Chronic pancreatitis is an inflammation of the pancreas that occurs over a long period of time with periodic exacerbations. Often this pathology is a consequence of the development of disturbances in the outflow of digestive fluid and other enzymes that are synthesized by the pancreas.
The disease poses a considerable danger to any person, as it can even cause death; as a result, it is important for every patient diagnosed with chronic pancreatitis to become familiar with the disease in more detail.
Today’s article on our resource will be an excellent help in this, because it examines a typical example of the history of this disease from the cases of a practicing gastroenterologist. Interested? Scroll below.
Medical history
Abdominal discomfort may be a sign of pancreatitis.
According to the patient, P.S. Klapovnikov, the disease appeared about 7 days ago. The first unpleasant manifestations of the disease appeared during meals.
There was no discomfort for several days. But within a day and directly on the day of admission to the clinic, the symptoms appeared again.
Life of a patient
There are no developmental problems. He ate 4-5 times a day and has no special food preferences. He was not seen by specialized specialists in the clinic.
The last time he was hospitalized was in 2006 due to acute appendicitis. The body systems function stably, there are no chronic ailments. The patient was completely healthy at the time of the last examination (March 1, 2016).
Experience in using hydroxyapatite-coated implants for immediate dental implantation
A.Yu. Drobyshev. Moscow State Medical and Dental University. Department of Hospital Surgical Dentistry and Maxillofacial Surgery (Head of the Department - Professor V.S. Agapov)
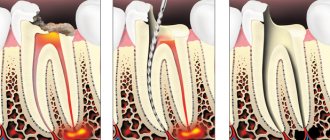
Instant replacement of a lost or removed organ and restoration of its function is the constant desire of every doctor. Dentists were among the first to use reimplantation of their own teeth and transplantation of them from other people and animals. With the emergence and development of dental implantology, this task seemed to have become simple, however, to this day, many practitioners are wary of the idea of installing an implant in the socket of an extracted tooth. As a rule, implants are placed 3-6 months after tooth extraction. The clinical experience we have currently accumulated and the results of experimental studies allow us to consider immediate implantation an effective method. A feature of immediate implantation is a more pronounced inflammatory reaction in the early postoperative period compared to delayed implantation. The undoubted advantages are: the ability to preserve the parameters of the alveolar process and interalveolar height; reducing the time from tooth extraction to prosthetics and wearing a temporary fixed prosthetic structure, which simplifies obtaining the patient’s consent for tooth extraction and implantation. The planning of the operation is facilitated by changing the diameter of the root in the gingival area and its length. An important factor is the ability to install implants exactly along the axis of the tooth, which creates optimal load distribution on the implant. A good aesthetic result is achieved - the papillary gingival contour is preserved. One of the problems faced by practicing doctors is the technical difficulties that lie in the absence of large-diameter implants in most domestic systems - 5 and 6 mm. The doctor performing implantation must have skills in working with bone replacement drugs, membranes, and know the basics of targeted tissue regeneration, since often, after installing an implant, the surgeon is faced with the problem of closing various bone and mucous defects. We consider the presence of an acute or chronic inflammatory process or tumor in the surgical area to be local contraindications for immediate implantation. In this case, general contraindications for implantation are taken into account. In order to achieve success, the following principles must be observed: - implants with a diameter of 4, 5 and 6 mm are required; — the optimal shape of the implant is root-shaped and mushroom-shaped; — the length of the implant must be longer than the root of the extracted tooth; — the implant must have primary stability, which is achieved by intercortical fixation and placement of the implant in freshly treated bone; — the hole after tooth extraction must be sanitized, the voids filled with bone replacement material. Immediate dental implantation was carried out in 48 patients diagnosed with chronic periodontitis, who received 87 dental implants with plasma sprayed hydroxyapatite, Konmet, Steri oss. Among the patients there were 37 women and 11 men, from 20 to 48 years old. 47 implants were installed after the removal of single-rooted teeth, 40 implants after the removal of many root teeth. If the operation was planned in advance, then 4-5 hours before the operation the patient began taking a broad-spectrum antibiotic (we used antibiotics - Augmentin, amoxiclav 375 mgm three times a day). The patient was given premedication before the operation. Under local anesthesia with ultracaine, the tooth or tooth roots were carefully removed so as not to damage the walls of the alvola; after careful curettage, the socket was examined for the presence of a defect in the bone wall. The root socket into which the implant was not inserted and the bone defects of the socket were filled with Kolapol KP-3. Then, trying to maintain the direction along the axis of the tooth, the implant bed was formed using a milling cutter of the appropriate diameter, going beyond the walls of the alveolus so that the implant was fixed in the freshly processed bone. The thread was cut and an implant of the appropriate diameter was inserted. At the beginning of our work, before extracting a tooth and installing an implant, we always peeled off a trapezoidal flap from the vestibular side in order to suture the mucous membrane over the implant, but this violates the profile of the gingival margin and worsens the aesthetics. Subsequently, this was done only in case of a significant defect in the outer wall, when demineralized bone or hydroxyapatite was placed in the defect area and covered with a resorbable membrane. In five patients, when removing teeth from the frontal part of the upper jaw, we did not form a vestibular flap, but sutured the mucous membrane around a high plug implant or healing abutment and, if necessary, a periodontal dressing. At the same time, the height and shape of the alveolar ridge is preserved. In the postoperative period, the patient continued to take an antibiotic, an antihistamine, and, if necessary, painkillers. Rinsing with antiseptic solutions was prescribed. For immediate implantation, after removal of the anterior teeth, in 20 patients a superstructure was immediately installed, an impression was taken, and a temporary crown was made on the day of surgery. The temporary crown was necessarily removed from the bite. After 3-6 months, the permanent crown was fixed. Making a temporary crown on the day of implant installation is possible if it is well initially stabilized. This is achieved by screwing in the implant with a force of 35 N/cm using a special ratchet wrench. Analysis of radiological and clinical data of patients after immediate installation of dental implants in patients diagnosed with chronic periodontitis suggests that this method is effective. Results were followed up to four years. Bone atrophy in the area of the implant neck did not exceed 0.1 - 0.2 mm per year. The mucous membrane in the area of the implants was of normal color, the depth of the gum pocket did not exceed 1 - 1.5 mm. In patients who had a temporary crown removed from the bite installed on the day of surgery, long-term data did not differ from those listed above. Therefore, it can be recommended to make a temporary crown immediately after installing the implant for defects included in the area of the anterior teeth of the upper jaw.
Case history No. 1
Patient, 37 years old, case history no. 28545, came to the clinic with complaints about the destruction of crown 36. The patient expressed a desire to compensate for the defect in the dentition with a crown on an implant and unwillingness to make a bridge supported by 35 and 37. Past diseases: childhood infections, influenza and ARVI. Denies allergic reactions. Local status:
In area 36, destroyed roots are determined, 37 and 35 - intact.
The radiograph reveals the roots of 36, the expansion of the periodontal fissure in the area of the medial and distal roots. Diagnosis:
Chronic fibrous periodontitis 36. After discussing the treatment plan with the patient, it was decided to remove the roots of 36, install a dental implant and compensate for the defect with a metal-ceramic crown. Under premedication and local anesthesia with ultracaine, roots 36 were removed; after careful curettage, an implant with a diameter of 4 mm, a neck diameter of 6 mm, a length of 13 mm was inserted into the area of the distal root; the socket of the medial root was filled with hydroxyapatite powder. The socket and implant are covered with a thin Parodontol membrane. Vicryl seams. The course is unremarkable. The sutures were removed on the 14th day. Postoperative course without complications. After three months the implant is opened. An abutment was installed and a metal-ceramic crown was made. The patient is observed for 4 years. There are no changes in bone tissue in the implant area. There is slight bone resorption in the area of the 0.5 mm cone-shaped part of the implant, according to radiography.
