Effective treatment of stomatitis in adults
Treatment of stomatitis in adults largely depends on the type of this disease, as well as concomitant diseases that provoke the appearance of ulcers and inflammation in the mouth. The most interesting thing is that the diagnosis of stomatitis is still carried out visually: the patient undergoes tests only if other, more serious diseases are suspected. Effective therapy for stomatitis is possible, but only if the type of disease is correctly determined. Recovery usually occurs within one or several weeks, but there are also more severe forms when long-term rehabilitation is required for complete recovery. Let's look at the main types of disease and drugs for the treatment of stomatitis in adults.
Why does the disease occur?
Stomatitis can be an independent disease or a symptom of systemic diseases. Immunodeficiency, pemphigus, streptoderma - all these are pathologies that create conditions for its development. Mechanical damage, which is possible if there are sharp dental crowns or low-quality dentures in the mouth, also lead to irritation of the mucous membranes.
Dentists agree that the disease occurs due to:
- failure to comply with oral hygiene rules;
- habits of chewing hard foreign objects;
- improper installation of braces, dental bridges, crowns;
- long-term use of certain medications;
- smoking;
- using drugs by placing them under the tongue or “behind the lip”;
- unbalanced nutrition, progressive vitamin deficiency;
- malignant tumors located in the mouth;
- prolonged stress;
- hormonal disorders.
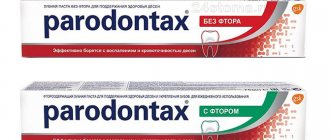
Today it has been proven that the need to use drugs to treat stomatitis often arises in people who are accustomed to using toothpaste that contains sodium lauryl sulfate. This is a compound that promotes the formation of thick foam during hygiene measures. It has been established that sodium lauryl sulfate “pulls” moisture from the mucous membranes of the mouth , as a result of which they become more sensitive to negative external influences. Therefore, when purchasing a hygiene product, it is important to study its composition.
Treatment of herpetic stomatitis
Treatment of stomatitis after detection can be carried out many times (once a year or more often), since once settled in our body, the herpes virus remains there for life. Herpes stomatitis is characterized by the accumulation of reddish transparent blisters on the lips and inside the mouth, so it is quite easy to detect. Especially often, herpetic stomatitis manifests itself against the background of decreased immunity, vitamin deficiency, hypothermia and stress. Remember that herpetic stomatitis in adults is contagious, so you should avoid tactile contact.
Types of drugs
- Antiviral agents.
- Immunostimulants (as a preventative measure).
- Ointments (including to eliminate visual manifestations of the disease).
Frequent stomatitis. How to quickly cure stomatitis
Go back
Stomatitis is an inflammatory disease of the oral mucosa. Persistent stomatitis, regardless of the cause, indicates a decrease in immunity and, as a result, the development of inflammation.
Symptoms of stomatitis
Pain, burning, mouth ulcers, swelling of the tongue and lips, as well as other parts of the oral mucosa, are the most common symptoms of stomatitis. Pain with stomatitis can occur both when eating or talking, and at rest with severe inflammatory changes in the oral mucosa. Advanced or long-term untreated stomatitis can affect most of the oral mucosa. In such a situation, patients with stomatitis are hospitalized.
Cause of stomatitis
The oral mucosa is the body's first barrier when encountering an infection.
Whether we eat or drink water, talk or breathe, every time a large number of different microbes rush into our body through the mouth. Often the causes of stomatitis in adults and children come down to poor hygiene and lack of adequate oral care. One of the most common causes of stomatitis is infection. Moreover, this group can include bacteria, viruses, and fungi. How ORALSEPT helps ORALSEPT® affects the cause of inflammation (bacteria and fungi) and relieves the symptoms of inflammation.
Read more
Frequent stomatitis in adults. Causes There are many causes of stomatitis, which occurs several times during the year. As a rule, repeated episodes of stomatitis develop against the background of disruption of both local and general immunity.
