An abnormality such as bone spurs is often ignored until it actively progresses. Patients often come to the clinic late, which entails complex treatment, including surgery. Exostosis is a pathology in which hardened areas of cartilage tissue protrude above the jaw are formed. The causes of this phenomenon are mechanical damage, trauma, tooth extraction and other diseases. Chewing functions are preserved, and soft tissues are also not damaged. But as the protrusions grow, thinning of the mucous membrane and ruptures occur, causing injury to surrounding areas.
Causes
Reasons for the formation of growths:
- inflammatory, infectious processes, purulent accumulations;
- mechanical impacts, injuries causing bone destruction, jaw displacement and other damage;
- deviations of row segments, formation of nodular hardenings;
- disorders of the endocrine system, hormonal levels.
One of the reasons for the development of pathology is complex tooth extraction. Often, when a wound heals, the tissue around it becomes overgrown with moving areas. If done incorrectly, compactions may appear and exostosis will gradually develop.
General idea of exostosis in the mouth
New growths on bone tissue are found in different parts of the body. Exostosis in dentistry according to ICD-10 refers to other specified diseases of the jaw K-10.8. The osteochondral formations look like a protrusion, lump, mushroom or ridge, and can branch and be tortuous. When they grow, they injure the mucous membranes of the mouth, which provokes the development of inflammation.
Zkzostoza on the upper jaw are less common than in the mandibular region. Usually formed on the alveolar process on the side of the cheek. When the size increases, they affect the aesthetics of the face, creating asymmetry. In the lower jaw, exostosis often forms on the lingual side. Protrusions can interfere with chewing food and talking.
You can see what exostosis looks like on the gum or bottom of the lower jaw in the photo. If the formation is small, then it is difficult to notice it visually.
Symptoms
The initial stage of the pathology practically does not manifest itself. Symptoms generally have a vague picture, which is why patients rarely see a doctor in a timely manner. But as the condition worsens, the following symptoms appear:
- growths with a pronounced convex shape appear on the tissues; the structure can be embossed or smooth;
- there is a feeling of a foreign object in the mouth;
- pain appears, sometimes quite severe;
- partial jaw dysfunction is observed;
- the shade of the mucous membrane changes to bright;
- capillary obstruction appears in the area of the growth.
How is the operation performed?
Like the operation to remove exostosis on the leg, there are also 4 main stages in dentistry.
- Pain relief in the mouth using local anesthesia.
- The surgeon makes a careful incision on the gum.
- The build-up is removed using a drill or laser, and the remaining surface is carefully sanded.
- The gum returns to its original place, the specialist applies stitches. To make the removal of exostosis of the lower jaw more effective and the bone to recover faster, it is possible to apply artificial bone.
As a rule, removal of exostosis of the upper jaw, as well as the lower one, takes place without any complications or problems. It is important to follow all the specialist’s recommendations during the rehabilitation period and provide proper care. In particular, limit your diet to soft foods, no alcoholic beverages, taking medication (prescribed by a doctor), treating the oral cavity with antiseptic drugs, etc.
A healthy and beautiful smile is simple. Even if this requires manipulation to remove the root of a tooth, exostosis, the hood of a wisdom tooth (or the tooth itself) or anything else, over time you will see that it was worth it in every sense. And the specialists of the Priority clinic are always ready to try their best for you.
Indications and contraindications
The growth is treated surgically. Indications for using this option for removing pathology are:
- the bone growth grows quickly;
- pronounced cosmetic changes, progression of pathology;
- physical discomfort, the growth becomes too large;
- before prosthetics.
There are a number of the following contraindications to surgical intervention:
- pathologies of the endocrine system;
- adrenal dysfunction;
- diabetes of any form;
- bleeding disorders.
Treatment
Before treatment, the doctor conducts an examination and prescribes a number of diagnostic measures. It is necessary to perform fluoroscopy, determine the level of blood clotting, and determine whether there are contraindications to surgery. If there are no contraindications, the doctor removes the growth:
- anesthesia is performed (for uncomplicated pathology, the operation is performed under local anesthesia);
- the oral cavity is treated with antiseptic drugs;
- an incision is made on the gum, then the mucosal tissue is dissected to open access to the bone;
- the growth is removed using a laser beam or chisel (depending on the state of the pathology);
- the bone tissue is smoothed to an even texture, at which time cooled water is supplied to the surface;
- The tissues are sewn together and a bandage is applied.
