Sometimes after a visit to the dentist (treatment, extraction or implantation of a tooth), neurological complications occur. Our clinic specializes in the treatment of facial pain and neurological complications after dental procedures. We will offer you the help of neurologists and ENT doctors with experience in the treatment of facial pain and neurostomatology.
- After treatment, the dentist has a toothache, numbness in the lip, cheeks, pain in the face and jaw, after treatment of pulpitis, a tooth hurts
- Pain after dental implantation, tooth implant hurts
- The mouth does not open after tooth extraction or treatment at the dentist, the temple hurts after treatment or tooth extraction
- The jaw hurts and clicks after prosthetics or dental treatment
- Sinusitis, maxillary sinus cyst, loss of sense of smell after visiting the dentist
Pain after dental implantation, tooth implant hurts
During dental implantation, the trigeminal nerve and its branches, the alveolar nerve plexus, may be damaged as a result of:
- Screwing the implant into the canal where the trigeminal nerve or its branches lies;
- Inflammation in the implant area (infection and/or implant rejection).
Some pain during the implant healing process is normal. If the pain after dental implantation lasts too long, is very severe, or is accompanied by numbness of the lip or cheek, we can check the condition of the trigeminal nerve using electromyography and a neurological examination based on the characteristic loss of facial sensitivity and the spread of pain along the trigeminal nerve system.
The rejection reaction and inflammatory processes in the implant area are usually clearly visible with CORRECT X-ray examination and computed tomography.
Implants in the lower and upper jaw. Pain after dental implantation
There may be direct pressure from the implant on the nerve or inflammation in the implant area with tissue swelling, edema and subsequent pressure on the nerve.
Nerve damage during wisdom tooth extraction
29.10.2020
Probably, nature once wanted a person to be very wise and endowed him with a generous gift - eighth teeth, which now, unfortunately, cause considerable problems. The roots of “eights” are often curved; it is sometimes impossible to fully care for the dental units due to their inconvenient location, which entails the development of caries. In some cases, wisdom teeth bother their owner even at the initial stage of eruption. Considering that the eighth dental units do not bear a functional and aesthetic load, in certain situations a decision is made to remove them.
Possible pain after wisdom tooth removal
- Jaw pain. It can occur due to rupture of ligaments and blood vessels, as well as nerve endings, or the doctor applied light pressure on the jaw to gain access to a distant dental unit.
- Pain when swallowing. They appear after the “figure eight” on the lower jaw has been removed. This happens because a nerve was hit when a wisdom tooth was removed.
Basically, it is problematic to remove a dystopic or impacted tooth; it is located in the bone tissue and has not yet fully erupted. In this case, the bone is sawed and special forceps are used. There is a risk that damage to the trigeminal nerve will occur when wisdom teeth are removed. Persistent pain after removal of a tooth indicates pathology. If the body temperature rises, swelling and bruising appear, and you feel unwell, this indicates the presence of an inflammatory process.
Unbearable toothache usually occurs when the second and third “branches” of the trigeminal nerve become inflamed. Intense pain is localized in the ears, chin, even in the lower lip. Periodically, the acute pain dulls, but the person continues to experience discomfort. The reason is that a nerve was probably hit during the removal of a wisdom tooth, or unsuccessful dental procedures were performed: filling, surgical manipulations. In such a situation, you need to contact your dentist. The doctor will give appropriate recommendations on how to restore the nerve after tooth extraction. Typically, the patient is prescribed B vitamins, as well as drugs that stimulate blood circulation and reduce blood viscosity. Properly carried out therapy can achieve positive results and restore the nerve.
Causes of paresthesia
The “eight” has been successfully treated or removed, the patient returned from the dentist in perfect order, but suddenly a strange feeling of numbness appears on the cheeks, tongue, and lips. The effect of the anesthetic has passed, but the unpleasant symptoms continue: the face becomes as if plastic, tingling, burning, and sometimes pain are felt. These signs indicate the presence of paresthesia.
- Incorrect position of the figure eight, its curved roots or very close dislocation of the processes of the trigeminal nerve - these factors cause damage to the nerve during wisdom tooth removal.
- The wound is swollen and there is heavy bleeding, oxygen does not properly reach the nerve endings, and as a result, numbness occurs.
- When injecting into a diseased tooth, it is possible that the needle may enter the alveolar nerve. In this situation, the sensitivity of the tongue, chin and lips is not lost much; it only takes a few days to recover.
Symptoms of paresthesia can last a couple of days or several months, rarely more than a year. Numbness that does not go away over a long period of time is called chronic paresthesia. If this diagnosis is protracted, the patient is prescribed treatment:
- Drugs are prescribed to reduce blood viscosity and establish normal blood circulation, injections intramuscularly, intravenously.
- Physiotherapeutic procedures are carried out: UHF, mud treatment, electrophoresis, diadynamic currents, magnetic therapy.
- In the absence of positive results, they resort to surgical treatment, but such cases are rare.
