Author:
- Khirnetkina Ayuna Fedorovna
otorhinolaryngologist, otoneurologist, audiologist
4.25 (Voted by: 
In medicine, the term paratonsillar abscess refers to the accumulation of pus in the tissues surrounding the tonsils. The term “paratonsillitis/peritonsillitis” is also distinguished when purulent has not yet formed. This is the stage before the formation of the abscess itself.
Peritonsillitis and paratonsillar abscess occupy first place among purulent processes of the pharynx and are a consequence of the spread of an acute inflammatory process from the palatine tonsils to the paratonsillar tissue and surrounding tissues, characterized by their inflammatory infiltration (edema). More often there is a one-sided process. These conditions are a complication of acute or exacerbation of chronic tonsillitis, tonsillitis, due to trauma to the pharynx by a foreign body, odontogenic process (caries, periodontitis, etc.).
Peritonsillar abscesses belong to a group of diseases that require emergency care. For diffuse purulent inflammation of the peritonsillar tissue for 2 days, when an abscess has not yet formed, the treatment is the same as for a severe form of tonsillitis (lacunary or follicular). In the absence of positive dynamics, the patient is hospitalized. In cases where an abscess has formed (usually by the 5-6th day, and with some infections and a decrease in the body’s immunity, an abscess can form, despite active treatment, earlier - on the 3-4th day from the onset of the disease) it is necessary to perform his autopsy.
How to treat peritonsillar abscess?
Treatment is carried out in two stages:
- Surgical.
- Conservative.
First of all, it is necessary to evacuate the pus from the peritonsillar space.
This can be done in the following ways:
A) Tonsillectomy - removal of the tonsils.
B) Puncture (puncture) and aspiration.
B) Opening (incision) and dividing the paratonsillar space.
After draining the pus, the patient should receive antibacterial and anti-inflammatory therapy.
Diagnostics
In the vast majority of cases, the diagnosis of PTA is made clinically, based on the results of pharyngoscopy (examination of the pharynx). It is confirmed by obtaining purulent discharge during drainage of the abscess or by instrumental studies (most often ultrasound).
Pharyngoscopy reveals a swollen and/or fluctuating tonsil with deviation of the uvula in the direction opposite to the lesion, hyperemia (redness) and swelling of the soft palate. In some cases, there is plaque or liquid discharge in the palatine tonsil. There is an increase and tenderness of the cervical and submandibular lymph nodes.
Bilateral PTA is extremely rare and its diagnosis is more difficult due to the lack of asymmetry in the pharynx, as well as the rarely present spasm of the masticatory muscles.
Laboratory tests are not required to make a diagnosis; they are additionally prescribed to determine the severity of the disease and select a treatment method.
Laboratory tests may include:
- general blood test with leukocyte formula;
- study of electrolytes (potassium, sodium, chlorine) for signs of dehydration;
- strepta test to exclude GABHS;
- culture for aerobic and anaerobic bacteria if the abscess was drained (culture is recommended only for complicated PTA, recurrent PTA, or in patients with immunodeficiency conditions).
Instrumental examination methods - ultrasound, computed tomography, lateral neck x-ray, magnetic resonance imaging or angiography - are not necessary and are performed to exclude other diseases if the diagnosis of PTA is not obvious.
Differential diagnosis
Severe course of acute tonsillopharyngitis . Frequent pathogens are Epstein-Barr virus, herpes simplex virus, Coxsackie virus (herpangina), adenovirus, diphtheria, GABHS, gonorrhea. It manifests itself as bilateral swelling in the throat, hyperemia, and plaque may be present on the tonsils.
Epiglottitis . An inflammatory disease of the epiglottis, usually caused by Haemophilus influenzae. More common in young children who have not been vaccinated against Haemophilus influenzae type b. Progresses faster than PTA. Manifested by sore throat, drooling, difficulty swallowing, respiratory failure.
Retropharyngeal abscess (retropharyngeal abscess) . Purulent inflammation of the lymph nodes and tissue of the retropharyngeal space. Most often observed in children aged 2 to 4 years. During pharyngoscopy, minimal changes are noted. Main complaints: stiff neck, pain on movement, especially when extending the neck (as opposed to the increased pain on flexion seen with meningitis), swelling and tenderness of the neck, chest pain, difficulty swallowing, drooling, muffled voice, spasm of the masticatory muscles ( present in only 20% of cases).