The duration of the procedure depends on the complexity of the treatment. For mild cases, the operation takes about forty minutes; for complex pathologies, removal may take an hour and a half.
During the recovery period, the patient must follow the doctor's recommendations. For the first day, the intake of food and solid foods is limited, smoking and drinking alcohol are excluded. It is necessary to avoid physical activity, which can provoke bleeding and cause swelling.
Why remove exostosis?
Exostoses, as a rule, do not hurt or cause discomfort. Most often they form in children under the age of 20 during the formation of the skeleton and bone tissue, however, pathology also occurs in adults.
It is necessary to remove bone growths for several reasons:
- violation of aesthetics: exostoses look like white balls on the gums, which are noticeable when smiling,
- growths often increase in size,
- possible transition to a malignant form,
- if it is necessary to install implants or prostheses, exostoses will become an obstacle to the procedure, since the prostheses will injure the growths, and the implants simply cannot be fixed due to a violation of the quality of the bone tissue.
Diagnosis of the disease
Expert opinion
Vasiliev Alexander Alexandrovich Implant surgeon Work experience 10+
“Exostoses do not always have external manifestations - often they can only be detected on photographs when diagnosing other diseases. However, the examination uses an x-ray - a targeted image of one tooth. Or, more effectively, an orthopantomogram. It allows us to examine the condition of the jaw bone and tooth roots along the entire row, because growths are often formed in multiple quantities.”
Types of tumor
A tumor on the roof of the mouth always indicates the onset of an inflammatory process in the human body. Tumors can be benign or malignant.
Malignant formation
Problems with the development of a malignant tumor are not limited to disturbances in speaking and eating. The lump, the cause of which is cancer, impairs articulation, complicates the ability to communicate or completely eliminates it.
Oral cancer is typical for men and is a local metastasis of other malignant tumors in the head. It is a rare cancer.
Such malignant lumps are classified as growths on the roof of the mouth. The tubercle can pop up due to a benign inflammatory process, so it is impossible to express a clear opinion about the diagnosis.
Understanding the reasons for the appearance of a tumor is important for determining the course of treatment. The causes can be accurately diagnosed by conducting clinical studies of the compaction.
Benign formation
A cyst on the roof of the mouth is not a fatal diagnosis; it is diagnosed with a number of benign tumors. Such tubercles are caused by insidious but curable diseases:
- growth of blood vessel tissue (angioma);
- cyst;
- pemphigus (erosion);
- myxoma.
Rehabilitation after removal of exostosis
The wound heals completely in about 1 week. For better tissue healing and prevention of complications, it is necessary to comply with the doctor’s requirements.
During the recovery period, you should not exercise or overheat the body. It is prohibited to visit the bathhouse, sunbathe on the beach, or take a hot bath. Otherwise, bleeding from the wound may occur.
In order not to injure the damaged mucous membrane, you should not eat rough, spicy or sour foods. Food should be liquid or pureed, at a comfortable temperature. It is undesirable to smoke, as nicotine constricts blood vessels, which prevents rapid healing.
When brushing your teeth, you should avoid the operated area. The toothbrush should be soft. After eating, you should rinse your mouth with warm water. Daily rinsing with antiseptic solutions, for example, chlorhexidine, miramistin, is recommended. For these purposes, you can prepare decoctions of chamomile, sage, calendula, and oak bark.
In the first few days, pain and swelling of the tissues persist. To relieve acute pain, you can take analgesics. A cold compress will help relieve swelling. Ice or frozen product is wrapped in plastic wrap, cloth and applied to the cheek several times a day.
If the patient is in poor health or has chronic diseases, the doctor may prescribe antibiotics.
If you ignore the dentist’s requirements, complications may occur: infection and inflammation of the wound, bleeding, suture dehiscence.