If during therapy the patient continues to complain of a lack of sensitivity, he is additionally examined by a neurophysiologist and the type of neuropathy is determined based on electroneuromyography.
Professional surgeons – dentists, as a rule, are specialists in their field. They have excellent knowledge of anatomy, have an excellent understanding of the complex structure of the lower jaw canal, plus vast practical experience. Therefore, if wisdom tooth removal is prescribed according to indications, you should not delay it. Experienced, attentive dentists will definitely conduct a preliminary consultation with the patient before removal in order to dispel all his fears and doubts and prevent serious mistakes during treatment.
Back
The jaw hurts and clicks after prosthetics or dental treatment
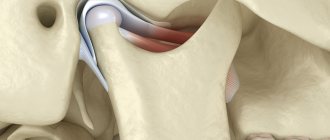
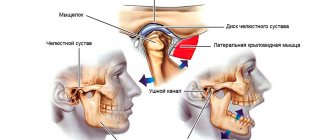
Dysfunction of the temporomandibular joint. The lower jaw is connected to the skull by two temporomandibular joints. Impairment of the function of these joints is possible after the installation of a denture, crown, bridge, any treatment or tooth extraction if this leads to malocclusion and/or damage to the temporomandibular joint. This is a typical complication after dental prosthetics. Read more about treating TMJ dysfunction here
Temporomandibular joint dysfunction
The green arrow indicates a healthy joint. The red arrow points to the joint that remains in the “open” position when the mouth is closed. This leads to wear and tear of the articular cartilage, pain and clicking when opening and closing the mouth. One of the reasons is the incorrect position of the upper right “eight” (tooth 1_8 lies horizontally).
How can we help you:
- Anti-inflammatory treatment will help relieve pain. If necessary, we inject anti-inflammatory medication directly into the lower jaw joint . This brings relief within a few minutes .
- Injection of botulinum toxin preparations (for example, Botox or Dysport) into spasmodic muscles. This is relevant in the case of an excessive increase in the tone of the masticatory muscles, if it is the muscles that are the “culprit” of dysfunction of the temporomandibular joint.
- Treatment by an osteopath. An osteopath works with the joints and muscles of the jaw using gentle manual techniques. This way you can solve a lot of problems that cannot be solved in classical dentistry. More about osteopathy
- Introduction of chondroprotectors (medicines for nutrition and restoration of cartilage) into the temporomandibular joint. Read more about cartilage restoration
Possible complications
The human factor plays a huge role in all dental procedures, including the administration of anesthetic.
Complications that may occur after local anesthesia:
- Unpleasant sensations in the injection area. Injecting the medicine too quickly or too slowly may cause pain.
- Hematoma at the site of needle insertion. The formation of a hematoma indicates problems with blood vessels or that the injection site was chosen incorrectly.
- Allergy. An allergic reaction to one or even several components of an anesthetic.
- Inflammatory process, development of infection. This is possible if errors were made during the administration of the anesthetic, due to which microbes penetrated the soft periodontal tissues and caused inflammation.
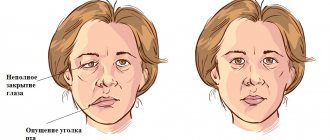
- Numbness of the facial muscles. The patient cannot control his facial expressions and cannot close his lips.
Sinusitis, maxillary sinus cyst, loss of sense of smell after visiting the dentist
The roots of the teeth of the upper jaw can normally be adjacent to the maxillary (maxillary) sinuses of the nose and even survive in them . Sinusitis, maxillary sinus cyst and loss of smell are possible when infection or filling material penetrates from the teeth into the paranasal sinuses. Unfortunately, this is not uncommon. Moreover, some cases of persistently recurrent sinusitis are associated with infection penetrating from the roots of the teeth . In this case, a possible symptom is a strong unpleasant odor from the nose and mouth.
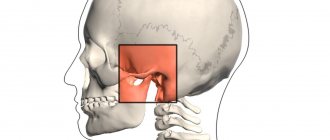
Odontogenic sinusitis after treatment by a dentist
Odontogenic sinusitis (scheme). Teeth and maxillary sinus. On the left is the norm. On the right – the root of the “seven” (tooth 2_7) is destroyed, inflammation around the destroyed root, pus in the maxillary sinus.
Filling material in the maxillary sinus and sinusitis after filling the “six” canals (tooth 2_6). Pain in the left side of the face after visiting the dentist.
1 – roots of teeth, 2 – normal, air in the right maxillary sinus (front view, the air looks black in the picture), 3 – in the left maxillary sinus there is a fragment of filling material surrounded by an inflammatory shaft. The patient had been mistakenly receiving treatment for trigeminal neuralgia for a long time.
Cysts of the maxillary (maxillary) sinuses in diseases of the roots of the teeth.
1 – roots of the teeth, 2 – cysts of the maxillary sinuses, growing from the roots of the teeth (cysts are round “bubbles”, they look gray in the picture).
