What is stomatitis
Stomatitis is a group of dental diseases that have similar manifestations. The disease looks like inflammation of the oral mucosa, localized on the inside of the cheeks, on the palate, gums, lips, and tip of the tongue. In rare cases, lesions are diagnosed in the pharynx, on the tonsils - such formations are the most difficult to notice.
Typically, stomatitis develops as an independent disease as a result of a sharp drop in immunity, chronic infection, or allergies. The disease is contagious only in rare forms, but if left untreated, it quickly spreads through the mucous membranes of the oral cavity - it can provoke a sharp rise in temperature, causing weakness and prolonged malaise.
Stomatitis also manifests itself as a complication or symptom of other diseases - influenza, gastritis, diabetes, bronchial asthma, HIV infection.
Commonly used drugs for inflammation
In dentistry, several types of antibiotics are used for toothache and inflammation.
- Penicillin group. Prescribed at any age, with minimal side effects and easy tolerability. The main use is for periodontal inflammation. Effective against anaerobic bacteria.
- Cephalospoirins. They are used when it is necessary to perform dental manipulation with the risk of injury, as well as during periodontal and odontogenic inflammatory processes.
- Tetracyclines. Relieves swelling in the area of bone and soft tissue.
- Imidazole and derivatives. They have a depressing effect on pathogenic microorganisms and quickly penetrate bone tissue. Recommended for extensive inflammatory lesions.
- Macrolides. Used during pregnancy and allergies to drugs of the penicillin group. Eliminates gram-negative and gram-positive bacteria.
- Lincosamides. Do not cause allergies. Used for severe bone tissue infections.
The prescription of osteotropic antibiotics is combined if the tests reveal different types of pathogenic microbes.
Stomatitis: symptoms
Since stomatitis is an inflammatory process, the manifestations of the disease are standard. Dentists identify signs of stomatitis:
- redness, formation of a hyperemic area in the oral cavity;
- swelling, swelling of the affected area;
- the appearance of erosions, ulcers, aphthae;
- itching, burning at the site of ulcer formation;
- gray or yellowish coating along the edges of the canker sores;
- pain when talking, opening the mouth, or touching the mucous membranes of the mouth;
- bleeding due to accidental damage to plaque;
- local temperature increase.
Patients also note an unpleasant taste in the mouth, a putrid odor, and loss of appetite.
Treatment with honey and propolis
Propolis has unique antibacterial and anti-inflammatory properties. An alcohol tincture of propolis for stomatitis allows you to get rid of the resulting aphthae. The drug not only disinfects, but also anesthetizes the inflamed surface.
It is necessary to dissolve a teaspoon of the medicine in a glass of warm water, rinse the mouth with the resulting solution or use it for applications and lubrication of ulcers. It is advisable to first disinfect the affected area with hydrogen peroxide, and then apply propolis.
The medicine is used for:
- rinsing;
- applications;
- wiping.
It is strictly forbidden to apply alcohol tincture directly to canker sores!
Honey has powerful antiseptic properties and is included in many proven folk remedies. However, among doctors there is no clear answer to the question of how to treat and whether stomatitis can be treated with honey. It is believed that it can promote the proliferation of pathogenic bacteria.
Honey is most often used to treat diseases in children.
One of the most popular recipes is the egg-honey mixture. To prepare it you need to take:
- one egg (white);
- a teaspoon of honey;
- 1 ampoule of novocaine;
- one ampoule of vitamin B1 and B6.
Beat the resulting mixture well, take 1 tablespoon orally before meals, keep this portion in your mouth until completely absorbed.
Stomatitis: causes
A variety of factors and diseases contribute to the development of stomatitis in adults. For ease of diagnosis, doctors combined the causes of stomatitis into four groups, highlighting the main problem conditions:
- Mechanical injury. Ulcers appear as a result of some irritating factor. Damage can be caused by eating hard foods, poorly installed dentures, tartar buildup, and sharp edges of chipped crowns. Pathogenic microflora enters the damaged area, causing inflammation and active formation of ulcers.