Features of the appearance of bumps on the gums
The formation of a lump on the gum occurs as a result of the development of a pathological process, the cause of which may be a non-infectious or infectious process. In most cases, the formation is a “bag” of pus, but compaction from periodontal tissue cannot be ruled out.
A lump on the gum can be caused by pathogenic bacteria (infectious origin) or tissue trauma (non-infectious). The pathological process is also distinguished by the nature of its course: chronic and acute.
Mostly, an acute form of pathology initially develops with the manifestation of pain and signs of inflammation. If left untreated, the formation can lead to complications or become chronic with periodic relapses. Treatment for a chronic gum lump may require surgery.
Prerequisites for the occurrence of a lump
Modern medicine has not created a complete list of reasons why bumps may appear. Doctors' reasoning is based on hypothetical cause-and-effect relationships. The appearance of a lump on the palate is caused by:
- Bad habits (smoking, alcohol, oral drugs);
- The presence of micro and macro injuries to the oral cavity (surgeries, scratches of the upper parts of the oral cavity);
- Availability of dentures;
- Viral infections;
- Intrauterine disorders (hemangioma is a congenital disease and acquired from the mother);
- Violation of the activity and integrity of the mucous membrane (typical of angina);
- Congenital and acquired dysfunction of the glands (the main cause of cysts).
There are two more hypothetical reasons for the appearance of malignant tumors:
- Eating too hot and spicy foods, constantly disrupting the structure of the cells of the oral cavity;
- The presence of papillomatosis or leukoplakia - diseases that are precancerous lumps that can develop into an oncological disease.
What to do if exostosis occurs after tooth extraction
Osteocartilaginous formations in the mouth can only be treated surgically, so if you suspect a pathology, you should consult a dentist. The doctor makes an accurate diagnosis after examining the patient: visual examination and radiography. Differential diagnosis of the nature of the lumps may be required.
Exostosis itself does not disappear, so the doctor decides whether the growth needs to be removed. If the protrusions are small, then the operation can be postponed indefinitely. In this case, you need to undergo regular examination at a dental clinic to monitor changes in tissues.
Tumors of bone tissue
Small bone growths that appear as a result of the hypertrophic process are called osteophytes.
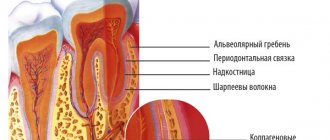
They are produced by the inner layer of the periosteum and upon examination are determined in the form of awl-shaped protrusions in various parts of the lower and upper jaw. A larger growth that rises above the surface of the bone is called exostosis. Osteophytes and exostoses consist, at the beginning of their development, of delicate bone crossbars with wide medullary spaces, with a large number of blood vessels. Subsequently, they become more compact, sclerosed and remain stable. They usually arise as a result of injury or productive inflammation.
Congenital spine-like bone formations are found on the lower jaw on the lingual side, corresponding to the location of the canine and the first small molar. More often they are symmetrical, that is, they are located on both sides, and resemble a small spur of a rooster. Sometimes they have an oval shape, resembling a swelling of the bone during canine impaction. They are usually discovered by a doctor during an examination of the oral cavity. The need to remove them arises only in cases where it is difficult to manufacture a denture for the lower jaw.
Congenital bone formations also include a bony protrusion along the midline in the area of the bony suture of the hard palate - torus palatinus.
Surgical interventions are not required even with prosthetics (Fig. 212).
Osteoma is a true tumor. Although they grow very slowly, osteomas sometimes reach significant sizes.
The starting point for osteoma growth is considered to be both endosteum and periosteum.
Growing intraosseously, osteoma remains invisible for a long time and only when it reaches a significant size does it attract attention. Like other parts of the skeleton, the maxillofacial bones are affected by osteoma (relatively rare. The tumor grows painlessly. In some localizations, osteoma can cause functional disorders. Thus, a 27-year-old patient came to our clinic about an increasing limitation in mouth opening. The cause of this turned out to be osteoma of the coronoid process, which, when opening the mouth, rested on the zygomatic arch. In another case, the osteoma was located on the articular process of the lower jaw (Fig. 213).
