close to the throat. Children are more often susceptible to the disease, but the infection can also occur in adults with weak immune systems.
Forms of candidiasis in the mouth
Typically, mouth fungus develops on the inside of the cheeks or lips. But the throat, tongue or palate may also be affected.
Thrush can change from one form to another, or occur independently.
Types of thrush in the mouth and their signs:
- pseudomembranous candidiasis: white, cheesy, easily removable plaque on the reddened, inflamed mucous membrane
- acute erythematous candidiasis: burning sensation on the tongue, severe redness of the mucous membrane without deposits
- hyperplastic candidiasis: dense gray-white plaque, the oral mucosa is hyperemic
Pseudomembranous candidiasis in the mouth
- classic thrush. In the most common form of oral thrush, pseudomembranous candidiasis, isolated white speckles form in the mouth and are easily removed.
After scraping, the oral mucosa appears shiny, dry and red. As a fungal infection progresses, increasingly large white creamy spots appear, which, when detached, lead to bleeding of the mucous membrane. If left untreated, thrush in the mouth can spread to the throat, esophagus, or gastrointestinal tract.
Other symptoms of oral thrush
In addition to the described plaque and redness of the mucous membrane, late-stage oral thrush causes additional symptoms. These include:
- burning and dry mouth
- increased thirst
- bad breath
- metallic taste in mouth
- swollen lymph nodes
- difficulty swallowing
- pain while eating or drinking
- thrush in the mouth in children is in most cases accompanied by fever
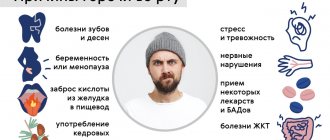
Causes of periodontal disease
The main reasons that lead to the appearance of periodontal disease:
- disruption of the endocrine system;
- bone tissue injuries;
- lack of vitamins, in particular vitamin C;
- problems with the gastrointestinal tract, cardiovascular system;
- smoking, alcohol abuse;
- hereditary factor;
- the presence of malocclusion (chronic injuries to the mucous membrane);
- taking anticonvulsants;
- the presence of chronic diseases, including diabetes mellitus, hypertension, dystrophic neurogenic processes, atherosclerosis, hypoxia;
- physical inactivity;
- impaired blood circulation in tissues;
- improper dental care.
The exact list of causes of periodontal disease has not been fully established. Much depends on heredity, the functioning of the cardiovascular and endocrine systems, and the presence of diseases of internal organs.
It is impossible to become infected with periodontal disease, since this disease is not caused by viruses or microbes. Bed linen, dishes, cutlery, and kisses cannot cause disease transmission. But personal hygiene should still be given maximum attention, since one of the reasons for the development of lesions is precisely damage to the mucous membrane of the gums and bone tissue.
Prevention of periodontal disease and periodontitis
Preventive measures include the following:
- periodic professional cleaning of tooth enamel from plaque and tartar;
- ensuring the body receives essential vitamins and minerals, in particular calcium and vitamin D3;
- routine visits to the dentist for oral hygiene;
- eradication of bad habits;
- from early childhood, taking care of enamel and the formation of a correct bite;
- include solid, healthy foods in your diet - raw carrots, apples, which improve blood circulation and strengthen gums;
- learn oral care skills.
The answer to the question of whether it is possible to become infected with periodontal disease is negative. However, there is always a risk of developing periodontitis, gingivitis and stomatitis.
Bibliography
- Barer G.M. – Periodontal diseases. Textbook, M.: GEOTAR-Media, 2008.
- Borovsky E.V. – Therapeutic dentistry. Textbook, MIA 2003.
- Dmitrieva L.A. — Modern aspects of clinical periodontology, M., 2001.
- Loginova N.K., Volozhin A.I. — Pathophysiology of periodontal disease (methodological manual), M., Medicine, 1993.
- Tsepov L.M., Kamanin E.I., Morozov V.G. — Periodontitis: intercellular, intertissue, intersystem interactions and clinical relationships, Smolensk, 1992.
- Gaurav, Solanki and Renu Solanki - Dental Plaque Forming Bacteria's Characterization and Stress Responses - M.: LAP Lambert Academic Publishing, 2012.
- Ijndhe J. - Textbook of Clinical Periodontology. 1995. Copenhagen.
- Kuzmina E.M. – Prevention of dental diseases, M.: 2003.
- Grudyanov A.I. — Antimicrobial and anti-inflammatory therapy in periodontology, M., 2004.
Find a clinic
Signs of disease development
In the early stages, periodontal disease is usually asymptomatic in humans. It is accompanied only by a slight change in the color of the gums. Painful sensations and any other manifestations are not inherent in it, which is why patients in the first months of the development of the pathology do not pay attention to it and do not come to the doctor in a timely manner.
As a rule, the disease makes itself felt only 3-5 years after the onset of the pathological process.
In the later stages, the development of periodontal disease in a person can be recognized by a number of characteristic symptoms. These include:
- Change in gum color. With periodontal disease they become pale. Inflammatory processes, suppuration, and bleeding are rarely observed with this disease.
- Reduction of alveolar processes in size. This symptom leads to exposure of the neck of the tooth. At the same time, the teeth themselves do not become loose and remain firmly in place.
- Itching that periodically occurs on the gums.
- Minimum amount of plaque and tartar on the teeth. In some cases, they may be completely absent in patients.
Also, with periodontal disease, a person may experience non-carious lesions of tooth tissue. These include abrasion of enamel, erosion, and wedge-shaped defect. Such pathologies require additional diagnostics and usually indicate the presence of concomitant diseases in the body, including pathologies of metabolic processes.
In the later stages of the disease, the patient may experience inflammation of the gums, tooth loss and the formation of ulcers. As a rule, at least 15-20 years pass between the onset of pathology and this stage.
Pain due to periodontal disease
With periodontal disease, patients may experience pain. The reason for its appearance is the exposure of the necks of the teeth. Because of this, their sensitivity to cold and hot foods increases. When contacting such products, an acute short-term pain usually appears, which disappears after the end of exposure to the irritant on the neck of the tooth.
With periodontal disease, patients do not have gum pain. If this symptom is present, there may be some additional damage (for example, cuts to the gums) or other diseases that complicate the underlying disease. If such symptoms appear, you should consult a doctor for additional advice.
Types of periodontal disease
Depending on the nature of the disease, periodontal disease is divided into types:
- acute stage;
- chronic course.
This division is not clear in its classification, since classic external manifestations are often not observed. During the acute stage, the process occurs quickly over several years.
By area of the oral cavity affected:
- localized stage, in which the affected area includes several teeth;
- generalized lesion involving the entire upper or lower jaw, or both.
According to the stage of the disease:
- initial, when changes in tissues are noticeable only during special diagnostics;
- the first, in which there is slight receding of the gums;
- the second stage, characterized by exposure of the necks of the teeth, the appearance of interdental spaces;
- third - if the gums are lost by more than 50%, loosening of the teeth and discomfort during the chewing process is possible;
- the extreme stage, the fourth, causes the greatest discomfort, eating becomes problematic, and the teeth are extremely loose.