The main causes of stomatitis are:
- Diseases of the gastrointestinal tract
- Intestinal infections
- Smoking
- Drinking alcohol and hot drinks
- Eating food with lots of spices
- Diabetes
- Acquired immunodeficiency syndrome (AIDS)
- Radiation therapy in the treatment of cancer
And this is not a complete list of factors leading to the development of stomatitis.
Frequent stomatitis in a child. Reasons “Don’t put it in your mouth” is one of the most common comments to a child. Children try to learn everything new by tasting it. This is how the infectious agent enters the oral cavity. Stomatitis in children can be a manifestation of both an independent disease - for example, herpes, and a symptom of other infections. Stomatitis often occurs with measles (Filatov's spots) and enterovirus infection, with chicken pox and other diseases. Also, stomatitis in children can often be a manifestation of an allergic reaction or the result of an intestinal infection. The first place among the infectious causes of stomatitis in children is occupied by herpetic and candidal stomatitis.
Herpetic stomatitis in children is characterized by severely painful ulcers in the mouth. The first episode of herpetic stomatitis can last quite a long time, up to 2-3 weeks, until the body forms protective antibodies to the virus. Children refuse to eat due to pain. The disease manifests itself not only with local symptoms, but also with general ones, such as weakness, fever, headache, nausea.
Candidal stomatitis in children can appear literally in the first months of life. With candidal stomatitis, a white, loose (curdled) coating appears on the oral mucosa. Beneath it, a red, swollen, inflamed mucous membrane is visible. The cause of candidal stomatitis is a decrease in immunity and a fungal infection (fungus of the Candida species), which, as a rule, develops due to disturbances in the gastrointestinal tract or food allergies. Infants with candidal stomatitis are very restless, often cry, and quickly lose weight.
How to quickly cure stomatitis The main complaint with stomatitis is pain. And therefore, first of all, drugs that reduce pain and have an anti-inflammatory effect are prescribed. These may be non-steroidal anti-inflammatory drugs, local anesthetics. It is also necessary to prescribe antimicrobial drugs that act on the main cause of stomatitis - infection.
How to quickly cure stomatitis in a child
To quickly relieve pain and inflammation during stomatitis, local remedies are used. But children often do not know how to rinse their mouths, and due to pain they may react negatively to the use of oral medications. In such a situation, using a topical treatment spray will help.
How to quickly cure stomatitis in an adult
Stomatitis in adults often affects general well-being.
In addition, people whose professional activities involve the active use of speech cannot fully perform their work when stomatitis occurs. In such a situation, either a temporary refusal to work for treatment or the use of drugs that quickly relieve pain and inflammation, and which can be taken with you and used on the go, is required. Remedy for stomatitis – what to choose? More recently, when treating stomatitis, doctors prescribed several drugs at the same time: for pain, inflammation, anti-infectives. It was a set consisting of gels, rinses, tablets for oral administration and topical use. Currently, in the treatment of stomatitis, agents are used that act directly on the site of inflammation and have a complex effect. Oralcept spray in such a situation is the best option. Acting locally on the source of inflammation, it quickly, within a minute*, reduces pain and reduces the inflammatory manifestations of stomatitis. In addition, it has a local antiseptic effect and fights bacterial and fungal infections. Oralcept has a pleasant, delicate mint taste. The compact plastic bottle of the drug with a special nozzle is convenient to carry with you.
*WITH. Simon-Savois, D. Forest. - "Local anesthetic activity of benzydamine", Modern Therapeutic Research, Vol. 23, No. 6, June 1978, Department of Dentistry, University of Montreal, Montreal, Canada
Treatment of candidal stomatitis
A type of stomatitis that is caused by a special type of fungus – Candida albicans. Very often, candidal stomatitis begins with glossitis, which is why its second name is stomatitis on the tongue. Treatment in this case requires fairly prompt treatment, since in adults it is quite painful and is accompanied by a burning sensation in the mucous membrane and sore throat. On the inner surface of the lips and cheeks, as well as on the tongue, characteristic foci of inflammation appear, covered with a white cheesy coating.