Patient Sh., 38 years old, case history no. 39016, was referred to the clinic by a dentist with a diagnosis of chronic granulating periodontitis of the 24th tooth. Case history No. 2
Complaints of minor pain periodically occurring in area 24, destruction of the crown of the tooth. History of the disease:
The 24th tooth was repeatedly treated, the canals were filled, and closed with temporary and permanent fillings. About two months ago, crown 24 collapsed. The patient consulted a dentist. It was not possible to go through channels 24, they were sent to the surgical department to remove 24. Past and concomitant diseases: childhood infections, acute respiratory viral infections, influenza. An X-ray examination reveals a rounded area of rarefaction in the area of the root apexes 24. Perforation of the buccal root in the upper third is determined. After examination and discussion of the situation with the patient, it was decided to remove the 24th tooth and immediate dental implantation. Under premedication and local anesthesia, 24 was removed, with precautions not to injure the cortical plates of the tooth socket. After removal, a thorough curettage was performed. The well is washed with 0.02% chlorhexidine solution. A burr with a diameter of 4 mm and 5 mm was used to expand the burr hole in the area of the buccal root socket. An implant 13 mm long, 5 mm in diameter, root-shaped, coated with hydroxyapatite was inserted. Considering that the diameter of the implant neck is smaller than the diameter of the hole around the implant and a mixture of hydroxyapatite powder and bone filings is introduced into the hole of the palatal root. The implant and socket are covered with a Parodoncol membrane. A flap was mobilized from the vestibular surface of the alveolar process. The flap is sutured with vicryl. After the operation, an antibiotic was prescribed - amoxiclav 350 1 tablet 3 times a day, tavegil 0.05 1 t 3 times a day and ketanov 1 t 2 times a day. The sutures were removed on the 10th day. Three months later, the implant was opened. Installation of an abutment instead of a gum former and fixation of a temporary crown. Three months after installation of the abutment, a metal-ceramic crown was made. Long-term results were followed up to three years. X-ray examination revealed no changes in the bone surrounding the implant. Radiologically detectable bone atrophy in the area of the implant neck is 0.2 -0.3 mm, after three years.
The patient's current condition
Abdominal discomfort when examined by a gastroenterologist will help make a diagnosis.
Condition category: mild severity. Consciousness: consistently clear. Body type: regular, hypersthenic. Patient activity: active. Parameters: height – 186 cm, weight – 97 kg, body temperature – 36.6 degrees Celsius. Lipid, epithelial and muscle tissues, as well as bone structures, are moderately and satisfactorily developed. There are no problems with any nodes in the body, with the exception of the gastrointestinal tract.
Inspection of the basic components of the body
Respiratory organs: the anatomy is normal, there are no pronounced disorders, the location and structure are symmetrical, the patient breathes through the nose and mouth, the type of breathing is mixed, the frequency of respiratory function is about 22 inhalations/exhalations per minute.
Epithelium: no problems, developed normally, good condition. Muscles and skeleton: no pathologies, well developed. Cardiovascular system: no pathologies were identified during the basic examination. Other body nodes: no pathologies were identified.
Dental treatment is the most widespread type of specialized medical care, which is addressed to patients of all age categories. In industrialized countries in 2000, about 20% of the population was over 60 years of age. According to demographic observations, the proportion of elderly people among the population will continue to grow. 30% of all patients at a dental appointment belong to the anesthetic risk group, that is, they have concomitant diseases [1]. It is also noted that 74% of elderly patients have at least four concomitant diseases, 38% have up to six, and 13% have eight or more [2]. In addition, many patients are sometimes not sufficiently aware of the presence of general somatic diseases, which complicates the assessment of the degree of risk during dental intervention.
The need for dental treatment does not exclude the presence of pathologies in the patient from the cardiovascular, bronchopulmonary, nervous, endocrine, and immune systems; severe damage to the liver, kidneys, as well as elderly and senile age, when compensatory capabilities decrease, which can lead to the development of complications.
Collection of anamnestic data to identify concomitant general somatic pathology
Before providing dental care in an outpatient setting, it is necessary to collect an anamnesis, which is usually carried out in two forms - a questionnaire and a survey. Questioning is convenient to conduct at the pre-medical stage, but it should be noted that a single standard form of questionnaires for collecting anamnesis has not been developed to date.
In questionnaires used within the Russian Federation, the patient is asked to indicate the presence of diseases (Appendix No. 1)
, but the patient may not know that he is sick.
Considering this fact, colleagues from the USA consider it advisable to ask the patient questions in questionnaires about the presence of the most common symptoms of diseases (Appendix No. 2)
. Of course, the use of such questionnaires, due to the large number of questions, significantly increases the time required to collect anamnesis, but makes it possible to identify concomitant diseases in the patient, even if the patient did not know about their presence [3].
The data obtained during the survey must be carefully analyzed by a doctor to conduct a survey, during which additional questions should be asked, according to the diseases indicated by the patient. It should be noted that it is at the interview stage that the “doctor-patient” contact is established.
A thorough history taking allows us to identify concomitant pathologies in the patient, draw up a treatment plan, justify the choice of means and method of pain relief, which will help avoid the development of emergency conditions during a dental appointment.
Content analysis of the drug therapy used by the patient
A large number of concomitant diseases entails taking an equal number of medications—polypharmacy. In modern clinical practice, various combinations of drugs are widely used and the unreasonable simultaneous prescription of more than 5 drugs for the treatment of one disease is one of the problems of modern medicine. Polypharmacy is often the cause of adverse drug interactions. When taking 8 drugs, complications of drug therapy occur in 10% of patients, and when taking 16 - in 40% of patients [4]. An analysis of cases of polypharmacy in Moscow hospitals showed that it occurs in 25% of treatment cases [5].
All pharmacological drugs used by the patient must be included in the medical history. The choice of methods of sedation and local anesthesia is determined based on an analysis of their interaction with the medications that the patient takes in the treatment of concomitant diseases, and the dentist should be interested in the entire list of medications that the patient is currently taking.
Careful collection of anamnesis and analysis of possible negative interactions of medications with painkillers will help to avoid severe general somatic complications during a dental appointment. But it is worth remembering that the patient does not always indicate the presence of previously diagnosed diseases.
When using a local anesthetic solution with a vasoconstrictor (most often epinephrine) in a patient taking beta-blockers, a rise in blood pressure (BP) is possible due to a decrease in the hypotensive effect.
Sympathomimetics weaken the effect of alpha- and beta-blockers (carvedilol, opoxyphenoxymethyl, methyloxadiazole). Drugs from the diuretic group weaken the effect of the vasoconstrictor, which can lead to a decrease in the effectiveness and duration of action of the local anesthetic. With simultaneous use of 1,4-dihydropyridines (nifedipine, nitrendipine, nicardipine, etc.) with sympathomimetics, the antihypertensive effect may be reduced due to sodium retention. When using epinephrine simultaneously with cardiotonic drugs (dopamine, phenylephrine), the risk of arrhythmias increases. It is necessary to take into account the use of antiarrhythmic drugs (digoxin), since adrenergic agonists also increase the likelihood of arrhythmia [6].
Taking various antipsychotics, tranquilizers, hypnotics and anxiolytics by the patient requires careful selection of methods and means for local anesthesia. Thus, droperidol and hydroxyzine reduce the pressor effect of epinephrine, while chlorpromazine enhances the effect of local anesthetics. Flupenthixol, when used simultaneously with epinephrine, can cause a sharp drop in blood pressure [7].
Most anticoagulant drugs do not have a description of their interaction with vasoconstrictors, but the combined use of warfarin with lidocaine increases the risk of bleeding [8].
If the patient is taking anticoagulants, the effect is assessed using the international normalized ratio (INR). If the INR value is less than or equal to 2.0, then dental treatment is possible, but if the INR value is greater than 3.0, consultation with the attending physician is necessary about the possibility of reducing the dose of anticoagulants to achieve values less than 3.0. If the attending physician concludes that changes in the use of anticoagulants are impossible in the acute period of ischemic stroke, then treatment is carried out without reducing the dose, since the risks associated with the possibility of recurrent strokes are much higher than the risks associated with bleeding [9].
Depending on the results of the content analysis, the choice of drugs for sedation and local anesthesia is determined, which will help avoid emergency conditions in an outpatient dental appointment.
Determination of the patient's functional state before dental intervention
Regardless of the presence or absence of concomitant pathology, all patients require an assessment of their functional state on the day of their visit to the dentist, which includes a rapid assessment of blood pressure and determination of heart rate (HR).
Method for determining blood pressure
In order to determine blood pressure and heart rate using the simplest and most accessible auscultatory method according to N.S. Korotkov, the dentist will need no more than 5 minutes. The use of automated (auscultatory or oscillometric) devices is allowed, but only in cases where their accuracy in clinical practice is confirmed in special studies [10]. In modern clinics, such devices are installed in the examination room or at the entrance to the clinic. The results obtained can be entered into the medical history. For patients whose blood pressure levels exceed the norm, planned dental treatment is recommended to be postponed, and emergency dental care is recommended to be provided after blood pressure correction [6, 11].
