All caring parents carefully monitor the health of their baby, so any irritation on the child’s face or body can cause severe anxiety. A callus on the lip of a newborn is an unpleasant, but not dangerous, phenomenon. Knowing what factors lead to injury to delicate skin, you can minimize the risk of formation.
Varieties and causes of occurrence
A callus on the upper lip of a baby is a patch of keratinized skin that appears due to strong friction. This is how the body protects the deep layers of the epidermis from damage.
There are several types of formations:
- dry - a hard crust consisting of dead particles of the epidermis;
- wet - under the rubbed layer of skin there is a bubble filled with lymphatic fluid;
- bloody - there is an admixture of blood in the fluid of the callus.
Dry calluses can most often be seen on the lips of infants. Delicate skin is damaged due to the following factors:
- rough tip of the nipple during artificial feeding;
- long and frequent friction on the nipple in the absence of a feeding regimen;
- improper latching of the breast by the child;
- features of the anatomical structure of the mammary gland;
- difficulty releasing milk.
Usually, a milk callus on a baby’s lip appears 2-3 weeks after the birth of the child and does not bring him significant discomfort. If the skin has become rough as a result of active sucking, such a neoplasm does not require special treatment. After a few days, the hardened crust will fall off, leaving no scars. In some cases, the skin finally heals only after the introduction of complementary foods, when the pressure on the lip is reduced.
Regardless of the reason that caused the appearance of a callus, it is forbidden to rip it off or pierce it . Such actions can lead to the entry of pathogenic bacteria into the wound. It is also not recommended to lubricate the formation with alcohol-based antiseptics, including iodine and brilliant green. The use of various traditional medicines can cause an acute allergic reaction, including suffocation.
If the blister opens on its own or is accidentally touched while swimming, it is necessary to lubricate the damaged area with hydrogen peroxide, Miramistin or an aqueous solution of Chlorhexidine. After this, the wound will dry out within 2 hours.
Cleft lip - symptoms and treatment
A multidisciplinary team is involved in the treatment of patients with clefts, since even a well-performed operation does not guarantee the absence of other complaints. Team members: pediatrician, dentist, orthodontist, plastic or maxillofacial surgeon, nutritionist, speech therapist, ENT, ophthalmologist and neuropsychiatrist. The ENT doctor works to prevent concomitant pathology of the middle ear, which often develops with clefts, and, if present, treats it. Orthodontists make orthodontic structures (obturators), thanks to which the child can eat normally. Obturators are prosthetic devices that close a cleft and can be used for children of all age groups.
Dentists Hubener D.V. and Liu J.R. classified means for orthopedic treatment of the cleft into preoperative and postoperative, active and passive, extraoral and intraoral [14]. There was a long debate about how these methods affect the growth of facial bones and whether they worsen the prognosis, until naso-alveolar plates were invented, which were made first of acrylic, then of rubber. The plates closed the cleft, and the child could suck normally; in addition, the pressure of the plate helped support the wings of the deformed nose, improved the ratio of the lengths of the columella, the cleft parts of the lip, and gently moved the triangular bone [11].
Many types of surgical treatment have been described for the treatment of cleft lip and palate, although the possibility of performing such operations has arisen relatively recently.
Since early times, people have tried to find a way to get rid of this defect. They tried to connect the crevice with sharp sticks, then they used metal needles that were wrapped with thread. Due to the lack of means for pain relief, the operations were primitive and ineffective. Since the 16th century, they have tried to use special caps for external impact on the cleft, trying to cause the edges to stick together. The protruded premaxillary bone in the case of bilateral clefts was simply cut off, which most often led to worsening deformation of the midface.
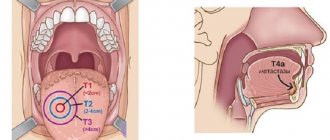
Surgery to correct a cleft lip is called cheiloplasty . With the beginning of surgical corrections, cheiloplasty methods began to change and improve. The first operations were perceived as a miracle; they created a linear incision. Over time, they began to make incisions of increasingly complex configurations in order to correct associated deformities and prevent the appearance of new ones. Now, in order to correct the complex deformity that occurs in the midface area and create conditions for the normal development of the facial part of the skull, it is necessary that the operation fulfill the following conditions:
- Was safe for young children.