In a 20-year-old patient, osteoma of the upper jaw occupied the nasal cavity and impaired nasal breathing (Fig. 214). A small osteoma in patient K, located in the body of the lower jaw, compressed the alveolar nerve and caused paresthesia in the corresponding half of the lower lip and chin (Fig. 214a). In a 27-year-old man, the tumor occupied the right half of the upper jaw and extended to the main bone. In a 47-year-old woman, osteoma occupied the right styloid process.
According to their structure, osteomas are divided into:
- 1) compact (osteoma eburneum s. compactum), which consist of cortical bone with a complete absence of bone marrow and an almost complete absence of Haversian canals;
- 2) spongy (osteoma spongiosum), consisting of a porous, spongy substance;
- 3) soft (osteoma medullare) with wide bone marrow cavities.
Compact osteomas are easily diagnosed using x-rays. They are projected as denser formations than bone with defined edges. Other types of osteomas must be differentiated from fibrous osteodystrophy and adamantinoma. In this case, on radiographs you should pay attention to the more massive (contrasting) peripheral areas of the tumor. The closer to the center of the tumor, the less noticeable the difference in the structure of the tumor and the bone on which it is located becomes.
In terms of its microscopic structure, osteoma generally resembles normal bone tissue. The size of the medullary spaces and the number of Haversian canals vary depending on the type of osteoma. The presence of cartilaginous processes in the spongy bone is sometimes noted.
Treatment. Treatment is surgical. Radical excision of the tumor is performed within healthy bone tissue.
Indications for surgery are dysfunction (of a joint, nose, etc.) or pain, the presence of disfigurement, and the impossibility of prosthetics.
Why should jaw osteophytes be removed?
A bone growth on the gum is not dangerous until it begins to grow. Increasing in volume, the osteophyte puts pressure on the dentition and bone structures. This leads to tooth displacement, malocclusion, and jaw deformation. Large growths impede the movements of the tongue, complicate diction, and interfere with normal chewing of food. Large growths prevent prosthetics and implantation. Osteophyte of the jaw will not disappear on its own. The only effective method of treatment is surgical removal of the pathological formation.
Diagnostic methods
To determine the method by which a lump on the roof of the mouth will be treated, the causes of its occurrence are studied. The diagnostic procedure is carried out by a dentist.
Regular visits to the dentist are important to prevent the disease and determine whether a lump has appeared on the roof of your mouth. It needs to be treated at an early stage.
For diagnosis use:
- Radiography;
- Biopsy;
- Blood analysis;
- Radioisotope study;
- Ultrasound.
If you comprehensively examine the ball on the roof of your mouth, this will confirm or deny the presence of a malignant formation, and if it is absent, it will determine the exact diagnosis of a benign one.
Possible complications after surgical treatment
Complications after surgery often arise due to the fault of the patients themselves. Problems usually appear as a result of non-compliance with doctor's recommendations and hygiene rules. Among the possible undesirable scenarios, the following processes and phenomena are distinguished:
- suture divergence due to too intense chewing load or trauma to the causative area with solid food products,
- the development of an inflammatory process, accompanied by swelling of the mucous membrane and even purulent processes. Most often, the cause is unsatisfactory care of the wound and the oral cavity in general.
If such complications occur, it is important to see a doctor as soon as possible. Otherwise, ignoring problems will lead to even more serious consequences.
Exostosis in dentistry - bone tumor in the oral cavity and technology for its removal
The appearance of atypical neoplasms in the oral cavity is a phenomenon that never happens without a reason. Most often, the cause of such troubles is injury or dental disease. One of the possible scenarios is the appearance of a bone growth - exostosis. Despite the fact that in most cases the defect can be easily detected by touch, most patients seek help at an advanced stage. Further in this article we will talk about what it is - tooth exostosis, in what cases it usually appears and how the procedure for its removal is carried out.
Classification of fibroids
Pathology is divided into several types according to criteria. This includes the density of the benign neoplasm, the nature of its origin, as well as the severity of clinical manifestations.