A study to identify the incidence of patients with arterial hypertension at an outpatient dental appointment, including 1590 patients aged 18 to 85 years (730 men and 860 women), showed that at a dental surgical appointment, systolic blood pressure (SBP) ≥140 mmHg. Art. and diastolic blood pressure (DBP) ≥90 mmHg. occur in 75% of patients (Fig. 1) [12]. At a therapeutic appointment before routine dental care, SBP readings≥140 mmHg. and DBP ≥90 mm Hg. were noted in 34.6% of patients, and before emergency dental intervention, an increase in blood pressure levels was recorded in 65.9% of patients. At an orthopedic dental appointment, an increase in blood pressure was detected in 29.5% of patients.
Rice. 1. Percentage of patients with SBP≥140 mmHg. and DBP ≥90 mm Hg. when providing various types of outpatient dental care.
Heart rate determination
Determination of heart rate is carried out by assessing the pulsation on the radial artery of the left hand with the tips of the II, III and IV fingers, covering the patient’s hand in the area of the wrist joint with the right hand. After detecting a pulsating radial artery, the properties of the arterial pulse are determined: frequency of beats per minute, rhythm, tension, filling, magnitude. A pulse rate of less than 60 beats per minute is considered bradycardia, and a pulse rate of 80 to 120 beats per minute is considered tachycardia.
For patients suffering from diabetes, the protocol for assessing their physical condition on an outpatient basis includes determining the level of glucose and glycated hemoglobin in the blood using various devices that can be either in the clinic or with the patient.
If the patient is taking anticoagulants, then before dental surgery it is also recommended to determine INR values in an outpatient dental appointment using special devices.
Thus, in order to prevent emergency conditions before a dental appointment, a mandatory condition is to determine the patient’s functional state.
Monitoring hemodynamic parameters
During dental interventions in patients with concomitant pathologies, monitoring of hemodynamic parameters is recommended. For this purpose, we use a pulse oximeter to record heart rate, a tonometer to measure blood pressure (Fig. 2), and, if available in the clinic, a separate monitor with registration of all hemodynamic parameters, intended for anesthesia (Fig. 3).
Rice. 2. Measuring blood pressure with a mechanical tonometer.
Rice. 3. Monitoring of hemodynamic parameters during the provision of dental care in an outpatient setting.
ASA Anesthetic Risk Classification
When treating patients with general somatic pathology, the dentist does not have any difficulties using various modern technologies, but questions arise about the safety of providing outpatient care.
In patients with a history of a risk factor, the dentist determines the need for consultation with the attending physician (therapist, immunologist, etc.) and further examination. Based on the data received from specialists, the dentist decides on the location of dental care (in a multidisciplinary or specialized hospital or in an outpatient dental facility), based on the international classification of anesthetic risk ASA, which distinguishes 5 classes of the physical condition of patients. This classification is adapted to dental practice by Professor S.F. Malamed and is widely used in world practice [13].
On an outpatient basis, it is possible to receive patients of classes I and II. Class III patients can be admitted on an outpatient basis only with the permission of the attending physician and/or after consultation with an anesthesiologist. If care is provided on an outpatient basis, then the presence of an anesthesiologist is necessary [12].
Profile examination by a gastroenterologist
Chronic pancreatitis can be examined using ultrasound.
The structure and anatomy of the ribs, gastrointestinal tract and nearby organs are not disturbed. The abdomen is slightly enlarged in size due to the presence of ascitic fluid, the appearance of which is caused by an attack of the disease.
The belly shape is “frog”. There is symmetry, complete. There are no hernias, ulcers or similar formations. The patient has his own teeth.
CASE STORIES OF PATIENTS WHO ARE SUGGESTED TOOTH EXTRACTION AND OTHER SURGICAL PROCEDURES
CASE STORIES OF PATIENTS WHO ARE SUGGESTED TOOTH EXTRACTION AND OTHER SURGICAL PROCEDURES
MANIPULATIONS IN THE MAXILLOFACIAL AREA
Part 1. Polyclinic
Service
Example No. 1. Exacerbation of chronic
Periodontitis
Option for recording local changes:
Complaints of pain in the upper jaw on the left and when biting on 27.
History of the disease. 27 was previously treated for chronic pulpitis and was periodically bothered. Two days ago, 27 fell ill again, pain appeared in the area of the upper jaw on the left, and the pain when biting on 27 increased. History: influenza, appendicitis.
Local changes. No changes are detected during external examination. The submandibular lymph nodes are slightly enlarged on the left, painless on palpation. The mouth opens freely. In the oral cavity: 27 under the filling, the color is changed, percussion is painful. On the gum on the vestibular side in the area of the projection of the apexes of the roots 27, a slight swelling of the mucous membrane is detected; palpation of this area is slightly painful.
On the radiograph: the palatal root of 27 is sealed to the level of the physiological apical foramen, the buccal roots are filled to 1/2 of their length. At the apex of the anterior buccal root there is a loss of bone tissue with unclear contours.
Dental formula: (specify).
Diagnosis: “Exacerbation of chronic periodontitis 27.”
Options for recording performed manipulations
with exacerbation of chronic periodontitis:
A) Under tuberal and palatal anesthesia with a 2% solution of lidocaine - 5 ml (or specify another anesthetic) with a 0.1% solution of adrenaline hydrochloride - 2 drops (or without it), 27 was removed, the hole was curetted, the edges of the hole were compressed, the hole was filled blood clot.
B) Under infiltration and palatal anesthesia (anesthetics, see the entry above, indicate the presence of a vasoconstrictor - adrenaline, or its absence), removal of 27 was performed, curettage of the hole, the edges of the hole were compressed, the hole was filled with a blood clot.
In cases of performing manipulations on other teeth, for example 24 and 22:
B) Under infiltration and palatal anesthesia (anaesthetics, see the entry above, indicate the presence of adrenaline), 24 was removed. Curettage of the socket, the edges of the socket were compressed, the socket was filled with a blood clot.
D) Under infraorbital and palatal anesthesia (see anesthetics above, indicate the presence of adrenaline), 24 was removed. Curettage of the socket, the edges of the socket were compressed, the socket was filled with a blood clot. E) Under infiltration and incisive anesthesia (see anesthetics above, indicate the presence of adrenaline), 22 was removed. Curettage of the socket, the edges of the socket were compressed, the socket was filled with a blood clot. E) Under infraorbital and incisal anesthesia (see anesthetics above, indicate the presence of adrenaline), 22 was removed. Curettage of the socket, the edges of the socket were compressed, the socket was filled with a blood clot.
Example No. 2. Acute purulent periodontitis
Option for recording local changes:
Complaints of acute pain in the area of 34, radiating into the ear, pain when biting on 34, a feeling of an “overgrown” tooth. General condition is satisfactory, previous diseases: pneumonia, childhood infections.
History of the disease. About a year ago, pain first appeared at 34, especially at night. The patient did not see a doctor; gradually the pain subsided. 34 days ago he fell ill again, the patient consulted a doctor.
Local changes. No changes were found during external examination. The submental lymph nodes are slightly enlarged, mobile and painless on palpation. The mouth opens freely. In the oral cavity: 34 - there is a deep carious cavity communicating with the tooth cavity, 34 is slightly mobile, percussion is painful. The mucous membrane of the gums in area 34 is slightly hyperemic and swollen. When carrying out EDI, the tooth does not respond to currents above 100 µA.
On X-ray 34: there are no changes in the periapical tissues.
Dental formula: (specify).
Diagnosis: “Acute purulent periodontitis 34.”
Options for recording performed manipulations
for acute purulent periodontitis:
A) Under mandibular and infiltration anesthesia (see anesthetics above, indicate the presence of adrenaline), 34 was removed, the socket was curettaged, the edges of the socket were compressed, the socket was filled with a blood clot. B) Under torusal anesthesia (see anesthetics above, indicate the presence of adrenaline), 34 was removed. Curettage of the socket, the edges of the socket were compressed, the socket was filled with a blood clot.
In cases of performing manipulations on other teeth, for example 31 and 12:
B) Under bilateral mandibular anesthesia (see anesthetics above, indicate the use of adrenaline), 31 was removed. Curettage of the socket, the edges of the socket were compressed, the socket was filled with a blood clot.
D) Under infiltration and incisive anesthesia (see anesthetics above, indicate the presence of adrenaline), 12. Curettage of the socket was removed, the edges of the socket were compressed, the socket was filled with a blood clot.