- I corrected the maximum in each specific case in 1 stage.
- Formed the correct line of the red border and Cupid's bow.
- Correct formation of the filtrum is desirable.
- Provided sufficient depth of the vestibule of the oral cavity.
- It eliminated improper attachment of the fibers of the orbicularis oris muscle and created a continuous layer of muscle, which will help in the correct formation of the bones of the facial skull.
- Lengthened the short medial part of the cleft lip.
- Corrected the shape and position of the nasal cartilage.
In 1938 A.A. Limberg described and in 1952 expanded the method of unilateral cheiloplasty. This method became the leading method in the USSR for a long time, because in most cases it made it possible to correct the concomitant deformation of the nasal wing on the cleft side.
In 1952, Tennyson C.W. in the USA and in 1955 Obukhova L.M. in the USSR they described a cheiloplasty method of a more complex configuration. The method is still used today; in addition, cheilorhinoplasties have been developed on its basis to reduce the likelihood of developing associated deformities. The techniques are interesting primarily for their historical significance: for the first time, complex-shaped incisions began to be made and the lip was lengthened. However, lengthening the lip on the cleft side was also a limiting factor because it itself created a recognizable deformity. Techniques are now being used to solve this problem.
The most used technique for suturing unilateral clefts in the world now is the Millard technique and its modifications. In our country this is a modification of I.A. Kozina.
Millard cheiloplasty involves simultaneous restoration of the continuity of the upper lip and correction of the nasal cartilage. On the medial fragment of the upper lip, point 1 is marked - the center of the cupid's bow. On the healthy half of Cupid's bow, look for limiting point 2 (apex of the arc), located approximately 2-4 mm from the midline. This distance is laid on a white roller on the shortened side, obtaining point 3. The length of the lateral fragment of the lip on the healthy side is measured between the limiting point 2 and the commissure of the mouth (point 6). The resulting distance (approximately 20 mm) is laid on a white roller on the damaged side of the commissure (point 7) and a limiting point 8 is obtained. Point 8 will be the top of the cupid's bow on this side; it should connect to point 3 on the medial segment. Measure the distance from point 2 to the base of the nasal wing of the healthy side (point 4), the same distance is set aside from point 8 to the base of the nasal wing of the affected side (point 10). On the shortened side, from the middle of the base of the columella (point 5) to point 3, an arcuate rotational incision is made, symmetrical to the arc of the philtrum on the healthy side. If necessary, extend the incision to point x (reverse incision towards the healthy philtrum). On the lateral (side) fragment, according to the length of the section x-5-3, point 9 is found medially from the base of the flattened wing of the nose. Modifications are mainly used to expand the intervention to the nose, with secondary cheiloplasty, hidden and incomplete clefts.
The advantages of this method of primary cheiloplasty:
- maximum tissue preservation;
- moving all elements of the upper lip to the correct position;
- formation of the bottom of the vestibule of the nasal cavity and the deep vestibule of the mouth.
The method simultaneously corrects the position of the deformed wing of the nose, and some modifications are supplemented with one-stage rhinoplasty. In addition, the arcuate scar is hardly noticeable and can be used for corrective cheiloplasty in adulthood.
Closure of a bilateral cleft can be one-stage or two-stage. This depends on the volume of the cleft, the experience and confidence of the surgeon in his techniques. Each option has its pros and cons, but it is believed that with the help of one-step closure of the cleft, it is more likely to fully create a sphincter of the orbicularis oris muscle.
Sometimes it is practiced to connect the edges of the cleft. This is not a full-fledged cheiloplasty, but only the transfer of a complete cleft into an incomplete one in the expectation that the pressure of the connected part of the lip will have an orthopedic effect on the edges of the cleft, which will lead to their convergence. In most Western countries, the Millard method of cheiloplasty remains the leading one [12].