Treatment methods
- Treatment of common diseases (if detected).
- Antimicrobial therapy.
- Preventive rinses.
Traumatic stomatitis
Inflammation of the mucous membrane in the mouth can be preceded by trauma: mechanical, thermal, chemical, radiation1,6.
Small children who put everything in their mouths can injure the mucous membranes with the sharp edges of toys or household items. Injuries often occur due to inept use of cutlery as a result of falls. In older children, stomatitis may be associated with a thermal burn, blows to the teeth, or the bad habit of chewing a pencil or pen. Sometimes the cause of inflammation is dental diseases and their treatment: sharp edges of damaged teeth and fillings, braces and aligners1.
When stomatitis develops in a child on the gum, on the inner surface of the cheek or in another place, the mucous membrane becomes red and swollen, and a painful erosion or ulcer may appear in the area of damage. Since there are many microorganisms in the mouth, there is always a risk of a bacterial or fungal infection1.
If the mucous membrane is constantly injured, painless whitish or whitish-gray layers may form on it.
In children under 1 year of age, stomatitis can be the result of using the wrong nipples: long, tight, irregularly shaped. The resulting Bednar aphthae are located in the area of the transition of the soft palate to the hard palate and are round erosions or ulcers1.
Treatment of traumatic stomatitis in children includes:
- elimination of traumatic factors;
- rinsing the mouth, irrigating the mucous membranes and treating wounds with drugs with an analgesic and antiseptic effect1.
Up to contents
Treatment of aphthous stomatitis
A distinctive feature of this type of stomatitis is the appearance of so-called aphthae on the oral mucosa. These are small round ulcers with redness at the edges, the touch of which causes unpleasant painful sensations. Often occurs as a result of the activity of microorganisms (in particular, staphylococcus). Treating aphthous stomatitis at home is only recommended if it is not caused by a more severe illness. Often aphthous stomatitis occurs with problems with the immune system, liver and gastrointestinal tract.
Treatment methods
- Allergy therapy.
- Antiseptic therapy (treatment of aphthae with anti-inflammatory solutions, gels and ointments).
- Dental treatment and sanitation of the oral cavity (after dental treatment, stomatitis occurs less frequently than in the presence of carious lesions).
- Immunotherapy.
- Diet.
Causes
The pathology is caused by numerous infectious agents, as well as oral injuries and allergic reactions. The reason for its development may be a lack of certain vitamins and microelements.
The following types are distinguished:
- viral (herpetic - present in 80% of all cases, the rest are represented by measles, chickenpox, influenza, rubella, mononucleosis, adenovirus, enterovirus, papillomavirus viruses);
- fungal – candidiasis is detected in the vast majority of cases in infants; in older children it occurs due to immunodeficiency, diabetes, or taking antibiotics;
- bacterial - most often it is caused by various types of staphylococci and streptococci; in rare cases, stomatitis is caused by pathogens of tuberculosis, syphilis, diphtheria, gonorrhea;
- allergic – often the pathology develops as a reaction to various products, components of toothpaste, chewing gum;
- autoimmune – in the occurrence of aphthous lesions, one of the leading causes is considered to be the presence of autoimmune problems;
- traumatic - in children, the oral mucosa is less stable than in adults; it is easily damaged under the influence of chemical and physical agents, or mechanical trauma.
The factor that caused this pathology determines the treatment tactics and what drugs will be prescribed.
There are factors that contribute to the development of the disease.
These include:
- diseases of the gastrointestinal tract (duodenitis, gastritis, intestinal dysbiosis, colitis, enteritis);
- blood diseases;
- pathologies of the nervous and endocrine systems;
- helminthiases;
- prematurity;
- insufficient oral hygiene;
- weak local immunity;
- lack of microelements, vitamins (B vitamins, selenium, zinc).
