Treatment of
jaw
fractures is a characteristic of conservative and surgical treatment methods. Treatment of any injury must begin with first aid. For fractures of the maxilla, it is necessary to restore the prominence and height of the face and recreate the pre-traumatic occlusion. The jawbone is often stable, so treatment is carried out by fixing the upper and lower teeth together. Various options for osteosynthesis of facial bones with titanium mini-plates. When the upper jaw is fractured, its fragments are displaced downward, disrupting the usual relationship of the teeth of the upper and lower jaw and somewhat lengthening the face.
PROVIDING ASSISTANCE FOR FRACTURES OF THE UPPER AND LOWER JAWS
Qualified assistance is provided before admission to a specialized hospital.
When providing qualified surgical care, the surgeon must:
1) anesthetize the fracture site;
2) inject antibiotics into the wound and administer antibiotics internally;
3) carry out simple transport immobilization, for example, apply a standard transport bandage;
4) make sure there is no bleeding from the wound, asphyxia or its threat during transportation;
5) carry out anti-tetanus measures according to the instructions;
6) ensure proper transportation to a specialized medical institution, accompanied by medical personnel (determine the type of transport, the position of the patient);
7) clearly indicate in the accompanying documents everything that was done to the patient.
Patients with complex and complicated facial injuries should be referred to a specialized department if there is a need for primary plastic surgery of soft tissues and the use of the latest methods for treating facial bone fractures, including primary bone grafting.
Temporary (transport) immobilization of fractures of the lower and upper jaw. It is carried out outside a specialized medical institution or at the scene of an incident by paramedics, doctors of other specialties, sometimes in the form of mutual assistance.
For temporary immobilization use:
1) Circular bandage parietal-chin bandage
2) Standard transport bandage
3) Soft chin sling Pomerantseva-Urbanskaya
4) Intermaxillary ligature fastening
Circular bandage parietal-chin bandage.
Circular tours of the bandage, passing through the chin of the lower jaw and parietal bones, do not allow fragments to move during transportation of the victim. For this purpose, you can use a mesh elastic bandage.
Standard transport bandage.
A standard transport bandage consists of a rigid chin sling and a support cap (dimensionless). The latter has 3 pairs of loops for fixing rubber rings, which tightly press the sling to the chin area. Under the loops there are fabric pockets for cotton pads, which allow you to remove the rubber rings from the swollen soft tissues of the face and prevent their injury. The cap is placed in such a way that it tightly covers the occipital protuberance, and its straps are tied on the forehead. A rigid chin sling is made with a cotton-gauze liner so that it covers the edges of the sling along its entire perimeter. This prevents direct contact of the rigid structure with swollen soft tissues, and can also serve as a protective bandage in case of damage to the skin of the chin area. Depending on the number of pairs of rubber rings used in the cast, the sling can hold the fragments without pressure or apply pressure to them. For fractures of the lower jaw behind the dentition or for a fracture of the upper jaw, a standard bandage can be applied using 3 pairs of rubber rings (as a pressure bandage)
In case of fractures of the lower jaw within the dentition, it should be applied only to support the fragments. Excessive pressure on displaced fragments will lead to even greater displacement with the risk of developing asphyxia. However, such a differential approach is only possible in a specialized department where there is a dental surgeon. Non-specialists should be advised to apply a standard transport dressing as support.
Soft chin sling by Pomerantseva-Urbanskaya.
Its chin part is made of several layers of canvas or calico. The intermediate section is represented by two wide elastic bands (haberdashery), which go into the peripheral section of the bandage, made of the same material as the chin part. The latter has lacing, which allows you to adjust the degree of tension of the rubber strips of the sling. This bandage is comfortable for patients, easy to use and provides good fixation of fragments
How to eat after splinting
Hard splinting involves difficulties in eating, but at the same time, during this period it is especially important for the body to receive a large amount of vitamins, minerals, and nutrients required for the speedy regeneration of bone tissue. The patient's menu after splinting usually includes various nutritious broths, fruit, vegetable and meat purees (baby purees), semi-liquid and liquid porridges. It is necessary to monitor the content of large amounts of protein, calcium, phosphorus, and zinc in food. It is possible to replace some meals with infant formula or sports nutrition, since in both cases the content of substances necessary for the body is high.
It is strictly forbidden to drink any alcoholic beverages during treatment, especially if, in addition to the jaw, there is also a traumatic brain injury. In addition, you should not try to eat solid foods that require chewing. Firstly, it can cause severe pain. Secondly, it can lead to improper healing of damaged bone tissue.
If you receive injuries that have symptoms similar to a jaw fracture: acute pain, bleeding, immobilization of the jaw, and so on, you should immediately seek professional help. Attempts at self-treatment or complete lack of treatment cause irreparable harm and lead to loss of dental functionality.
INTERDENTAL AND INTERMAXILLARY LIGATURE BINDING:
Requirements for using the method:
1) on each fragment there are at least two adjacent stable teeth and two antagonist teeth;
2) the bandage should not include teeth located in the fracture line, with signs of periodontitis and pulpitis, and having pathological mobility.
Contraindications to the application of intermaxillary ligature bonding:
1) concussion;
2) the possibility of bleeding in the oral cavity;
3) danger of vomiting;
4) transportation of the patient by water or air.