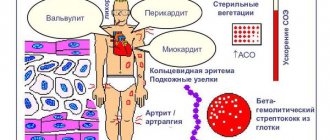
Signs and symptoms of paratonsillitis
The disease has an abrupt onset. An abscess forms a few days after an exacerbation of tonsillitis or the onset of a sore throat and is accompanied by vivid symptoms:
- acute pain in the throat, radiating to the jaw or ear;
- sensation of a “lump” in the throat;
- fever (temperature 39-40°C);
- submandibular lymph nodes are greatly enlarged;
- difficulty swallowing (even drinks);
- the appearance of a repulsive odor from the mouth;
- neck pain that gets worse with exercise;
- general weakness;
- inability to fully open the mouth;
- headache;
- speech impairment (voice as if there is a hot potato in the mouth);
- difficulty breathing (with large ulcers).
Spontaneous breakthrough of suppuration into the throat cavity is accompanied by an improvement in well-being and the appearance of an admixture of pus in the saliva.
The spread of the abscess contents into the peripharyngeal space significantly worsens the condition, so there is no need to delay operations to open the abscess. If you have even one of the symptoms listed above, schedule a consultation with an otolaryngologist today. Doctors at the Center for Operative Otolaryngology at GMS Hospital use gentle microsurgical techniques, which contributes to a speedy recovery and the absence of relapses of the disease.
Causes of the disease
Peritonsillitis occurs when pathogens enter the tissues around the tonsils.
The causative agents of the disease are streptococci, staphylococci, and fungi.
How do pathogenic microorganisms get into the paramygdaloid tissue? There may be several reasons for the start of the inflammatory process:
- untreated tonsillitis, when bacteria from the tonsils penetrate into nearby tissues;
- exacerbation of chronic tonsillitis, when pathogenic microflora also penetrates from the tonsils;
- dental diseases - for example, caries (infection comes from the oral cavity), although it is not necessary that the tonsils themselves become inflamed;
- injury to the tissue around the tonsils, during which infection occurs;
- infection through the bloodstream;
- chronic accumulations of infection in the body (for example, chronic sinusitis);
- diabetes;
- reduced immunity;
- smoking.
Typically, purulent inflammation acts as a complication of chronic or acute tonsillitis (tonsillitis) - this is the most common cause of the disease.
How is an abscess removed?
A few days before the planned surgery, the patient needs to start taking antibiotics.
Before the autopsy begins, the patient is given an anesthetic for local anesthesia. In the place where the wall of the pharynx protrudes most and has the smallest thickness, the doctor makes an incision into the purulent formation. Its depth does not exceed 10-15 millimeters - this way it is possible to prevent damage to adjacent vessels and nerves. Using a special suction, the surgeon removes purulent contents from the cavity, after which he inserts a blunt instrument into the incision and destroys the partitions of the cavity from the inside to improve the outflow of pus. Next, an antiseptic is injected into the cavity, the doctor stops the bleeding and sutures the edges of the wound.
If during the process it is discovered that the pus does not have a clear localization, but has spread between the fascia of the neck, the surgeon decides to take the necessary therapeutic measures. The scope of the operation is expanding, since this condition is deadly for the person being operated on. If necessary, a drainage tube can be inserted into the patient through incisions in the neck. Each specific situation requires different surgical procedures.
Clinical picture
ENT patients mainly complain of a sensation of a foreign body in the throat and larynx and pain, which becomes much stronger when eating. In some cases, the pain is so severe that swallowing becomes impossible. During examination of the larynx, a limited area of inflamed mucous membrane is observed, and in its center a focus of inflammation is clearly visible. As the disease develops in the arytenoid cartilage or epiglottis, their mobility sharply decreases. In the absence of timely treatment, acute laryngeal stenosis may develop.
Friends! Timely and correct treatment will ensure you a speedy recovery!
Opening an abscess (furuncle) of the ear
Ear boil is a purulent-inflammatory disease of the hair follicle of the skin of the auricle and external auditory canal.
The cause of an ear boil is microtrauma when scratching or cleaning the ear with a cotton swab or foreign objects (matches, pins, etc.). Pathogenic microflora settles on the injured surface of the skin of the external auditory canal and an inflammatory process develops. This is facilitated by water getting into the ear, metabolic disorders that change the barrier function of the skin (diabetes, obesity), decreased immunity, unfavorable ecology and environmental factors (air pollution, working in a dusty room, etc.).
