Childhood stomatitis is a disease of the oral mucosa, in which inflammatory processes form everywhere on it. The potential age at which children develop this disease ranges from 1 to 5 years. The cause of this disease may be an insufficiently well-developed immune system at an early age, as well as individual characteristics of the structure of the oral mucosa.
The child has a very thin and fragile mucous membrane, it is easy to injure, which can lead to infection and, as a result, inflammation. In an adult, saliva has some bactericidal properties, while in children this composition has not yet had time to form.
Types of stomatitis
Infection of the oral cavity can be caused by both viruses and protozoan microorganisms, which are an integral part of the human microflora and do not manifest themselves in any way if the immune system works without failures.
Children with low body weight, premature babies and those who often suffer from colds (respiratory) diseases are most susceptible to the development of stomatitis.
In the photo: the location of stomatitis in different parts of the oral cavity in children
Depending on the type of pathogen, several types of stomatitis are distinguished.
Viral (herpetic)
Occurs as a result of infection with the herpes virus. Children aged 1 to 3-4 years are most susceptible to this form of stomatitis. After the virus enters the body, an incubation period begins, which can last more than two weeks (in rare cases, the incubation of the virus takes 30 days).
The disease is severe: the child becomes lethargic, capricious, refuses food and water (infants can push away a bottle of milk and their mother’s breast).
Body temperature usually fluctuates between 37-38.5 degrees, but in exceptional cases it can reach 39 and even 40 degrees. In this case, we recommend reading what to do if your child has a fever. The rash characteristic of herpetic stomatitis can cover not only the oral cavity, but also areas of the face and ears. In case of moderate and severe damage, the child must be admitted to a hospital.
Fungal (candidiasis)
Candidiasis (thrush) is caused by fungi of the Candida family.
Even a newborn baby can become infected with thrush. Cases when a baby becomes infected in the maternity hospital account for about 40 percent of all candidiasis diagnosed in infants.
The main sign of pathology is a white cheesy coating covering the mucous membranes, the inner surface of the cheeks, gums, tonsils, tonsils, etc. Often, candidiasis is accompanied by glossitis - damage to the surface of the tongue. Candidal stomatitis in children is accompanied by elevated temperature (within 37.6-38.1 degrees) and a general deterioration in health.
Aphthous
This type of stomatitis rarely occurs in children under 5-7 years of age.
Pediatricians still cannot come to a consensus on what exactly causes the aphthous form of the disease. Some believe that the problem is problems with the functioning of the gastrointestinal tract; others are inclined to believe that the disease is of an allergic nature. It is the second version that is now recognized as more reliable.
With aphthous stomatitis, the baby develops aphthae - these are oval or round ulcers with clear, even edges and outlines. As the disease progresses, the aphthae becomes covered with a dense film. If it breaks through, the wound may become infected, which significantly aggravates the course of the disease and reduces the effectiveness of the therapy.
Bacterial
Caused by pathogenic bacteria, infection with which is often a complication of diseases of the oropharynx (laryngitis, tonsillitis, pharyngitis, etc.).
A separate type of stomatitis is traumatic (the result of mechanical damage to mucous areas) and allergic, which is a consequence of contact with allergens and increased production of histamine.
Causes
Stomatitis can have different etiologies
Doctors are not always able to identify the cause of stomatitis. The inflammatory form of the disease can occur suddenly against the background of complete clinical well-being. It is assumed that the mucous membrane can be damaged under the influence of a variety of negative factors.
Main reasons:
- Minor trauma to the oral mucosa as a result of careless brushing of teeth, an accidental bite, or damage during eating.
- Negative effects of substances contained in toothpastes and mouthwashes. For example, sodium lauryl sulfate can cause an inflammatory process in the mucous membrane.
- Sensitivity to certain foods. As a rule, these are chocolate, coffee, fruits, eggs, nuts, cheese, spicy and sour foods.
- Vitamin B12 deficiency in the diet.
- Insufficient intake of zinc, folic acid and iron from food.
- Allergic reaction.
- Hormonal changes during puberty and the menstrual cycle.
- Chronic stress.
- Entry of pathogenic bacteria, viruses or fungi into the oral cavity.
- Pathologies of immunity.
It is also necessary to take into account the influence of risk factors, the presence of which increases the likelihood of developing the disease. The main risk factors for stomatitis include:
- Inflammatory diseases of the digestive organs. This could be celiac disease, Crohn's disease or ulcerative colitis.
- Gastroesophageal reflux. The contents of the stomach can even enter the oral cavity.
- Behçet's disease is a rare disorder that causes inflammation throughout the body, including the mouth.
- HIV and AIDS.
- Childhood.
- Family history of inflammatory and infectious diseases of the mouth.
Often, stomatitis appears against the background of other inflammatory pathologies of the digestive organs.
Treatment
Therapy for stomatitis in children involves general rules that are mandatory for all types of the disease, and drug treatment aimed at eliminating the underlying cause.
Treatment should be prescribed by a pediatrician after examining the child, collecting the necessary information and identifying the causative agent of the infection.
General recommendations
General recommendations for treating stomatitis in young children include:
- Drink plenty of fluids (it is allowed to give the child unsweetened compotes and decoctions, but it is best to persuade the child to drink plain water).