- Chemical or thermal burn. Aggressive chemical agents can be food (citrus fruits), medications, nicotine, incorrectly selected toothpastes or mouth rinses. Thermal burn occurs when consuming excessively hot food or drinks.
- Poor oral hygiene. Failure to comply with regular hygiene procedures, tartar, and plaque provoke the active proliferation of bacterial microflora, which leads to inflammation of the oral mucosa.
- Chronic diseases. In adults, stomatitis develops as a reaction to problems of the gastrointestinal tract, cardiovascular system, due to anemia, endocrine pathologies, and HIV infections.
In addition to the listed categories, the causes of stomatitis can also be internal problems:
- vitamin deficiency, micronutrient deficiency - unbalanced diet, metabolic disorders in the body;
- allergies - of any origin;
- heredity - the individual reaction of the immune system to deteriorating health;
- a general decline in immunity - as a result of serious illnesses.
Unfavorable factors become catalysts for the development of pathology, and external circumstances aggravate the course of the disease.
The variety of causes points to an important point: there is no obvious causative agent of stomatitis. In order for an ulcer to localize, several circumstances must coincide - decreased immunity for any reason, an abundance of pathogenic microflora in the oral cavity, a traumatic agent.
Clinical researches
Repeated clinical studies have proven that the two-component mouth rinse ASEPTA ACTIVE more effectively combats the causes of inflammation and bleeding compared to single-component rinses - it reduces inflammation by 41% and reduces bleeding gums by 43%.
Sources:
- The role of anti-inflammatory rinse in the treatment of periodontal diseases (L.Yu. Orekhova, A.A. Leontyev, S.B. Ulitovsky) L.Yu. OREKHOVA, Doctor of Medical Sciences, Prof., Head of Department; A.A. LEONTIEV, dentist; S.B. ULITOVSKY, Doctor of Medical Sciences, Prof. Department of Therapeutic Dentistry of St. Petersburg State Medical University named after. acad. I. P. Pavlova
- The use of adhesive balm "Asepta®" in the treatment of inflammatory periodontal diseases L.Yu. OREKHOVA*, Dr. med. Sciences, Professor, Head of Department V.V. CHPP**, Dr. med. Sciences, Professor, Head of Department S.B. ULITOVSKY*, Dr. med. Sciences, Professor A.A. LEONTIEV*, dentist A.A. DOMORAD**, O.M. YAKOVLEV** SPbSMU named after. acad. I.P. Pavlova, St. Petersburg - *Department of Therapeutic Dentistry, **Department of Microbiology
- https://cyberleninka.ru/article/v/puti-sovershenstvovaniya-pervichnoy-profilaktiki-zabolevaniy-parodonta Acute herpetic stomatitis in children, Baranaeva E.A. Merkulova E.P. magazine "Medicine and Healthcare"
- https://cyberleninka.ru/article/v/osobennosti-protivoretsidivnogo-lecheniya-allergicheskogo-stomatita Acute stomatitis in children, Drobotko L.N., Strakhova S.Yu.
Types of stomatitis in adults
Effective treatment of stomatitis in adults begins with the diagnosis of pathology. Identifying the provoking factor is one of the main tasks of the dentist. The situation is aggravated by the fact that many reasons are similar - they overlap each other, distorting the clinical picture. For this reason, only experienced doctors treat stomatitis in adult patients.
There are a variety of classifications of stomatitis:
- according to the course - acute periodic, chronic, recurrent;
- by external manifestation - redness, aphthae, erosion;
- by localization - on the lip, on the tongue, on the palate, in the throat.
When diagnosing and selecting a treatment plan, dentists try to take into account the versatility of the disease - the form, causes, degree of damage to the mucous membranes, stage of the disease, and other classification parameters. Based on these factors, it is customary to identify the most popular types of stomatitis in adults:
- aphthous;
- ulcerative;
- herpetic;
- candida;
- prosthetic;
- allergic;
- ray.