The development of the disease goes through several stages:
- infiltrative,
- abscess formation and necrosis,
- recovery
The disease is characterized by diffuse pain in the affected ear, aggravated by chewing, talking, and opening the mouth. Due to swelling of the skin of the external auditory canal, its lumen narrows until there is no lumen at all. This leads to a feeling of ear fullness and decreased hearing on the affected side, since sound waves cannot be carried to the eardrum and transmitted along the chain of auditory ossicles to the inner ear. Upon examination, the skin of the external auditory canal is hyperemic and swollen; at the stage of abscess formation, an area of necrosis with a purulent core can be seen. As a rule, regional lymph nodes are involved in the process, enlarging and causing pain upon palpation. Depending on the stage of the disease and the extent of damage to the skin of the external auditory canal, the clinical picture may be limited only to local manifestations, or accompanied by symptoms of general intoxication - high fever, weakness, malaise, headache.
Diagnosis of an ear boil
Diagnosis of an ear boil is not difficult; it is enough to collect an anamnesis, the patient’s characteristic complaints and examine the external auditory canal using an otoscope or endoscope.
Treatment of ear boil
Treatment for ear boils depends on the stage of the disease. At the infiltration stage, local alcohol applications (calendula solution, chamomile, iodine tincture), oral antibiotics, antiplatelet agents (aspirin) to prevent thrombosis, and antihistamines are prescribed. If it was possible to start treatment in the first hours or day of the disease, then the process is localized and quickly resolves without a stage of suppuration. It should be remembered that self-medication and independent attempts to open an abscess threaten the development of serious complications, including death.
Opening a boil in the ear
In the stage of suppuration and necrosis, it is recommended to open the boil and drain its cavity, rinse with antiseptic solutions, continuing active general therapy.
In the resolution stage, a good therapeutic effect is achieved by the use of physiotherapeutic procedures, such as ultraviolet irradiation of the affected area, laser therapy or photochromotherapy.
Doctors at the ENT Clinic in Chertanovo carry out the full range of necessary treatment measures for patients with ear boils, selecting an individual treatment regimen and choosing certain techniques based on the stage of the disease, the patient’s age, duration of the disease and concomitant pathology. After opening the boil, it is possible to conduct detoxification therapy and monitor the patient in a day hospital. During the recovery stage, patients undergo laser treatment or photochromotherapy of the external auditory canal in order to improve the regeneration process of the skin of the external auditory canal and prevent relapses in the future.
After recovery, it is necessary to conduct an examination for concomitant conjugate, hidden pathology to prevent the occurrence of boils in the future, since in the absence of treatment of the underlying disease, frequent relapses of the disease are possible.
Prevention of paratonsillitis
The following simple preventive measures will help prevent the development of peritonsillar abscess:
- strengthening the immune system;
- healthy lifestyle;
- timely treatment of acute and chronic diseases of the ENT organs (sinusitis, adenoids, pharyngitis, tonsillitis, etc.), caries;
- rejection of bad habits.
In the presence of recurrent abscesses, elective tonsillectomy is recommended.
Opening a peritonsillar abscess at the GMS clinic is a simple and safe surgical procedure that is performed in an outpatient or inpatient setting. Recovery takes 10-14 days, after which you will return to your normal life. You can make an appointment with an otolaryngologist at GMS Hospital by phone or using an online application.
Complications
The development of a purulent inflammatory process leads to severe complications:
- Bronchopneumonia as a result of infection spreading through the upper respiratory tract;
- Congestive pneumonia due to respiratory failure;
- Brain abscess, purulent meningitis due to the spread of infection into the cranial cavity through the circulatory system;
- Cardiac arrest;
- Asphyxia (suffocation) due to blocking of the trachea by an abscess, swelling of the larynx, pouring of purulent masses into the larynx during independent opening of the formation;
- Purulent mediastinitis – spread of infection into the mediastinum;
- Phlebitis;
- Jugular vein thrombosis;
- Arrosive bleeding due to purulent fusion of blood vessels;
- Sepsis (blood poisoning).
Opening a hematoma (abscess) of the nasal septum
Traumatic injuries to the nose are often accompanied by external bleeding of varying degrees of intensity, which stops on its own or with the help of nasal tamponade. With normal blood clotting and the absence of severe concomitant pathology, bleeding is not dangerous and the body very quickly compensates for this blood loss.
It is very important to monitor a patient with a nasal injury in the first days after the injury, since complications in the form of a hematoma of the nasal septum and its subsequent abscessation are possible. According to statistics, in 1 out of 100 cases of nasal injuries we encounter such complications. Considering the abundant blood network in the nasal cavity and the direct connection with the vessels of the brain, the high importance and timeliness of the primary diagnosis of these nasal diseases for the prevention of serious intracranial complications becomes obvious.