All these numerous factors cause and contribute to the development of stomatitis. In this regard, there is a significant difference in the treatment of different types of disease.
Treatment of ulcerative stomatitis
Ulcerative stomatitis very often occurs due to poor oral hygiene and bad habits (especially smoking). Often this type of stomatitis at its onset is confused with periodontitis and gingivitis, since it is characterized by inflammation of the gums, a grayish coating around the teeth and death of soft tissues. Often accompanied by fever and fever. One of the few forms of stomatitis, which often requires treatment by a doctor, and in the most advanced cases, surgical intervention.
Treatment methods
- Antibiotic therapy.
- Antibacterial treatment of affected areas.
- Surgical intervention (in severe cases, removal of areas of dead tissue and gum grafting).
Systemic pharmacological treatment –
Systemic therapy includes 3 types of drugs - antihistamines, glucocorticoids and immunomodulators. Antihistamines can and should be prescribed to absolutely all patients with aphthous stomatitis (without exception), the cause of which has not been precisely established. As for the drugs of the other 2 groups, they are the second line of defense, after which there are essentially no other treatment options.
1) Antihistamines –
Antihistamines will be an excellent addition to local therapy even for mild cases of aphthous stomatitis. The fact is that aphthous stomatitis can often be caused by unidentified food allergens (or components of hygiene products, for example, parabens). Therefore, it makes sense to start taking 2nd generation antihistamines orally for a course of 7-10 days.
Modern antihistamines are well tolerated and do not have significant side effects, therefore, given the difficulty of identifying the true cause of ulceration, you can start taking them from the first day of the disease, or even better - in the prodromal period, when ulcers have not yet formed, but the patient can already feel at the site of their future occurrence there is a slight burning or itching.
Table No. 1 (examples of 2nd generation antihistamines)
Means for nonspecific hyposensitization - for moderate and severe forms of aphthous stomatitis, when we need to quickly reduce the patient's body's sensitivity to allergens - in this case, the use of drugs for nonspecific hyposensitization is indicated. For example, these could be subcutaneous injections of histoglobulin - 2 ml 2 times a week with an interval of 2-3 days (a total of 10-12 injections per course). Or we can prescribe intravenously - a 30% solution of sodium thiosulfate, 10 ml daily, for a total of 6-8 injections for a course. These are all prescription drugs!
2) Systemic glucocorticoids –
These drugs are a second line of defense and are a lifesaver for patients with acute severe outbreaks of canker sores, but these drugs can only be used as directed by a doctor. Typically, prednisolone tablets are used in adults at an initial dose of 25 mg/day for the first 7 days (followed by a gradual dose reduction). The total duration of the course of therapy is usually 15 days, but in severe cases it can even reach 1-2 months.
However, in a clinical study by Pakfetrat et al. (source) – good results of treatment with prednisolone were achieved when used at a dosage of only 5 mg/day. Prednisolone is an extremely effective drug for the treatment of severe forms of aphthous stomatitis, but its dosage must be selected individually for each patient (taking into account the severity and severity of the disease, as well as the patient’s health condition). Be aware that prednisone may cause long-term side effects.
The search for alternative, safer drugs made it possible to find that the drug "Montelukast" (usually used as an anti-asthmatic drug) - at a dose of 10 mg per day, like prednisolone, reduced the number of lesions, relieved pain and accelerated the healing of ulcers, but at the same time it caused significantly fewer side effects (clinical study - Femiano et al.). It is important that Montelukast can be used even when systemic glucocorticoids are contraindicated.
3) Immunomodulators –
Immunomodulators are also a second line of defense, as are glucocorticoids. Their use is especially indicated in patients who are diagnosed with chronic recurrent aphthous stomatitis (with frequent relapses and an aggressive course of the disease). For children over 1 year of age, this could be, for example, in the form of Thymogen nasal spray, but keep in mind that this is a prescription drug.