Example No. 3. Acute purulent periostitis
Upper jaw
Option for recording local changes:
Complaints of swelling of the right cheek, pain in this area, increased body temperature to 38°C. Previous and concomitant diseases: duodenal ulcer, colitis.
History of the disease. Five days ago pain appeared at 14, two days later swelling appeared in the gum area of this tooth, and then in the cheek area. The patient did not go to the doctor, applied a heating pad to his cheek, did warm intraoral soda rinses, took analgin, but the pain grew, the swelling increased, and the patient went to the doctor.
Local changes. An external examination reveals a violation of the facial configuration due to swelling in the buccal and infraorbital areas on the right. The skin over it is not changed in color, it folds painlessly. The submandibular lymph nodes on the right are enlarged, slightly compacted, slightly painful on palpation. The mouth opens freely. In the oral cavity: 14 - the crown is destroyed, percussion is moderately painful, mobility is grade II. Pus is released from under the gingival margin 14. The transitional fold in the area 13,15,14 bulges significantly, is painful on palpation, a positive symptom of fluctuation is determined.
Dental formula: (specify).
Diagnosis: “acute purulent periostitis of the upper jaw on the right in the area 15,14,13.”
Example No. 4. Acute purulent periostitis
Lower jaw
Option for recording local changes:
Complaints of swelling in the area of the lower lip and chin, sharp pain in the anterior part of the lower jaw and pain when biting in the 32nd area, general weakness, lack of appetite, increased body temperature
up to 37.6°C.
History of the disease. After hypothermia, a week ago spontaneous pain appeared in area 32, which had previously been treated, pain when biting on a tooth. On the third day from the onset of the disease, the pain in the tooth decreased somewhat, but swelling of the soft tissues appeared in the area of the lower lip, which gradually increased. The patient did not undergo treatment. He went to the clinic on the 4th day of the disease.
Past and concomitant diseases: influenza, sore throat, penicillin intolerance.
Local changes. During an external examination, swelling of the soft tissues in the area of the lower lip and chin on the left is determined; its soft tissues are not changed in color and are folded freely. The submental lymph nodes are slightly enlarged, slightly painful on palpation. Opening the mouth is not difficult. In the oral cavity: the transitional fold in the area 31,32,33 is smoothed, its mucous membrane is swollen and hyperemic. Palpation reveals a painful infiltrate in this area and a positive symptom of fluctuation. Crown 32 is partially destroyed, percussion is slightly painful, degree I mobility is noted. Percussion of 31 and 33 is painless.
Dental formula: (specify).
Diagnosis: “Acute purulent periostitis of the lower jaw in the chin area on the left.”
Option for recording surgical intervention for acute purulent periostitis of the jaws:
Under mandibular (torusal, infiltration) anesthesia (see the anesthetic above, indicate the presence of adrenaline), an incision was made along the transitional fold in the area of (indicate the formula of the teeth) 2 cm (3 cm) long to the bone. Pus was obtained. The wound was drained with a rubber strip. Prescribed (indicate medications prescribed to the patient and their dosage).
The patient is incapacitated from _______________ to _________________________, sick leave No.____________________ has been issued. Turnout_______________________________________________ (specify number) on
dressing.
An option to record a diary of a patient's dressing after an intraoral incision for acute purulent periostitis of the jaw:
The patient's condition is satisfactory (or moderate). Notes improvement (or worsening, or no change). The pain in the jaw area has decreased (or increased, remains the same).
On examination: swelling of the soft tissues in the chin (cheek) area has decreased, the mouth opens freely, in the oral cavity: a small amount of pus is released from the wound. The wound is washed with a 3% solution of hydrogen peroxide (or a solution of furatsilin at a dilution of 1: 5000). A rubber strip is inserted into the wound (or: the wound is drained with a rubber strip). A Vaseline bandage is applied to the cheek (chin) area. UHF therapy was prescribed for the area of the chin (or upper jaw) No. 7 for 10 minutes.
Example No. 5. Palatal abscess
Options for recording local changes:
Complaints of pain in the area of the hard palate on the left of a pulsating nature and the presence of swelling on the hard palate. The pain intensifies when touching the swelling with the tongue.
History of the disease. Three days ago, independent pain appeared in the previously treated 24, pain when biting on this tooth and the feeling of an “overgrown tooth”. Then the pain in the tooth decreased, but a painful swelling appeared on the hard palate, which gradually increased in size.
Past and concomitant diseases: stage 2 hypertension, cardiosclerosis.
Local changes. Upon external examination, the configuration of the face has not changed. Palpation reveals an increase in the submandibular lymph nodes on the left, which are painless. Mouth opening freely. In the oral cavity: on the hard palate on the left, respectively 23,24, there is an oval-shaped bulge with fairly clear boundaries, the mucous membrane above it is sharply hyperemic and edematous. In the center of the bulge, palpation reveals a positive symptom of fluctuation. Crown 24 is partially destroyed, there is a deep carious cavity. Percussion 24 is painful. X-ray 24 shows cystogranuloma in area 24.
Dental formula: (specify).
Diagnosis: “Acute purulent periostitis of the upper jaw on the palatal side on the left (palatal abscess).”
Option to record the manipulations performed when
palatal abscess:
Under palatal and incisal anesthesia (specify anesthetic), the abscess of the hard palate was opened with excision of soft tissue in the form of a triangular flap of the mucous membrane to the bone within the entire infiltrate, and pus was obtained.
The wound was drained with a rubber strip. Drug therapy was prescribed (specify which).
The patient was incapacitated from ________________________________________________ to _______________________________________________________________________, sick leave No. _________________________________________________ was issued. Appearance__________________________________________________________________________ (specify
number) for dressing.
Diary recording option for palatal
abscess:
The condition is satisfactory. Notes a decrease in pain in the area of the postoperative wound. Body temperature is within 37.3°C. The mouth opens freely. In the oral cavity: after removing the drainage from the wound, no discharge of pus was detected. The wound is washed with a 3% hydrogen peroxide solution. Continue previously prescribed medication.
Turnout_________________ (specify date) for dressing.
Example No. 6. Acute purulent odontogenic
Osteomyelitis of the lower jaw
Option for recording local changes:
Complaints of shooting, boring pain in the area of the entire half of the lower jaw on the right, general weakness, increased body temperature up to 39°C, chills, sweating, bad breath.
Previous and concomitant diseases: practically healthy.
History of the disease . Five days ago, pain appeared in the previously treated 46, pain when biting on this and adjacent teeth, swelling of the gums and cheeks on the right. I had chills at night and went to the doctor in the morning. The tooth was removed, but there was no improvement. Pain in the jaw and general weakness increased, numbness of the skin of the lower lip on the right, and bad breath appeared. The swelling of the soft tissues increased, and the body temperature increased.
Local changes . An external examination reveals significant swelling in the submandibular and cheek areas on the right; the skin above it is hyperemic, tense, and does not fold. Palpation of soft tissues is painful. Pain sensitivity of the skin of the lower lip and chin on the right is reduced. Palpation of the base of the lower jaw on the right is sharply painful. In the oral cavity: the mucous membrane of the alveolar part of the lower jaw in the area 45,46,47 on the vestibular and lingual sides is swollen and hyperemic. Percussion 45,46,47 is sharply painful, the teeth are mobile. A bulge is detected along the transitional fold in the area of 47,46,45 on the vestibular side, and infiltration of the soft tissues of the alveolar part in the area of these teeth on the lingual side. Pus is released from the removed socket 46.
Dental formula: (specify).
Diagnosis: “Acute purulent odontogenic osteomyelitis of the lower jaw on the right, inflammatory infiltrate in the submandibular and buccal areas on the right.”
Option for recording surgical intervention for acute odontogenic osteomyelitis of the mandible:
Under torusal anesthesia (specify the anesthetic), an incision was made along the transitional fold to the bone in the area 45,46,47, and pus was obtained. An incision was also made to the bone in the area of the alveolar part on the lingual side within these teeth, no pus was obtained, and stagnant blood was obtained. The wounds are drained with rubber strips.
Drug therapy was prescribed (specify which). The patient is incapacitated from _____________________________________________________ to________________ _______________________________________________________, sick leave No. _________________________________________________ was issued. Turnout_______________________________________________________________ (specify number) on
dressing.
Option for recording a diary for acute odontogenic osteomyelitis of the mandible:
The condition is satisfactory. Notes a decrease in pain in the lower jaw. Body temperature decreased to 37.5°C. The mouth opens freely. In the oral cavity: after removing the drainage from the wound, a small amount of pus was obtained. The wound is washed with a 3% solution of hydrogen peroxide (or other anesthetic) and drained with a rubber strip.