With a two-stage closure, one side of the cleft is first closed using any method, and after some time the other side is closed.
The debate about at what age to perform surgery still continues to this day. There are those who urge treatment to be carried out as early as possible. Even operations on the fetus are offered, due to the lack of scarring in the prenatal period. Many insist on surgery in the first days and even hours of life. On the one hand, there are advantages to this (parents are not afraid of the child’s appearance, there are no intra-family conflicts, there are no problems with nutrition), but there are also disadvantages (imperfect thermoregulation of newborns, high sensitivity to blood loss, very small anatomical basis). In the 60s of the last century, a large-scale analysis of the results of operations performed in the maternity hospital in the first days of life was carried out. The result showed in almost all children much worse results than in patients who were operated on as adults [1]. N.M. Mikhelson, in one of the oldest Russian manuals on plastic surgery, advises performing the operation at the age of 5-6 months, when the child is sufficiently strong and developed. He believed that cosmetic success was easier to achieve during this period. It is also described that such operations should be performed under local anesthesia, due to the danger of anesthesia [10]. Now there are safe drugs for anesthesia, so it is difficult to imagine performing an operation on young children under local anesthesia. Most surgeons believe that primary cheiloplasty is indicated at the age of 6-12 months.
The extent of the operation depends on the degree of the cleft. Many modern authors believe that in case of a complete cleft, primary cheiloplasty (when only the cleft is sutured) should be used in exceptional cases, since it does not correct the condition of the nose. Therefore, now the primary rhinocheiloplasty technique should be used, when, together with suturing the cleft, the position of the alar cartilages, septum, and vomer is corrected. The quality of the primary operation should be maximum, since repeated corrections are more difficult to perform in conditions of soft tissue deficiency and extensive scarring [4].
Complications during surgery
When performing surgery, the danger is aspiration (inhalation by the patient) of blood and mucus, which can cause asphyxia. To prevent this, you should prevent bleeding and carefully suck out the contents of the oral cavity (blood, saliva, mucus). Possible complications also include collapse, shock, laryngospasm and other conditions.
Mortality on the operating table and shortly after surgery is usually associated with improper selection of patients. You cannot operate on malnourished and premature children, those who, even before surgery, suffer from inflammatory conditions of the respiratory system, hearing, and decompensated abnormalities in the development of the brain, heart, and blood vessels. Also, surgery is prohibited in the presence of thymic-lymphatic status (enlarged thymus). The possibility of surgery should be decided together with the pediatrician.
Complications after surgery
In the coming days after surgery, stenosis (narrowing) of the larynx, bronchitis, pneumonia, urinary retention and other somatic complications may occur, the prevention and treatment of which should be carried out with the participation of a pediatrician. The most common local early complication is suture dehiscence, which is usually associated with technical errors in the operation:
- excision of a significant amount of tissue in the area of the edges of the cleft;
- insufficient tissue preparation;
- incorrect layer-by-layer suturing of the wound;
- tissue tension in the wound area, inflammation and swelling in the operation area.
Sometimes the sutures come apart due to injury (a child’s fall, an accidental blow to a hard object), infection, or the child’s illness with ARVI, rhinitis and other inflammatory pathologies. If the sutures diverge, the issue of applying secondary sutures is decided according to the patient’s condition.
When examining a patient who has undergone surgery, the height of the upper lip, the degree of its deformation, the depth of the vestibule of the mouth and its tightness (the presence of oronasal anastomoses and palate defects) are checked. You should pay attention to lip mobility, phonation, and changes in the structure of the dental system. The integrity of the orbicularis oris muscle can be tested by having the patient stretch his lips into a smile and purse his lips into a tube [1].
Severe psychological trauma is caused by scar changes after an unsuccessful first operation. One of the most unpleasant long-term complications of cheilorhinoplasty is deformation of the upper lip, nose and upper jaw, which can occur for various reasons [9].