Aphthous stomatitis
Aphthous stomatitis is characterized by the appearance of round ulcerative formations covered with necrotic plaque. This is the most common variant of the disease - it occurs in 65-70% of dental patients.
The causes of aphthae formation are viral and bacterial diseases. Localization of ulcers is on almost any mucous tissue of the oral cavity.
Initially, the patient is faced with the fibrinous form, when local blood circulation is disrupted. If left untreated, the disease turns into a necrotic form, accompanied by tissue death, or into a scarring form - the mucosal tissue changes structure.
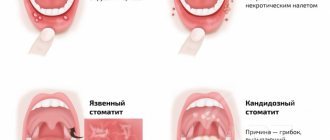
Ulcerative stomatitis
Ulcerative stomatitis is characterized by the formation of deep, painful ulcers in the mouth. They usually arise due to:
- poor hygiene - a large amount of plaque on the teeth, tartar;
- problems with the gastrointestinal tract - metabolic disorders;
- chemical burns - abuse of especially spicy foods.
Lesions affect the deep layers of tissue, so treatment of ulcerative viral or bacterial stomatitis in adults is carried out only by a dentist according to a carefully developed plan.
A separate type of ulcerative stomatitis is ulcerative-necrotizing gingivitis, Vincent's stomatitis. The cause of the disease is the active proliferation of pathogenic microflora, the influence of spindle bacillus and Vincent's spirochete. The disease is observed against the background of a sharp decrease in immunity and is characterized by reactive development. Patients complain of swelling of the gums, suppuration, pain, putrid breath, and loss of appetite. Without treatment, tissue necrosis progresses and tooth roots are exposed.
Herpes (herpetic) stomatitis
Viral herpetic stomatitis is a contagious variant of the disease provoked by the herpes virus. Transmitted through hygiene items, through negligence, by airborne droplets.
Externally it differs from other types, since the lesions look like fluid-filled blisters before turning into ulcers.
During treatment, the doctor conducts complex therapy, including taking medications.
Candidal stomatitis
The cause of candidal stomatitis is a fungus that causes the appearance of a cheesy coating on the oral mucosa. Underneath the plaque is a swollen, inflamed area. When the formations are removed, the tissue surfaces begin to bleed.
The causes of the disease are decreased immunity and poor hygiene. Treatment requires careful selection of drugs so as not to aggravate the situation.
Prosthetic stomatitis
The pathology is typical only for adult patients, as it is a consequence of improper prosthetics, individual intolerance to the crown material, and poor quality of care for the orthopedic product.
The disease manifests itself as inflammation of the soft tissues around the prosthetic structure, turning into ulcers and erosion.
Allergic stomatitis
A distinctive feature of the disease is dryness and itching in the mouth. This is how increased sensitivity to allergens manifests itself. At the site of the inflamed areas, aphthae and ulcers quickly form. In severe cases, an ulcerative-necrotic form may develop.
Pathology happens:
- acute - single manifestation;
- chronic - with constant relapses and complications.
Treatment requires an integrated approach.
Radiation stomatitis
The reason for the appearance is the patient undergoing radiation therapy or chemotherapy and, as a result, a decrease in immunity. It occurs acutely - with inflammation and ulcers. Requires careful attention from the doctor during treatment to avoid worsening the situation.
Prevention
To ensure that candidal stomatitis never bothers you, you should follow a few simple but very useful rules:
- Follow basic hygiene rules. Namely: wash your hands well with soap, especially when returning from the street, brush your teeth, use dental floss at least once a day, and also rinse your mouth with special means.
- You should definitely buy a new toothbrush. For those who have dentures, it is recommended to place them in a disinfectant solution overnight.
- After consuming liquid antibiotics, you should immediately rinse your mouth with water.
- When using spray corticosteroid drugs, you should wear a special nozzle.