Continue previously prescribed medication.
Turnout (specify date) for dressing
Example No. 7. Odontogenic cystogranuloma
Option for recording local changes:
Complaints of recurring pain in area 12. The tooth was previously treated with canal filling. Considers himself practically healthy.
Local changes. Upon external examination, the facial configuration is not disturbed. The submandibular lymph nodes are not palpable. The mouth opens freely. In the oral cavity: the mucous membrane is pale pink, well moisturized. Upon examination and palpation of the alveolar process of the upper jaw from the vestibular side, a slight bulging of tissues in the area of the projection of the apex 12 is determined. Percussion 12 is painless, the tooth is discolored, there is a filling.
On the radiograph, in the area of the apex 12 there is a rarefaction of bone tissue of a round shape with clear contours, with a diameter of 0.6 cm. Channel 12 is sealed 2/3 with cement.
Dental formula: (specify).
Diagnosis: “Cystogranuloma in area 12.”
Option to record the operation of root apex resection:
Under infraorbital (or infiltration) and incisive anesthesia (specify the anesthetic and adrenaline solution, if used), a semi-oval (or trapezoidal) incision was made in the soft tissue of the alveolar process to the bone at the level 11,12,13. A flap is formed with its base facing the transitional fold.
The mucoperiosteal flap has been detached in the area of (specify the teeth formula). A usura was found in the compact lamina of the alveolar process (if there was one), which was expanded with a bur. The apex of root 12 was exposed along with the granuloma, the apex of root 12 was resected using a fissure bur, which was then removed with a curettage spoon along with the cystogranuloma. The protruding part of the root is smoothed with a milling cutter to the bottom of the bone cavity. Streptocide powder (or another substance - indicate which) is injected into the wound. The flap is placed in place and fixed with interrupted catgut sutures. A pressure bandage is applied to the upper lip area. Drug therapy was prescribed (specify which). The patient is incapacitated from work, a sick leave certificate No. has been issued. Turnout
______ (specify number) for dressing.
Example No. 8. Semi-retention and dystopia of teeth
Option for recording local changes:
Complaints of periodic pain in the left lower jaw and difficulty opening the mouth. Past and concomitant diseases: hypertension, penicillin intolerance.
History of the disease. He considers himself sick for about 1 year. In February, for the first time I felt the appearance of painful swelling of the gums in the area of 37 and some difficulty opening my mouth. I went to the district clinic, where treatment was carried out: 5 sessions of UHF therapy on the area of the angle of the lower jaw on the left, took sulfadimethoxine orally according to the scheme, and took baths with baking soda. The above phenomena subsided and he was sent for consultation to the regional clinic.
Local changes. Upon external examination, the configuration of the face is not disturbed; palpation reveals an enlarged to 1.5 cm in diameter, painless, mobile submandibular lymph node on the left. Opening the mouth is free and painless. In the oral cavity: the mucous membrane of the vestibule of the mouth is pale pink, sufficiently moist. It is noted that 38 is cut through by two distal tubercles and is displaced (inclined) towards 37.
On the lateral radiograph of the lower jaw it is determined: 38 is inclined towards 37, with its medial tubercles adjacent to the distal root of 37.
Dental formula: (specify).
Diagnosis: “Semi-retention and dystopia 38.”
Option for recording a complex tooth extraction operation
wisdom:
Under mandibular and infiltration (or torus) anesthesia (specify the type of anesthetic), an angular incision was made and the mucoperiosteal flap was detached in the area 37,38. The compact plate of alveolar bone tissue in area 38 was trepanned with a bur from the vestibular and retromolar sides. The bone tissue was removed with a bur, completely exposing the crown 38 and partially exposing its root on the vestibular side. The tooth was dislocated with an elevator and removed with forceps. The wound is washed with a 3% solution of hydrogen peroxide, white streptocide powder is poured into it (or another medicinal substance is injected - indicate which one). The flap is put in place, the wound is sutured tightly with interrupted catgut sutures. A rubber strip was inserted into the wound along the transitional fold in the area 37-38 on the vestibular side. A pressure bandage was applied to the area of the angle of the lower jaw on the left.
The patient is incapacitated from _________________________________________________________________ to _________________________________________________________________, issued
sick leave No._______________________________________________. Drug therapy was prescribed (specify which). Attendance _________________________________ (specify
number) for dressing.
Example No. 9. Pericoronitis
Option for recording local changes:
Complaints of pain in the area of 37 and 38, pain when swallowing, difficulty opening the mouth and eating.
Past and concomitant diseases: sore throat, denies allergic reactions.
History of the disease. The pain and difficulty opening the mouth began two days ago and is gradually increasing. Taking analgesics orally did not bring improvement and the patient consulted a doctor.
Local changes. Upon external examination, a slight swelling is detected in the left submandibular region due to tissue edema. The skin over the swelling has not changed in color and folds well. Palpation reveals enlarged (up to 2 cm in diameter), compacted, painful, limited mobility of the submandibular lymph nodes on the left. Mouth opening is limited (2 cm between the central incisors), painful. In the oral cavity: the mucous membrane in the retromolar region, the anterior palatine arch on the left and along the transitional fold on the left in area 37 is swollen and hyperemic. In area 38 there is a “hood” of the mucous membrane, from under which a drop of pus was released, 38 was cut through by medial tubercles. Palpation of tissue in area 38 is sharply painful. The tonsils are not enlarged. The tissues in the area of the maxillo-lingual groove on the left are free. An x-ray of the lower jaw in the lateral projection on the left reveals the correct position of 38 in the dentition; no pathological changes in bone tissue are noted in the area of 38.
Dental formula: (specify).
Diagnosis: “Pericoronitis in area 38.”
Option for recording the operation of cutting the hood:
Under mandibular (torusal) and infiltration anesthesia (specify anesthetic), the cut is made in the retromolar region above the crown 38 and to the bone through the middle of the “hood”. The edges of the resulting soft tissue flaps are moved apart, a little pus is obtained, the wound is washed with a solution of furatsilin at a dilution of 1: 5000 (or another antiseptic - indicate which one), an iodoform swab is inserted into it.
The patient is incapacitated from _______ to ________________________. Sick leave No.________________ was issued. Drug therapy prescribed
(specify which one). Appearance________________________________ (specify date) for dressing.
Option for recording the hood excision operation:
Under mandibular (torusal) and infiltration anesthesia (specify anesthetic), soft tissue was excised in area 38, the tooth crown was completely freed from the mucous membrane. The wound in the distal section 38 is covered with an iodoform swab.
The patient is incapacitated from __________________________________________________________________________ to __________________________________________________________________________, issued
sick leave No.__________________________________________. Medication prescribed
therapy (specify what). Appearance__________________________________________________________________________ (specify date) for dressing.
Post-excision journaling option
or cutting the hood:
The condition is satisfactory. Body temperature 37.5°C. Notes pain when opening the mouth and swallowing. When viewed from the outside, no changes are noted. The submandibular lymph nodes are enlarged and painless. The mouth opens 1.5 cm between the incisors. During forced separation of the jaws, it was found that iodoform turunda is well fixed in the area of the crown of the wisdom tooth, the soft tissues in the tooth area are hyperemic and edematous. Turunda is stewed with 3% iodine tincture. Continue drug treatment, show up_________________________________________________________________________ (specify date) for dressing.
Glands of the lower lip
Option for recording local changes:
Complaints about a spherical formation in the area of the lower lip on the right, which does not hurt, but interferes with eating. Previous and concomitant diseases: flu, sore throat.
History of the disease . About 3 months ago, the patient bit his lower lip while eating. A few days after this, I noticed the appearance of a small formation in the thickness of the lower lip on the right, which gradually enlarges, does not hurt, but interferes with eating. I went to the doctor.
Local changes. On external examination, a slight change in the configuration of the face is noted due to swelling in the area of the lower lip on the right. Regional lymph nodes are not palpable. Opening the mouth is free and painless. In the oral cavity: the mucous membrane is pale pink, sufficiently moist. On the inner surface of the lower lip on the right, a rounded formation with a diameter of 0.7 cm is determined, different in color from the surrounding mucous membrane. On bimanual palpation, a round-shaped formation is determined in the thickness of the lower lip on the right, soft-elastic consistency, painless, mobile.
Dental formula: (specify).