Causes of hematoma of the nasal septum
The immediate cause of a hematoma of the nasal septum is a trauma to the nose, which results in damage to the vessels of the perichondrium in the cartilaginous part of the nasal septum and hemorrhage into the cavity between the mucous membrane of the nasal cavity and the cartilage. Predisposing factors are disorders of the blood coagulation system, acute respiratory diseases, in which a hematoma of the nasal septum can appear even with the slightest trauma to the nose.
Symptoms of nasal septum hematoma
The main and first symptom of the development of a hematoma of the nasal septum is difficulty in nasal breathing, which develops several days after the injury to the nose, on one or both sides, increasing in intensity every day. The addition of a headache, increased body temperature, and malaise indicate the addition of pathogenic microflora and the formation of an abscess of the nasal septum.
Diagnosis of nasal septum hematoma
Due to the high risk of developing intracranial complications, diagnosis of nasal septum hematoma and its possible abscess formation should be timely and based on characteristic complaints, medical history and rhinoscopy data.
Treatment of nasal septum hematoma
Treatment of hematoma of the nasal septum consists of emptying the hematoma cavity, leaving drainage and tamponade of the nasal cavity on both sides for 1-2 days. General treatment consists of prescribing antibiotics and hemostatic agents for changes in hemostasis. In case of an abscess of the nasal septum, the abscess is opened and emptied, drainage is introduced into the abscess cavity and systemic antibiotic therapy is performed.
As a rule, with timely diagnosis and adequate treatment, recovery occurs within 5-7 days.
The ENT Clinic in Chertanovo provides comprehensive care to patients after nasal injuries complicated by the development of a hematoma of the nasal septum and its abscess formation.
Indications for autopsy
Drug therapy is possible only at the stage of paratonsillitis, when there is inflammation, but there is no abscess yet. If antibiotic therapy was not carried out in the first two to three days, the abscess will need to be opened. At the stage of purulent inflammation, conservative treatment will not give a positive result.
In 25% of cases, the abscess opens on its own without surgical intervention. At the same time, the temperature drops sharply, the pain goes away and recovery occurs. But if this does not happen, then the patient is shown opening the abscess cavity with a scalpel.
If the operation is not performed, then the purulent inflammation can go further, which poses a danger to life.
Treatment methods
The treatment tactics for paratonsillitis depend on the extent of the spread of the purulent process and the presence of complications. Peritonsillitis in the initial stage is treated conservatively, with antibiotics, decongestants, painkillers and anti-inflammatory drugs. If drug treatment is ineffective or an abscess forms, the abscess is surgically opened and its cavity is drained. The opening of the paratonsillar abscess is carried out under local anesthesia. The otolaryngologist dissects the wall of the abscess, removes the purulent contents, and rinses the cavity with an antiseptic. An improvement in the condition is observed immediately after opening and draining the abscess.
You have questions? We will be happy to answer any questions Coordinator Tatyana
Types of disease
The inflammatory process can occur on the left or right in the pharynx. Such inflammation is called one-sided - respectively, a left-sided or right-sided abscess. If inflammation occurs on both the left and right at the same time, this is a bilateral type of inflammation.
If we take the location of the purulent “pocket” as the basis for the classification, the following types of disease are distinguished:
- anterior - the most common type of diagnosis; the tissues above the tonsils become inflamed;
- posterior, when purulent inflammation occurs between the posterior palatine arch and the tonsil; such inflammation can spread to the larynx;
- lower, when inflammation is located at the lower pole of the tonsil, while the anterior palatine arch moves forward and downward;
- external (lateral) - a less common, but most severe type, in which a suppurating cavity appears between the edge of the tonsil and the wall of the pharynx. With this form of the disease, pus can break into healthy tissue in the neck.
Preparing for surgery
Surgery is performed only when the abscess is “ripe,” that is, a purulent pocket is completely formed. This usually occurs on the 5th day after tonsil swelling occurs.
Checking the readiness of the cavity for opening is carried out by a diagnostic puncture. Using a large needle, a puncture is made in the place that sticks out the most. All manipulations are controlled by an ultrasound machine or endoscopic observation. If pus is detected in the sample, it means that the abscess is ripe for surgery.
If necessary, a blood test is prescribed, as well as a culture to determine the pathogen and check for resistance to antibacterial drugs.
After the examination, the patient is sent to the operating room, where the abscess will be surgically opened.