Dense fibroma
Characterized by a solid consistency. This is due to the fact that the contents are quite hard fibers of connective tissue. They include a small number of cores. Formations of this type are most often found on the gingival surfaces and palate.
Soft fibroma
The fibrous structures are thin and freely located, so their clusters are characterized by a high degree of softness. This type is most often observed on the tongue and the inside of both cheeks. Benign neoplasms of a mixed type, combining the signs of all the varieties listed above, can be found on the sublingual part and on the mucous membranes of the floor of the oral cavity. For example it could be:
- Fibrolipoma. It is hard to the touch because it contains fibrous fibers. It can be eliminated surgically, with laser, or radio waves.
- Fibrohemangioma. As a rule, it is provoked by infectious processes occurring in the child’s body. It is extremely rare in adults. It never degenerates into malignant tumors. Most often it is treated surgically, in some cases it can resolve on its own.
Fibroma from irritation
This is not a tumor formation in its usual form, but the result of reactive hyperplasia. Chronic pathology is characterized by the development of focal lesions, which are caused by systematic mechanical action and subsequent injury.
The most common cause is installed crowns, fillings, and dentures. In the latter case, the disease is called prosthetic granuloma. The orthopedic structure exerts continuous pressure on the alveolar process, leads to its resorption, moves forward and contributes to the formation of compactions, which are associated with the inflammatory process.
The risk group includes not only patients who have undergone prosthetics, but also people with untimely cured caries, in adulthood, with foreign objects in the oral cavity (for example, with piercings). Studies have shown that women are more prone to such hypertrophic transformations than men.
Symmetrical fibromas
Doctors diagnose such tumors in the area of the third molars in the areas between the gums and the roof of the mouth. The tumor is hard to the touch and resembles a bean in shape.
It should be noted that this type of compaction does not apply to true fibromatosis. These are just overgrown tissues in the gingival membranes, accompanied by the process of scarring and other changes of a similar nature.
Lobular fibroma
It occurs as a result of reactive hyperplasia with systematic trauma to delicate sensory fibers with prostheses or other orthopedic structures. The main distinguishing feature of such formations is their rough, textured surface. When palpated, tubercles are felt.
Fibrous epulis
This is a dense growth of pinkish tissue that does not cause pain or other discomfort. The edges are often hyperemic, have clear boundaries and irregular shape. The base is quite wide.
The vestibular part of the gums is usually affected. There are cases of neoplasms occurring in the interdental spaces in the form of a saddle with spread to the intraoral surface.
Quite often, a dental unit located in a pathological area has a poorly fitted metal crown, extensive carious lesions, or a prosthetic clasp. It is these structures that are the provoking factor in the occurrence of a chronic inflammatory process with the formation of granules, which over time are transformed into mature connective fibrous fibers.
In dentistry, there are also angiomatous epulis. They are brighter in color, somewhat softer to the touch and bleed. In this case, blood appears not only at those moments when the surface is affected mechanically, but regardless of the presence or absence of a traumatic factor. When conducting diagnostic studies, many vascular branches are detected in the pathological area.
Signs
The main symptom is the presence of a dense tubercle near the place where the tooth was removed. At first it does not manifest itself in any way, except that it disturbs a little in the mouth, but again this depends on the location of the compaction. The lump is growing very quickly. When the maximum size is reached, the following signs are present:
- Aching pain that intensifies when eating.
- The cone takes on a bright scarlet hue.
- At maximum sizes, it interferes with the normal position of the tongue.
Prevention Tips
It is impossible to avoid such a problem with a guarantee, but it is possible to significantly reduce the risk of its occurrence or identify a defect at the initial stage of its formation. To do this, you need to be careful about the condition of the oral cavity, carefully monitor hygiene, do not skip preventive examinations, eliminate traumatic factors if possible and do not trigger dental pathologies - start treatment on time.
Preventive examinations will help to recognize the problem in time
Experts also recommend systematically conducting self-diagnosis - from time to time carefully examining the tissues of the oral cavity for abnormal neoplasms. This should only be done with clean hands, carefully feeling every part of the jaw apparatus, including the palatal area. If you detect a suspicious growth, you should seek help from a dentist as soon as possible.