After surgery, the patient may have a lack of soft tissue of the upper lip, its lengthening or shortening, stiffness due to extensive scarring, or an aesthetic defect. Alveolar cleft leads to the formation of crowding of teeth, the growth of dystopic (improperly positioned) and supernumerary (extra) teeth, which can support inflammation or, due to their location, form an oronasal fistula (an opening between the oral cavity and the nasal cavity). In general, such a fistula can also be due to excessive tension, cutting sutures, a defect in suturing, etc. Through it, the discharge of liquid part of food into the nasal cavity can persist, which in turn helps to maintain chronic rhinitis, sinusitis, etc.
Possible insufficiency of the muscle ring of the orbicularis oris muscle, which develops with defects in muscle alignment or insufficient separation of muscle fibers from the pyriform opening. Deformation of the vestibule of the mouth in the form of its flattening complicates further orthodontic treatment, which is so necessary for patients, and aggravates the retrusion of the midface (backward displacement). Deformations of the external nose and septum lead to a significant deterioration in the aesthetic result and disruption of nasal breathing, and breathing through the mouth in such patients aggravates the deformation of the facial skeleton.
Symptoms of rashes
A milk blister on the lip of a newborn can be confused with pathological rashes that require special treatment. The formation, associated with the way the baby feeds, looks like a small white or yellowish bead, reaching 0.5 cm in diameter and located in the center of the upper lip. The edging of the affected area merges with the skin.
The inflammatory element resulting from the entry of infectious agents into the body may have a gray, yellow or white color. The baby's oral cavity should be examined. The presence of plaque, blisters or ulcers in it indicates the presence of pathogenic bacteria. You should be alert if you notice the following symptoms:
- frequent regurgitation and gagging;
- problems with stool, changes in the smell, color and consistency of stool;
- apathy, tearfulness for no reason;
- refusal of food, malnutrition;
- a repulsive odor emanates from the mouth caused by the activity of pathogenic bacteria;
- high body temperature, sweating;
- redness of the skin, appearance of a rash;
- there are similar formations on the oral mucosa;
- increased salivation.
Symptoms
- Fever, fatigue, muscle pain, irritability.
- Pain, burning, tingling and itching (at the site of future infection rashes).
- Formation of sores in the mouth: on the gums, the front of the tongue, the inside of the cheeks, the throat and the roof of the mouth.
- Enlarged lymph nodes.
- Damage to the mucous membrane of the throat with the formation of small ulcers and a grayish coating on the tonsils.
- Lack of appetite.
For the diagnosis of herpes infection, cytological, immunofluorescent, serological and PCR methods are valuable. The material for testing for herpes is blood, throat swabs, the contents of blisters, ulcers, and urine.
Preventive measures
The likelihood of a callus forming on the upper lip of a newborn can be reduced by following feeding rules . You must adhere to the following recommendations:
- If the baby falls asleep while sucking, you need to take him off the breast by gently pressing his chin and put him in his crib.
- With good lactation, a feeding session should not last more than 20 minutes. To normalize milk flow, you need to drink more liquid. 10-15 minutes before feeding the baby, you should drink a glass of warm fruit compote, rosehip decoction or weak tea with milk.
- The baby should grasp not only the nipple, but also the areola with his mouth. To do this, you need to hold the baby so that his face is at the level of the breast. If the grip is incorrect, the position of the chest should be corrected.
- If there are no problems with lactation, pediatricians recommend breastfeeding babies for at least six months so that their delicate skin is not damaged. If your lips are rubbed with a pacifier, you need to make sure that its hole is not clogged with lumps of the mixture. The softest attachments are made of latex and silicone.
- With artificial feeding, the risk of overfeeding the baby is increased. It is impossible to feed a child with formula milk in unlimited quantities, not only because of the risk of callus formation, but also because the finished powder is saturated with vitamin supplements and vegetable fats, which must be supplied to the child’s body in a volume appropriate to his age and body weight.