How can we help you:
- Let's find the source of pain after dental treatment;
- We will treat inflammatory processes, sinusitis, sinusitis and neurological complications; if necessary, your health will be taken care of jointly by a neurologist and an ENT doctor. Treatment of sinusitis without puncture
Symptoms and causes of numbness after an injection
Numbness of the jaw after anesthesia is considered normal. But if it is accompanied by the following symptoms, you should seek the help of a doctor:
- numbness, burning or tingling of the tongue;
- numbness of the cheek;
- painful sensations in the tooth;
- sagging of the lower parts of the face;
- excessive salivation;
- pulsation in the gum.
Factors that influence the occurrence of symptoms:
- when injecting the anesthetic, the needle entered a blood vessel;
- a nerve was damaged during the injection;
- due to increased toxicity, the anesthetic itself caused numbness.
A little about the anatomy and course of the branches of the trigeminal nerve
The teeth of the upper and lower jaw are innervated by the branches of the trigeminal nerve, which provide all types of sensitivity directly to the teeth, skin and mucous membrane of the lips and cheeks. The lower jaw - by the mandibular nerve, the upper - by the alveolar branches of the maxillary nerve, forming the dental plexus.
The alveolar branches of the maxillary nerve pass along the wall of the maxillary sinus to the apexes of the roots of the upper teeth, where they form a nerve plexus responsible for the sensitivity of the upper teeth and gums. The mandibular nerve passes through the bone canal of the same name, innervating the lower teeth and gums, lower lip, and part of the cheek.
Types of pain relief
There are three types of anesthesia in dental practice:
- Local – anesthesia of the oral cavity using a syringe and an anesthetic. This type of anesthesia is used most often. Local anesthesia is performed in several ways depending on the indications.
- Sedation is a superficial depression of consciousness using mild sedative intravenous drugs. Sedation puts the patient into a state of sleep, eliminates fear and anxiety, and allows treatment to be carried out in a comfortable environment for the patient and the doctor.
- General anesthesia is anesthesia that involves influencing the central nervous system. In clinical practice, anesthesia is used quite rarely. It is used in cases where treatment with other methods of pain relief is impossible.
Local anesthesia provides pain relief to the teeth, gums, jaws and soft tissues of the mouth. It comes in several types depending on the methodology:
- Conduction – anesthesia of large nerve endings at the points where the nerve exits the bone. It is used when necessary to numb the entire jaw or part of it. This type of anesthesia is used during surgical operations, implantation, and tooth extraction.
- Intraosseous – injection of an anesthetic into the bone tissue of the jaw. It is performed more often for additional pain relief at the intervention site.
- Infiltration – gradual introduction of an anesthetic solution into the soft tissues of the maxillofacial area. First, the drug is injected under the mucous membrane, then into the deeper layers of tissue. The anesthesia acts quickly, is easy to administer, and can be injected if necessary.
- Intraligamentary – injection of an anesthetic into the tooth ligament and periodontal fissure. It is used to numb one tooth using a special syringe.
- Application – superficial anesthesia of the mucous membrane using cream, gel, spray. Most often used in pediatric dentistry. It can be performed before anesthesia using a syringe to eliminate pain during injection.
How long should it take to freeze?
How long does anesthesia last after tooth extraction? The duration of the effect depends on several factors:
- The type and amount of pain medication administered;
- Type of anesthesia, injection depth, injection site;
- The presence of a vasoconstrictor in the drug (substances that constrict blood vessels and prolong pain relief);
- Human weight, individual parameters;
- Features of metabolism;
- The presence of chronic diseases of the urinary system.
Conduction anesthesia lasts 2-3 hours on the upper jaw and 3-5 hours on the lower jaw. Therefore, the pain relief effect may persist for several hours after visiting the doctor. Other types of local anesthesia have a shorter period of action - from 15 minutes to 2 hours.
Computer anesthesia
In order to eliminate the possibility of developing complications after an injection, modern dentistry uses computer anesthesia.
Advantages of the technique:
- There is no numbness of soft tissues. Computer anesthesia only numbs the area where the anesthetic is injected.
- Computer anesthesia is painless.
- The pressure of the anesthetic is controlled by a computer, so it is administered at the desired speed and in smaller quantities.
- There is no feeling of gum swelling.
- The influence of the human factor is eliminated due to the fact that the computer controls the entire process.
- The tip is shaped like a pen, which is less intimidating for patients who are afraid of injections.
What to do, how to treat
Treatment of paresthesia due to unsuccessful implantation can be prescribed by the implantologist who performed the operation, dentist, neurologist, or physiotherapist.
Before moving on to restorative therapy, a diagnosis must be carried out, during which the nature and extent of the damage is established. The treatment is carried out comprehensively, aimed at restoring the conductivity and sensitivity of nerve fibers .
If the patient consults a doctor immediately, drug therapy in combination with physiotherapeutic procedures is very effective. In other cases, surgery is required.