- Regular ventilation.
- Air humidification in a children's room.
- Excluding refined and sweet foods from the child’s diet. If your baby is receiving complementary foods, you should avoid fruit purees made from sweet fruits (bananas) and cereals with added sugar.
- Medications depending on the type of stomatitis
For young children, lotions with chamomile decoction are used, which help relieve inflammation, have an antiseptic effect, and reduce pain.
Victoria Druzhikina
Neurologist, Therapist
Treatment of Herpetic stomatitis
Therapy for this type of disease is carried out in three stages:
- relieving irritation and eliminating the inflammatory process;
- healing of wounds formed after opening ulcers;
- fighting the virus and activating the body’s immune reserves.
To treat herpetic stomatitis in children under 3 years of age, antiseptic treatment of the oral cavity is used, after which antiviral medications are applied. Given the young age, rinsing with special infusions and solutions is excluded.
To treat the affected areas, you need to moisten a cotton swab with a solution of Furacilin (Rivanol) and gently wipe all the places where the rashes are localized. After this, you can begin applying ointments (for example, “Oxolinic” or “Interferon”) . The procedure is performed every three hours, unless a different treatment regimen is recommended by the pediatric dentist.
Doctor's advice
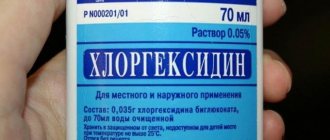
In the case of bacterial stomatitis, treatment with a solution of chlorhexidine bigluconate 0.05% is effective. If the child is small, then moisten the cotton wool, squeeze it out and wipe the affected area. Make sure that the drug does not flow from the cotton wool into the child’s throat. Processing is carried out 2-3 times per day. If the child knows how to rinse his mouth, then rinse 3-5 times a day. Hydrogen peroxide solution should not be used to avoid burns.
Victoria Druzhikina Neurologist, Therapist
When herpetic stomatitis is diagnosed in a child aged 1 year (or younger), parents do not always cope with antiseptic treatment measures. If it is not possible to treat the cavity with a tampon, you can purchase a special brush for young children (from 4 months), which is placed on the finger, wrap it in gauze and lubricate the affected areas.
Restoring immunity and fighting herpes viruses occurs with the help of medications (Arbidol, Acyclovir, Imudon). To heal wounds, you can lubricate them with sea buckthorn oil or rosehip oil.
Treatment of Candidal (fungal) stomatitis
Drugs with antifungal effects can only be prescribed to older children, so treatment of candidiasis in children under 3 years of age is predominantly local.
Newborn children can be prescribed medications such as Candide, Nystatin or Clotrimazole - these drugs are safe for children and can be used from the first days of a baby’s life.
In a clinic setting, a doctor may prescribe an irrigation procedure (irrigation of the oral cavity) using sodium bicarbonate in the form of a 2% solution, followed by treatment with sodium borate (10%).
An important condition is maintaining oral hygiene and regular treatment of lesions (plaque removal). This can be done using a soda solution (2 tablespoons of soda per mug of warm water). This procedure will help restore the alkaline environment, which is detrimental to yeast-like fungi. At home, it is recommended to repeat it at least 4-6 times.
Treatment of Bacterial Stomatitis
Treatment of bacterial stomatitis (often occurring at 2-3 years of age) is aimed at destroying bacteria that cause the development of the disease and deterioration of the baby’s well-being.
Severe cases require taking antibiotics, which are prescribed by a pediatrician after taking a smear to determine the causative agent of the disease and its sensitivity to various pharmacological groups of antibiotics.
For local treatment, you can use antibacterial sprays (Tantum Verde, Hexoral, etc.). Treatment must be combined with antiseptic treatment.
Allergic stomatitis
This type of stomatitis, in addition to hygiene measures, includes taking allergy medications and antihistamines (histamine blockers). Young children can use Tavegil or Suprastin for these purposes - both drugs are in drops.
Treating stomatitis in young children is not the easiest task, but it is quite feasible. To do this, you need to consult a doctor in time, follow his recommendations, monitor the baby’s nutrition and hygiene, and not make any changes to the treatment regimen on your own. The use of traditional methods should only be carried out with the permission of a doctor after examination and an accurate diagnosis.
To learn how to recognize and treat stomatitis in a child, watch the video:
This article has been verified by a current qualified physician, Victoria Druzhikina, and can be considered a reliable source of information for site users.
Bibliography
1. https://stgmu.ru/userfiles/depts/therapeutic_dentistry/Obyavleniya/stomatity_2013.pdf
Rate how useful the article was
5 Voted by 1 person, average rating 5
Did you like the article? Save it to your wall so you don’t lose it!
Symptoms and signs
With fungal stomatitis, a white coating appears
The symptomatic picture depends on the type of stomatitis. Infectious and inflammatory forms of the disease may have different symptoms.
Main manifestations:
- Painful sensations. The pain may worsen while eating because the skin under the ulcer is very sensitive.
- The appearance of red spots in the mouth.
- Swelling and redness around the ulcer.
- Burning sensation in the mouth.
- Weakness.
- High body temperature.
The most aggressive symptoms are characteristic of candidiasis and herpetic stomatitis.