For children over 3 years old, the over-the-counter drug “Likopid” 1 mg is suitable, which is taken 1 tablet 3 times a day, for a total of 10 days (for resorption under the tongue or orally). However, despite the over-the-counter availability of this drug, we, in principle, recommend taking drugs from the group of systemic immunomodulators - only after consulting an immunologist.
For adults - in adults, for immunocorrection with recurrent aphthous stomatitis, it is optimal to use either the drug "Timogen" (in the form of intramuscular injections of 100 mg daily for 10 days), or "Levamisole", which restores normal phagocytic activity among macrophages and neutrophils and modulates T-lymphocyte-mediated immunity. It is prescribed - 150 mg 3 times a week (for 6 months).
You can also use the drug "Methyluracil" (1 tablet 0.5 g - 3 times a day, for 1 month). For the most severe outbreaks of aphthous stomatitis, you can use Thalidomide at a dose of 50-100 mg/day, but keep in mind that although with the use of this drug 85% of patients experience complete remission of severe lesions (already in the first 14 days) - it has very strong side effects. Keep in mind that all of the above medications can only be used as prescribed by a doctor!
Both children and adults can also use the over-the-counter drug "Imudon", which is available in the form of tablets for resorption in the oral cavity. But this drug affects only the local immunity of the oral mucosa, without affecting the immune system as a whole. The course of treatment is 6-8 tablets per day for resorption (course duration is from 10 to 20 days - depending on the severity and frequency of relapses of aphthous stomatitis).
4) Means for restoring intestinal microflora –
We have already said above that there is a clear correlation between gastrointestinal diseases and repeated outbreaks of aphthous stomatitis, which is explained by the significant influence of intestinal pathology on the state of the immune system. Therefore, such patients are always advised to take medications (probiotics) that normalize the intestinal microflora. This could be Linex or Bifiform, as well as Hilak-Forte or other similar drugs.
Probiotic Bifiform –
Treatment of bacterial stomatitis
This type of stomatitis is also called prosthetic stomatitis, since it occurs due to unsatisfactory care of the orthopedic structure, when many pathogenic microorganisms accumulate in the area of contact between the prosthesis and soft tissues. After treating foci of inflammation, it is necessary to carry out complete cleaning and antibacterial treatment of the prosthesis or replace it. This type of stomatitis should not be confused with allergic stomatitis, which develops against the background of an allergy to the prosthetic material. In this case, the prosthesis must be changed to a hypoallergenic one.
Treatment methods
- Anti-infective therapy.
- Mouth rinse.
Treatment of allergic stomatitis
This type of stomatitis is caused by the body's immunological response to contact with an allergen. The role of the latter can be played by anything: food products, new oral hygiene products, dentures, animal hair and much more. At risk are patients who are predisposed to allergies or suffer from various autoimmune diseases. A distinctive feature of allergic stomatitis is the acute onset of the disease, accompanied by an increase in temperature, severe pain and putrid odor from the mouth, which does not disappear even after thorough brushing of the teeth.
Treatment methods
- Identifying the allergen and eliminating it (or minimizing contact).
- Antihistamine therapy.
- Relief of inflammation with corticosteroids.
- Taking analgesics to relieve pain.
- Local antiseptic drugs
- Diet.
Kinds
Varieties are distinguished according to the depth of damage to the mucous membrane and the reasons that caused the development of the pathology.
According to the depth of the lesion there are:
- aphthous;
- catarrhal;
- necrotic;
- ulcerative
Treatment varies depending on the stage. For the catarrhal variety, local treatment at home is predominantly prescribed. With the most severe necrotic, the child is hospitalized in a hospital.
Clinical manifestations of different types of disease
Signs of stomatitis in children vary significantly. This depends on the nature of the agent causing the disease.