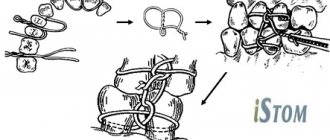
Among the many types of intermaxillary ligature fastening, the following are most often used: simple, figure eight, according to Ivey.
a) simple ligature binding.
With a simple intermaxillary ligature fastening, the end of a ligature wire 5-6 cm long is passed into the interdental space, covers one of the teeth included in the bandage from the lingual side and returns it through the other interdental space to the vestibule of the mouth. On the vestibular side, both ends of the wire are twisted together. The twisted wire tightly wraps around the neck of the tooth. The second ligature is fixed in the same way on the adjacent tooth. These two wires are then twisted together, combining the two teeth into one bandage. A similar bandage is applied to the teeth of the second fragment, then to the antagonist teeth. Having reduced the fragments, they are brought into contact with the teeth of the upper jaw and fixed in this position by twisting the wire extending from the teeth of the lower and upper jaws with each other on each side in turn. The ends of the wire are cut with scissors for cutting metal and bent so that they do not injure the mucous membrane of the cheek and gums.
b) figure eight ligature binding.
When fastening in the form of a figure eight, both ends of a ligature wire 6-8 cm long are passed into the interdental spaces from the vestibular side to the oral side so that the wire covers two teeth included in the bandage at once. Then both ends of the wire are returned to the vestibular side, passing them through the gap between the teeth included in the bandage. In this case, one end is passed over the wire covering the teeth from the vestibular side, and the other - under it. On the vestibular surface, the ends of the wire are twisted together. Then the same bandage is applied to the teeth of the second fragment and the antagonist teeth. As in the previous case, the wire fixed to the teeth of the upper and lower jaws is twisted together. The excess is cut off with scissors.
c) ligature binding according to Ivey
When fastening according to Ivy, a wire 10 cm long is first bent into the form of a hairpin, leaving one end 1-1.5 cm longer than the other. At the end of the “hairpin” a loop with a diameter of about 0.2 mm is formed. To do this, you can use a small piece of aluminum wire, crampon tongs, or tweezers. Both ends of the wire are passed from the vestibular side to the oral side between the teeth included in the bandage. The long end of the wire is returned to the vestibular surface through the interdental space located posterior to the loop and passed through it. The short end is brought out to the vestibular side through the interdental space located anterior to the loop and twisted with the long end. The excess wire is cut off by bending the remaining end about 0.5 cm long so that it does not injure the mucous membrane of the cheek. The same bandage is applied to the teeth of the second fragment, the antagonist teeth. The fragments are reduced and fixed to the teeth of the upper jaw with wire passed through the loops of the ligature bandage on each side.
This method has some advantages over the simple one: it is less traumatic, it allows you to examine the oral cavity without removing the entire structure, but only by cutting off the ligatures connecting the teeth.
Indications for osteosynthesis of the jaw with plates
The main indication for installing metal plates for osteosynthesis is the prevention of complications that cannot be effectively prevented by applying a traditional splint. In the case of osteosynthesis, an important task for the surgeon is to compare the fragments and fix them in the correct position. If successful, fusion will take up to 3–4 weeks.
Indications:
- fracture behind a row of teeth;
- inflammation that provoked injury;
- significant displacement of bone elements;
- high mobility of teeth at the fracture site;
- incorrect position of the jaws relative to each other.
Recovery after surgery
Rehabilitation after installation of a titanium plate for a jaw fracture takes 6 months. The specific recovery time depends on how much time has passed from the moment of injury to treatment, as well as on the patient’s age, his condition, the severity of the injury, and the method of osteosynthesis.
Rules during rehabilitation:
- immediately after the manipulation, a bandage is applied for fixation; it must be worn constantly;
- it is important to exclude any movements (talking, chewing, opening and closing the mouth);
- drug rehabilitation involves taking a course of antibiotics and restoratives, the drugs are selected individually and prescribed by a doctor;
- for recovery, the patient is prescribed decongestant and anti-inflammatory physiotherapy (from day 2 - UHF, from day 4 - magnetic therapy, after 2 weeks you can start a course of electrophoresis);
- classes in LVF (therapeutic and restorative physical education) begin 3–5 weeks after removing the fixing bandage, their goal is to restore normal speech function, normalize chewing, and facial expressions.
For the entire recovery period after installation of a plate for a fracture, the patient is prescribed a diet (liquid meals, purees, strictly at room temperature, taken through a straw). Solid food is introduced into the diet gradually after the bandage is removed and chewing functions are restored.
To avoid complications, it is important to maintain good oral hygiene. You can brush your teeth only after removing the bandage and restoring mobility, so in the first weeks hygiene comes down to rinsing your mouth, which should be done up to 10 times a day (including after each meal).
Teeth splinting technique
Installation of permanent tires made of metal, fiberglass or aramid almost always follows a similar scenario.
- Consultation, determination of indications and contraindications.
- Professional teeth cleaning, etching of enamel with a special solution.
- Forming a groove in the enamel to attach the splint (in some cases this can be avoided).
- Primary fixation of the splint using dental glue.
- Application of composite material.
- Illuminating the composite with an ultraviolet lamp until it hardens.
- Tire grinding.
The splinting procedure for injuries and fractures is carried out under the guidance of a maxillofacial surgeon and differs from the classical technique in the design of the splint and the method of its fixation. Installation of a custom retention tray requires taking impressions.