Diagnosis: “Retention cyst of the minor salivary gland of the lower lip.”
Option for recording the retention removal operation
cysts of the lower lip:
Under infiltration anesthesia (specify anesthetic), the mucous membrane of the lower lip on the right above the formation was dissected with two semi-oval converging incisions. Using a Mosquito hemostatic clamp, scissors and a scalpel, the retention cyst was isolated from the surrounding tissues and removed, and hemostasis was performed during the operation. The wound is sutured with interrupted catgut sutures. A pressure bandage was applied to the lower lip area. The patient is incapacitated from ________________________________________________________________________________ to __________________________________________________________________________, issued
sick leave No.__________________________________________. Turnout___________
Option for recording a diary after surgery to remove a retention cyst:
The condition is satisfactory. Complaints of slight pain in the lower lip area. The sutures secure the edges of the wound well; there is slight postoperative swelling of the soft tissues in this area. The suture area is treated with 1% tincture of iodine. Appearance________________________________________________________________________________ (specify date) for dressing.
Example No. 11. Papilloma of the tongue
Option for recording local changes:
Complaints about the presence of a tumor on the tip of the tongue, which interferes with eating, and sometimes bleeds when it is injured by food. Previous and concomitant diseases: practically healthy, denies allergic reactions.
History of the disease. The patient noticed the appearance of a tumor on the tip of the tongue about 3 months ago, when a bridge was made in the area 44-33.
Notes the gradual growth of the tumor.
Local changes. During an external examination, no changes in facial configuration were noted. Regional submandibular and submental lymph nodes are not palpable. Opening the mouth is free and painless. In the oral cavity: the mucous membrane is pale pink, well moisturized. At the tip of the tongue there is a neoplasm measuring 0.5 cm in diameter, on a narrow stalk. On palpation - soft, painless, mobile. On the mucous membrane of the neoplasm there are fringed outgrowths that are barely noticeable upon examination.
Dental formula: (specify).
Diagnosis: “Papilloma of the tongue.”
Option to record the operation of excision of a benign neoplasm of the tongue (papillomas, fibromas, etc.):
Under mandibular (or infiltration, lingual) anesthesia (specify anesthetic), two semi-oval converging incisions were used to excise the tumor within healthy tissue down to the muscle layer. The wound is sutured with interrupted catgut sutures. The patient is incapacitated from _____ to _____________________________________, a sick leave certificate has been issued
No._____________________. Appearance __________________ (specify date) for dressing.
Option for recording a diary after surgery to remove a tumor on the tongue:
The condition is satisfactory. Complaints of slight pain in the tongue area. The sutures secure the edges of the wound well; there is slight postoperative swelling of the soft tissues in this area. The suture area is treated with 1% tincture of iodine. Appearance_______________________ (specify date) for dressing.
Example No. 12.Epulis
Option for recording local changes:
Complaints about the presence of a formation on the gum of the upper jaw on the left, bleeding when brushing teeth and biting hard food. Past diseases: childhood infections, influenza, acute respiratory infections.
History of the disease. Three months ago I noticed the appearance of a formation on the gum of the upper jaw on the left, which gradually enlarges and bleeds when eating.
Local changes. No changes are detected during external examination. Regional lymph nodes are not palpable. Opening the mouth is free and painless. In the oral cavity: the mucous membrane is pale pink, moderately moist. On the gum in the area 24-25 there is a mushroom-shaped formation on a wide base, covered with a bluish mucous membrane, 0.7 cm in size, painless on palpation, partially covering the vestibular surface of the crown 24. On the radiograph in the area 24-25 there is a loss of bone tissue.
Dental formula (specify).
Diagnosis: Epulis in the area 24-25.
Option to record the epulis removal operation:
Under infiltration and palatal anesthesia (specify anesthetic), the formation was excised within healthy tissue. Using a bur (cutter, curettage spoon), softened bone tissue is removed. The wound surface is covered with iodoform turunda, fixed with a catgut suture. The patient is unable to work, sick leave has been issued
sheet No. ______________ from _________ to ______. Drug therapy prescribed
(specify which one). Appearance for dressing ________________________________________________________________________________ (specify date).
Journaling option after surgery
epulis removal:
The condition is satisfactory. Complaints of slight pain in the upper jaw. On examination, slight postoperative swelling of the cheek on the left is noted. The sutures fix the iodoform turunda well. Turunda is stewed with 3% tincture of iodine Turnout (specify the number) for dressing.
Example No. 13. Lobulated Fibroma
Option for recording local changes:
Complaints about the impossibility of using a removable denture on the lower jaw due to the appearance of a formation in the area of 42,43,44 and 45. Past and concomitant diseases: arterial hypertension II, acute respiratory viral infection, chronic gastritis.
History of the disease. The formation appeared one year after prosthetics, when a complete removable denture was made for the lower jaw. He notes a gradual increase in education, and therefore cannot use a prosthesis.
Local changes. No changes are detected during external examination. The mouth opens freely. In the oral cavity, the mucous membrane is pale pink in color and well moisturized. On the lower jaw, after removing the complete removable denture at the level of 42, 43, 44, 45, a lobulated formation was found along the transitional fold, on a wide base, painless on palpation, relatively mobile, covered with a slightly hyperemic mucous membrane, soft-elastic consistency.
Dental formula (specify).
Diagnosis: Lobulated fibroma in the area 42-45.
Recording option for lobular excision operation
fibroids:
Under mandibular and infiltration anesthesia (specify anesthetic), two semi-oval converging incisions were used to excise the fibroma. The wound was sutured with interrupted catgut sutures. The patient is incapacitated from _____________________________________________________________________ to _____________________________________________________________________,
sick leave certificate No. was issued. Drug therapy was prescribed (specify which). Appearance for dressing (specify date).
Journaling option after surgery
removal of lobular fibroma:
The condition is satisfactory. Complaints of slight pain in the lower jaw. Upon examination, a slight swelling of the soft tissues of the lower buccal region on the right is detected. The mouth opens freely. The sutures secure the edges of the postoperative wound well; slight swelling of the soft tissues is noted in this area. The suture area is treated with 1% tincture of iodine Yavka (specify the number) for dressing.
Example No. 14. Radicular cyst of the upper jaw
Option for recording local changes:
Complaints of a painless swelling in the upper jaw area on the left, raising the upper lip. Previous and concomitant diseases: the patient is practically healthy.
History of the disease. Previously, 22 was periodically ill, but the patient did not see a doctor. I noticed the swelling about 2 years ago. He noted its gradual increase. Currently, due to a cosmetic defect, I went to the dentist.
Local changes. On external examination, there is a slight swelling of the soft tissues of the upper lip on the left. The skin over the swelling is of normal color, folds well, and upon palpation the tissues are soft and painless. Regional lymph nodes are not palpable. Opening the mouth is free and painless. The base of the lower nasal meatus on the left is elevated (Gerberian ridge). In the oral cavity: the mucous membrane is pale pink in color, sufficiently moist. Upon examination, a limited swelling of semi-oval tissue is determined on the vestibular side of the alveolar process of the upper jaw in the area 21, 22, 23. The mucous membrane above the swelling is pale with a pronounced vascular pattern. Upon palpation, it is noted that the swelling is pliable, moderately dense, and painless. In its center, a mild symptom of “parchment crunch” is determined. Crowns 21 and 22 are converged, 22 is changed in color. On the radiograph: in the area of the alveolar process of the upper jaw on the left, a rarefaction of bone tissue is determined within the limits of 21, 22, 23 with smooth and clear contours, round in shape. The area of bone loss extends to the bottom of the nose.
EDI has been carried out: 22 does not respond to currents above 200 mA.
Dental formula: (specify).
Diagnosis: “Radicular cyst of the upper jaw in the area of 21, 22, 23, pushing back the bottom of the nose.”
Option for recording a cystectomy operation:
Note: the roots of teeth whose apex is resected during surgery must be filled in advance with phosphate cement.
Under infraorbital and incisal anesthesia (specify the anesthetic), a semi-oval (or trapezoidal) incision was made in the mucous membrane and periosteum to the bone in the area 11, 21, 22, 23, 24. A flap was formed with its base facing the transitional fold so that the future bone wound became smaller soft tissue flap. The mucoperiosteal flap was detached in the area 11,21, 22, 23,24. An ulcer was found in a thinned, swollen compact plate of the alveolar process bone, which was expanded with pliers. The shell of the radicular cyst was discovered and completely isolated, the apexes of the roots were resected (specify which ones), which were removed along with the shell of the radicular cyst. The sharp edges of the resulting cavity are smoothed with a milling cutter. Streptocide (or another substance - indicate which one) is poured into the wound, the flap is put in place, the wound is sutured with interrupted catgut sutures. A pressure bandage was applied to the upper lip area.