Signs of this pathology:
- Viral - this type of pathology is characterized by the appearance of bubbles with a clear liquid that quickly open. Then erosive areas of round shape and small size are formed. They are covered with a grayish coating. In severe cases, the lesion has a draining character. The mucous membrane of the oral cavity and nasopharynx is bright red. There is pronounced pain. Similar skin rashes are also noted. The child shows signs of general intoxication and elevated body temperature. Signs of enlarged lymph nodes and conjunctivitis are detected. Possible loose stools and vomiting. Mucosal defects are epithelialized without scarring.
- Fungal - most of this species is candidal. It often develops in infants. It can also appear in children wearing braces. In other cases, its occurrence indicates immunodeficiency or other severe somatic pathologies. On the surface of the mucous membrane, areas covered with white plaque appear, then its area increases. A dense white layer covers the entire oral cavity; it has a curd-like consistency. In severe forms, it becomes gray and sometimes separates, exposing the bleeding surface. With the atrophic variety of the disease, only redness and dryness of the mucous membrane are detected. Plaque appears rarely, only in folds.
- Bacterial - the most common type of infection is the impetiginous type. It is characterized by confluent superficial erosive lesions and a purple color of the mucous membranes. Yellowish crusts form that stick the lips together. Salivation increased. There is an unpleasant odor from the mouth. Body temperature rises.
- Autozny - this variety is more common in children under 7 years of age. It is assumed that it is of an infectious-allergic or autoimmune nature. With it, aphthae appear on the mucous membrane - these are painful ulcers of a necrotic nature. They are round in shape, covered with fibrin, surrounded by a reddish granulation rim. The child's temperature rises, he is bothered by pain in his mouth, and refuses to eat. This option has a chronic course. Typically, exacerbations occur once or twice a year. Outside of exacerbation, aphthae heal.
Symptoms in children are quite varied. They depend on the form of the disease and the pathogen that caused it.
Treatment of stomatitis in children
Treatment of childhood and adult stomatitis follows the same methods. At the same time, some drugs used for adults are replaced with those that are better suited for the child’s body. First of all, we are talking about antibiotics, antiseptics and drugs to enhance immunity. Children are often prescribed more gentle methods, which include the use of herbs and natural tinctures for rinsing. At an early age, dentists recommend preventing stomatitis using traditional medicine.
| Age | Type of disease |
| From 0 to 3 years | Candidal stomatitis, or childhood oral thrush. This type of stomatitis is especially common in infants. |
| 1 – 4 years | Aphthous and herpetic stomatitis caused by external infections and mechanical trauma to the oral cavity. |
| Children of primary and secondary school age | Allergic and aphthous stomatitis. |
Is stomatitis contagious?
The disease can be recognized and treated in a short time.
At the appointment, the doctor must correctly determine the causes and type of stomatitis, because drawing up a treatment plan depends on this. Depending on the classification, appropriate drugs are selected. Is stomatitis contagious?
Inflammatory ulcers that arise as a result of:
- allergic reaction;
- mechanical damage to the mucosa;
- during intoxication.
The disease is contagious if it develops during an infection in the body.
This class includes: fungal, herpetic, infectious stomatitis. Stomatitis in children can be caused by the herpes virus, chickenpox, adenovirus, influenza or parainfluenza. Transfer methods:
- general toys;
- household items;
- dishes and cutlery;
- hygiene items;
- towels
It can also appear with a weakened immune system or while taking antibiotics.
Whether stomatitis is contagious can only be determined by a doctor upon examination of the oral cavity. You cannot self-medicate and wait until the inflammation goes away on its own.
Treatment of stomatitis at home
I would like to immediately note that treating stomatitis with folk remedies at home is possible, but you need to understand that in many cases it is impossible to do without a visit to a specialist and the use of antibiotics. Ignoring these points can lead to worsening of the disease and longer rehabilitation. In addition, on the Internet you can find a whole lot of “revolutionary” recipes for stomatitis, so you need to be able to separate the wheat from the chaff and understand which remedies can really help, and which are the fruit of the inflamed imagination of “couch healers”. Below we publish the most common methods of preventing and treating stomatitis with folk remedies, but please note that only an experienced specialist can draw up an optimal treatment plan.