The patient is incapacitated from _____ to ________________________________, sick leave No. _______________ has been issued. Drug therapy prescribed
(specify). Turnout_____________________ (specify date) for dressing.
Option for recording qi operation
Surveys
To make an accurate diagnosis, the following types of examinations are prescribed:
- blood tests (clinical, biochemistry);
- examination of urine and stool;
- X-ray of the abdominal cavity without contrast;
- Ultrasound of adjacent organs to the gastrointestinal tract (liver, gallbladder, pancreas);
- ECG.
Stages of dental examination
The patient undergoes examination in three stages.
- clarification of complaints and medical history;
- examination using physical methods (inspection, palpation, percussion, auscultation);
- research using special methods (laboratory, x-ray).
The final clinical diagnosis is made after clarifying complaints and other aspects of the disease and collecting additional information about the patient. All this will allow appropriate treatment to be carried out at the next stage.
Test results
A blood test is a very important procedure for making a correct diagnosis.
Based on the results of the surveys, the following results were obtained:
- clinical blood test – indicators are normal;
- biochemical blood test – the indicators are normal;
- X-ray of the abdominal cavity is normal, there are no free gases;
- Ultrasound of the underlying organs to the gastrointestinal tract - the liver is in a “normal” state, the pancreas is moderately enlarged, the gallbladder is in an irregular shape and has no stones.
Conclusion based on the results of the diagnostics: diffuse disorders of adjacent organs to the gastrointestinal tract. The results of the examinations are discussed in more detail in the appendices to the medical history.
e-Dentistry.ru
Extractfrom the medical history
Patient K.E.Yu.,
Born in 1960, medical history No. 702873 dated September 28, 2005.
Complaints:
for recession of the upper lip, violation of facial proportions, inability to chew food, lack of aesthetics, the existing denture on the upper jaw does not hold, destruction of the front teeth on the lower jaw.
Anamnesis
: I used prosthetics many times, but did not get the desired aesthetic effect. The last prosthesis for the upper jaw was made a year ago, the prosthesis does not hold, now without prostheses. He treated the teeth on the lower jaw, but did not complete the treatment and only removed them as they were destroyed. Desperate to get dentures that would improve aesthetics and normalize chewing.
Objectively:
Visual inspection:
face type – “rectangular” shape. Significant reduction in the height of the lower third of the face, sharp expression of nasolabial folds. The significant retraction of the upper lip is partially hidden by the mustache.
Oral examination:
on the lower jaw there are roots 44, 43, 42, 41, 31, 32, 33, the existing teeth are dark brown in color with a destroyed crown part.
43, 42, 41, 31 – movable in the anteroposterior direction, the entrance to the canals is determined by a probe, probing is painless. In the area of the apex of tooth 42 there is a fistulous tract; upon palpation there is purulent discharge.
On the R-image - 42, 41, 31 - there is a vacuum at the tips of the roots measuring 3 mm. 43 – partial destruction of the vestibular surface of the coronal part of the tooth, partially restored with a plastic filling, changed in color and partially destroyed.
32, 33, 34, 35 – mobility in three planes, the canals are empty, there is a vacuum of 2-3 mm at the tops of the teeth.
On the upper jaw there is a complete absence of teeth, significant uniform vertical atrophy of the alveolar process, a wavy line of the alveolar process crest, a shallow vestibule, a sloping slope of the alveolar process, a flat arch of the palate.
The mucous membrane of the oral cavity is pale pink in color, sufficiently moisturized; on the alveolar processes, motionless, pliable, class I according to Supple.
The frenulum of the upper and lower lips is normal. In the area of teeth 14, 13 there is a mucous cord.
Progenic jaw ratio.
Additional examination methods.
X-ray of OPG: the upper jaw lacks teeth and roots. The frontal area does not have a clearly defined bone tissue structure with a large area of extraction defects from tooth 13 to tooth 23; there is no continuous line of the compact plate.
The alveolar process in the area of the chewing teeth on the right has a closure of the compact plates of the maxillary cavity and the alveolar process in the area of teeth 16, 17. On the left there is a separation of the compact plates by cancellous bone of 6 mm.
On the lower jaw there are roots of teeth 44, 43, 41, 31, 32, 33, 34, 35. X-ray contrast material is present only in the canal of tooth 44, the root is fixed in the bone 3 mm.
All roots, except tooth 43, have a vacuum at the root apices of 2-4 mm. Tooth 43 has a widening of the periodontal fissure.
The alveolar process is pronounced. The height of the alveolar process in the area of the chewing teeth is about 20 mm. There are no changes in the bone tissue in the area of the chewing teeth.
Diagnosis:
Complete absence of teeth in the upper jaw. Partial absence of teeth in the lower jaw (Kennedy class I), complicated by a progenic relationship of the jaws. Chronic periodontitis 43, 42, 41, 31, complicated by mobility of the first degree. Chronic periodontitis 44, 32, 33, 34, 35, complicated by mobility of the third degree.
Recommended:
1. Remove 44, 32, 33, 34, 35, which have bone loss at the tops of the teeth and mobility of the third degree.
2. Implantation of two implants on the upper jaw to obtain satisfactory fixation of the upper covering prosthesis and the ability to set teeth in a direct or orthognotic bite with a progenic jaw relationship.
3. Treatment and filling of canals 43, 42, 41, 31 to make it possible to produce inlays with male spherical locking fastenings with their oral displacement for setting artificial teeth with maximum oral displacement to reduce the undesirable progenic relationship of the jaws.
4. Make a covering prosthesis for the upper jaw with fixation on the attachment of a beam structure with the possibility of hinge-like movement when chewing to exclude dislocation movement on the implants, a covering prosthesis for the lower jaw with fixation on single attachments of a spherical design to allow the removal of any conditionally preserved root, and implementation of the installation teeth in an orthognathic or straight bite. In the frontal area, when setting the teeth, create separations to eliminate the tipping movement when closing the teeth.
Visit diary:
29.09.05.
In order to sanitize the oral cavity, the root of the 44th tooth was removed before implantation.
No complaints. In the R-image, the root 44 by 3 mm is immersed in the alveolar process, the depression is at the root apex. Mobility in 3 planes.
Diagnosis:
chronic periodontitis of the third degree of mobility.
Under application mandibular anesthesia sol. Ultrocaini 1.7 ml removed. Alveostasis.
05.10.05.
No complaints. In the R-image, 32, 33, 34, 35 have rarefaction at the root tips, the canals are empty, previously resorcinolized, and mobility is in three planes.
Diagnosis:
chronic periodontitis 32, 33, 34, 35. Third degree mobility. 32, 33, 34, 35 were removed under application mandibular anesthesia sol. Ultrocaini 1.7 ml. Bandage. Alveostasis.
10.10.05.
Joint consultation with an implantologist and orthopedist.
Based:
1. R-images - vertical resorption of the ridge of the alveolar process of the upper jaw with extensive extraction defects of bone tissue in the area of 13, 12, 22, 23 teeth. Proximity of the maxillary and nasal cavities;
2. financial capabilities of the patient;
3. a drawn up orthopedic treatment plan
defined
The optimal location for installing implants is in the area of 21 and 23 teeth.
21.11.05.
No complaints. I feel satisfactory.
Intraosseous implantation in areas 11, 13, bone grafting. Under application mandibular anesthesia sol. Ultrocaini 1.7 ml an incision was made and the mucoperiosteal flap was folded back. Two screw implants were installed in the area of teeth 21, 23. Stitches were applied. Apply cold to the upper lip area for 30 minutes. Recommendations on oral hygiene are given.
26.11.05.
No complaints. I feel satisfactory.
Objectively:
The swelling of the upper lip is insignificant, the dynamics are positive, slight swelling remains in the area of the surgical wound, slight hyperemia along the incision line. Raid.
Diagnosis:
condition after implantation; medicinal and mechanical treatment of the suture line was performed.
02.12.05.
No complaints. The condition is satisfactory. There is no edema or hyperemia. The stitches have been removed. Recommendations on hygiene and timing of prosthetics are given.
13.12.05.