In the case of children, treatment of stomatitis with folk remedies at home is used quite often. This is especially justified as a preventive measure, since the child’s body is more susceptible to the influence of the external environment. The most popular remedies are considered to be all kinds of decoctions, for the production of which chamomile, calendula, burdock, propolis and blackberry leaves are used. A homemade ointment is also used to treat stomatitis, which is made from novocaine, egg white and honey. Be that as it may, if your child shows signs of stomatitis, it is best to immediately take him to a specialist who can make the correct diagnosis and plan treatment.
Additional recommendations –
As soon as you notice the appearance of ulcers due to aphthous stomatitis, immediately start taking an antihistamine (anti-allergy) drug, plus eliminate from your diet all the foods and drinks that we described above. Immediately begin local therapy, which includes antiseptic rinses, anti-inflammatory gel + bismuth-based product to protect the surface of the ulcers from irritants. See if your toothpaste contains sodium lauryl sulfate or parabens, and if so, it is worth purchasing a toothpaste without these ingredients.
If brushing your teeth causes pain, then buy a soft toothbrush (they are usually used for inflammation and bleeding gums). For adults and children with constantly recurring outbreaks of aphthous stomatitis, there is an excellent preventive remedy - toothpastes with licorice extract and a whole complex of lactic enzymes. These components increase the protective factors of the oral mucosa, preventing the development of new cases of aphthous stomatitis.
Additional laboratory tests - with frequent, recurring outbreaks, a complete blood count should be performed to rule out hematological diseases. It is important to check blood plasma immunoglobulins and the number of lymphocytes, and take a test for HIV infection. To exclude autoimmune diseases, the patient is usually referred for the following tests:
- erythrocyte sedimentation rate,
- antinuclear antibodies and antineutrophil cytoplasmic antibodies,
- IgA-antiendomysial antibodies,
- antibodies to tissue transglutaminase.
If ulcerative lesions heal very poorly, take a long time and practically do not respond to local treatment, it is necessary to refer the patient for a biopsy to exclude granulomatous conditions such as orofacial granulomatosis, tuberculosis or malignant tumors.
Calling a doctor to your home –
If your child has stomatitis, it is very important to correctly determine its shape. Usually this is either an aphthous or herpetic form of stomatitis, and the most important thing is that they are treated completely differently. If your child develops stomatitis, you should not call the pediatrician. These specialists usually do not even know that there are several forms of stomatitis, and many of them still recommend treating them with brown, blue or Metrogil-dent gel. Or they prescribe a whole bunch of drugs with opposite effects - as if “at once for everything.”
It makes sense to contact a pediatrician only if the child’s general condition is severe, i.e. symptoms of intoxication (high temperature, dehydration...), but such symptoms are characteristic not of aphthous stomatitis, but of primary acute herpetic stomatitis. Therefore, it is optimal to contact a pediatric dentist, and you can always arrange a house call at the reception of a pediatric dental clinic. We hope that our review “Aphthous stomatitis: treatment in adults and children” was useful to you!
Sources:
1. Dental education of the author of the article, 2. National Library of Medicine (USA), 3. Textbook “Pediatric Dentistry” (Kolesov A.A.).4. “Pediatric therapeutic dentistry. National leadership" (Leontyev V.K.). 5. “Clinical recommendations (treatment protocol) for chronic recurrent aphthous stomatitis” (Volkov E.A., Butova V.G.).
Treating stomatitis with home remedies
| Facilities | Description |
| Hydrogen peroxide | Rinsing with a solution of hydrogen peroxide helps reduce discomfort and has an antiseptic effect. |
| Baking soda | Treatment of stomatitis in adults with soda is recommended when the disease is detected in the initial stages. A solution of the substance (a spoon in a glass of water) is recommended for rinsing. |
| Decoctions of chamomile, rose hips and calendula | They have disinfecting properties and contain vitamins and nutrients to maintain oral health. |