No complaints. Revision of root canals 43, 42, 41, 31. According to the patient, they were previously treated endontically. They are brown in color and are resorcinenes. The root canals are not filled. R-image 43 shows changes in the form of widening of the periodontal fissure. In teeth 42, 41, 31 there are changes in the area of the root apices. In the area of the apex of root 42 in the oral cavity there is a fistulous tract on the vestibular surface of the alveolar process.
Diagnosis:
chronic periodontitis 43, 42, 41, 31. Periostitis 42 – fistulous tract.
Treatment:
mechanical and medicinal treatment of root canals. Channel 43 is sealed with endomethasone paste + thermophil. R-image, filling control 41. Filling to the root apex, temporary filling. Channels 43, 42, 41 are left open.
15.12.05.
Diagnosis: 42, 41, 31 – chronic periodontitis, mechanical treatment of canals. 42, 41, 31 – medicinal treatment of root canals 41, 31, filled with Kalasept medicinal paste, 42 left open. The patient has an appointment.
22.12.05.
There are no complaints, my health is satisfactory.
Diagnosis:
42, 41, 31 – chronic periodontitis. Medicinal treatment 41, 31, sealed with Calasept medicinal paste, temporary filling.
07.12.05.
There are no complaints, my health is satisfactory.
Diagnosis:
42, 41, 31 – chronic periodontitis.
Treatment:
Drug treatment 42, 41, 31, sealed with Calasept medicinal paste, temporary filling. Turnout in a month.
29.03.06.
No complaints.
Diagnosis:
42, 41, 31 – chronic periodontitis.
Treatment:
The R-image shows a slight improvement in the periodontium of the indicated teeth, medicinal treatment of 42, 41, 31 under application mandibular anesthesia sol. Ultrocaini 1.7 ml, sealed with Kalasept medicinal paste, the canals are closed with silidont.
20.06.06.
There are no complaints, my health is satisfactory. The mucous membrane in the implant area is epithalized. Application mandibular anesthesia sol. Ultrocaini 1.7 ml. Incision in the area of the implant. Gum formers are installed in the implants. Stitches have been applied. Sent for prosthetics.
23.06.06.
No complaints.
Diagnosis:
42, 41, 31 – chronic periodontitis.
Treatment:
application and mandibular anesthesia sol. Ultrocaini 1.7 ml, medicinal filling with endomethasone paste + thermophil. Control R-image, in 31 there is a slight extension of the filling material beyond the apex into the granuloma cavity, 42 and 41 are sealed to the root apex. Temporary filling. Sent for prosthetics.
03.07.06.
There are no complaints, my health is satisfactory.
Diagnosis:
complete absence of teeth in the upper jaw, condition after implantation in the area 21, 23, partial absence of teeth in the lower jaw (Kennedy class I), 43, 42, 41, 31 – condition after long-term treatment for periodontitis. The gum formers were removed and treated with antiseptic hydrogen peroxide. Transfers are installed, plastic is fastened.
Taking impressions with an open tray with silicone mass from the upper jaw and alginate mass from the lower jaw.
04.07.06.
I feel satisfactory. No complaints. The central relationship of the jaws was determined using wax bases with occlusal ridges.
12.07.06.
I feel satisfactory. No complaints. Fitting before passive landing of cast abutments with an attachment beam with a unloading mechanism for influencing the supports. Taking an impression with a bar on the abbotmen for the manufacture of an overdenture on the upper jaw. Screwing the healing abutment.
19.07.06.
I feel satisfactory. No complaints. Fixing the abbotmen with the beam with screws, closing the holes with acrylic oxide. Delivery of the finished overdenture with attachment and fixation on the beam. Installation of the matrix in a removable denture. At the patient's request, prosthetic replacement of lower jaw teeth was postponed until October.
13.10.06.
I feel satisfactory. No complaints. Teeth 43, 42, 41,31 do not bother me after treatment. There were no exacerbations. The dynamics are positive.
Objectively:
The fistulous tract of tooth 42 was epithalized. In the R-image, the canals of teeth 43, 42, 41, 31 are filled. In the canal of tooth 42, the filling material was partially removed into the cavity of the granuloma cyst. Percussion is painless.
Teeth 42, 41, 31 are conditionally preserved. Channels 43, 42, 41, 31 were unsealed by 1/2, inlays with caps were modeled and “uni” males were installed using the direct method.
With the consent of the patient, the design of the removable denture was chosen taking into account the removal of any of the conditionally preserved roots without alteration of the entire structure of the combined denture. The holes are closed with a cotton swab and septopak.
23.10.06.
I feel satisfactory. No complaints. Percussion of the roots is painless. Fixation of cast inlays with caps and “uni” males on “Harvard cement”. The patient will return after 2 weeks to monitor the reaction of the tooth roots to the installed structure.
08.11.06.
I feel satisfactory. No complaints. Impressions were taken from the upper prosthesis with alginate mass and the lower jaw with “uni” male inlays with superimposed containers for the manufacture of a covering prosthesis on the lower jaw.
17.11.06.
I feel satisfactory. No complaints. Fitting the metal frame of the covering prosthesis. The central relationship of the jaws was determined.
22.11.06.
I feel satisfactory. No complaints. Checking the wax structure with a metal frame and existing matrix sockets. The patient's appearance is satisfactory.
29.11.06.
I feel satisfactory. No complaints. Delivery of the finished prosthesis. Installation of matrices. Fixation of the prosthesis in the oral cavity on existing inlays with males. Recommendations for the care and use of the prosthesis are given. Appear as necessary for prosthesis correction. Follow-up examination after 6 months.
06.12.06.
Complaints of pain from the upper covering prosthesis in area 26, correction of the prosthesis in the namin area was made.
| OPG with an increase in the area of pathological changes | condition after implantation in the upper jaw |
| conditionally preserved teeth requiring endodontic treatment | final filling of the canal of tooth 43, temporary filling of tooth 42 with Calasept |
| canals of teeth 31, 41,42,43 after pretreatment | screw fixation of abbutmen with beam structure attachment |
| prepared support for a covering prosthesis on the upper jaw and the frontal group of teeth of the lower jaw during treatment | the same, front view |
| appearance of fixed structures in the oral cavity | progenic relationship of jaws with fixed structures |
| completed prosthetics of the upper jaw, preparation of attachments for taking impressions using the direct method from the lower jaw | cast frame of the overdenture with sockets for matrices |
| fitting of the overdenture frame | applying the frame to the model |
| application and fitting of the frame in the oral cavity | placement of overdenture teeth on the lower jaw |
| setting of teeth in orthognathic occlusion | the same, side view |
| overdenture removed from the model | shortening the base of the covering prosthesis along the vestibular slope, corresponding to the undercut area |
| eliminating the retraction of the upper lip and reducing the severity of nasolabial folds | state of physiological rest |
| the same, bottom view | patient's smile |
| OPG after completed prosthetics | |
Diagnosis
Based on the observed history of the patient’s pathology, the results of examinations and medical practice, with the maximum guarantee, a diagnosis can be made - chronic pancreatitis at the acute stage (not an advanced type of pathology). There are no associated diseases, with the exception of mild gastritis.
You can learn more about chronic pancreatitis from the video:
https://www.youtube.com/watch?v=YkefLGAvbKg&t=1459s
Pain symptom
The pain symptom is an important indicator for making a diagnosis. By clarifying complaints, the patient is questioned. The dentist determines the causes of pain, its nature (pulsating, twitching, aching pain), time of occurrence (at night or during the day), duration (constant or attacks), and where pain occurs.
All this information forms the basis for making a diagnosis. The duration of existence of symptoms is established, the dynamics of the pathological process is formed. After this, it is necessary to collect information about the treatment being carried out. Was it carried out and, if so, how effective was it? The patient is questioned about previous diseases, allergy and epidemiological history, and working conditions.
An objective dental ( and not only ) examination consists of examination, palpation (basic methods), percussion and a number of additional methods.
Prescribed treatment
Papaverine is a drug for normalizing the functioning of the pancreas.
In accordance with the patient's history of pancreatitis, he was prescribed the following treatment:
- the first 7 days - observation by a specialist, leave to go home, daily regimen: bed, diet: moderate fasting, medications: Diphenhydramine, Papaverine, Glucose, Novocaine (intravenously, intramuscularly) and Enap tablets (orally);
- 7-30 days after hospitalization - observation by a specialist, special diet, taking preventive medications prescribed by a specialist based on the results of observations;
- after 30 days – maintaining gastrointestinal health according to the recommendations of a specialist.
More precise dosages of drugs, their list and other elements of treatment are discussed in the appendices to the medical history.