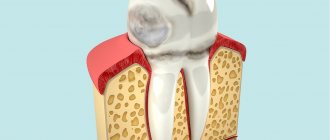
Wedge-shaped defects are defects in the hard tissues of the tooth, located on the vestibular surface of the teeth, most often canines and premolars. Defects are formed in the area of the tooth neck and arise due to trophic lesions of the organic matter of enamel and dentin, usually in connection with past diseases of the gastrointestinal tract and endocrine system. Often these defects accompany periodontal disease. The pulp remains covered with secondary, compacted dentin and undergoes atrophy and sclerosis. The development of a wedge-shaped defect lasts for years.
Symptoms of the defect
In the early stages, symptoms of the disease are often not detected. The appearance of teeth changes in the second stage. A thickening appears in the cervical part. At the middle and more clearly at the deep stage the following symptoms are noted:
there is a piercing pain of a short duration; the patient experiences discomfort while eating and brushing his teeth; hypersensitivity of tooth enamel; the cervical region has a pronounced wedge-shaped defect; enamel pigmentation begins; in the deep stage the neck of the tooth becomes exposed
Prevention of wedge-shaped enamel defect
To prevent a wedge-shaped defect, it is necessary to follow the rules of prevention:
visit the dentist regularly for examination; brush your teeth correctly; maintain a balanced diet rich in calcium and fluoride; rinse your mouth after every meal (especially after eating sour foods); correct bite defects in a timely manner; if necessary, install braces for children.
Tooth erosion
Dental erosion is a progressive cup-shaped loss of enamel and dentin on the vestibular surface of first the incisors, and then the canines and premolars of the upper jaw. Occurs in middle-aged people. The cause has not been established. The course is chronic with the gradual involvement of new unaffected teeth. The defects are very painful.
Treatment
The dentist’s task is to stop the destruction of bone tissue, prevent sepsis, and alleviate symptoms.
For this purpose, therapeutic and surgical methods are used, such as:
- Drug therapy
Broad-spectrum antibiotics, antihistamines, and aseptic mouth rinses are prescribed. For pain, analgesics are prescribed.
- Surgical intervention
The doctor performs curettage of pockets or sockets of extracted teeth. Removes sequestration, opens and provides drainage of purulent foci, splints mobile teeth.
Depending on the stage of the disease, an operation is indicated in which the affected bone is completely removed, leaving only its healthy part.
In many cases, reconstructive surgery must be resorted to to fill the defect or correct the deformity. This could be a bone transplant or jaw restoration.
Treatment of jaw necrosis is a multi-step process that requires the participation of several doctors. Depending on the nature of the disease, the dentist works closely with an oncologist or general practitioner. For reconstructive operations under general anesthesia, the participation of an anesthesiologist and an oral and maxillofacial surgeon is required.
Symptoms of tooth erosion
In the initial stage, there is a loss of enamel shine in a limited area of the vestibular surface of the tooth. At this stage, you can notice signs of the beginning of the erosive process only after drying the tooth surface with a stream of air or applying 5% iodine tincture to the affected area - in this case, a yellow-brown coloration of the erosion area occurs.
Initially, the erosive defect is a round or oval cup-shaped lesion with a hard, smooth and shiny bottom. As the lesion expands and deepens, complete loss of the enamel layer and exposure of dentin may occur. With I and II degrees of tooth erosion, the defect has a whitish color; at stage III of the pathological process, light yellow or brown pigmentation appears.
At the initial stage of tooth erosion, with a stabilized course, there is no pain. In the active phase, with moderate and deep degrees, phenomena of hyperesthesia are observed when brushing teeth, the action of chemical and thermal irritants. The most common lesions are symmetrical incisors, canines and premolars. Erosion of enamel is often combined with pathological abrasion of hard dental tissues. The course of dental erosion is chronic, progressive, characterized by gradual damage to new teeth.
Diagnostics
Tooth erosion is diagnosed during a dental examination. A clearer localization of the defect is facilitated by drying the surface of the tooth crown and an iodine test. Tooth erosion requires differentiation from wedge-shaped defects, enamel hypoplasia, and superficial caries.
To identify concomitant endocrine disorders, patients suffering from dental erosion may need to consult an endocrinologist, perform an ultrasound of the thyroid gland, and study thyroid hormones. To exclude GERD, examination by a gastroenterologist is recommended.
What factors provoke it?
The development of this pathology can be influenced by a variety of and completely different factors. Dental tissue necrosis can be provoked by both internal and external causes.
Domestic
Internal factors include the following:
- dysfunction of the central nervous system;
- pregnancy period. As a rule, necrosis was observed with frequent pregnancies following one after another;
- pathologies of the thyroid gland, for example, hypothyroidism;
- imbalance of hormone production (especially in adolescence);
- regular human intoxication;
- genetic predisposition.
Internal factors mainly lead to the occurrence of cervical necrosis .
External
External factors include everything that can negatively affect tooth tissue directly :
- excessive or prolonged exposure to substances containing acids or harsh chemicals. For example, medicines, products, industrial substances;
- receiving high doses of radiation. Most often observed in the treatment of cancer diseases;
- constant exposure to electromagnetic radiation.
Prognosis and prevention
Unlike caries, the development of dental erosion has nothing to do with poor oral hygiene. However, against the background of progression of the erosive defect, secondary addition of carious lesions of the teeth may be observed. Therefore, treatment of dental erosion must be timely and complete. After stabilization of erosion is achieved, patients require clinical observation by a dentist-therapist.
Prevention of dental erosion consists of the correct selection and use of dental care products, limiting the consumption of products with a high erosive potential, and eliminating concomitant endocrine disorders. Using phosphate-containing toothpastes 2-3 times a week is very effective.
Acid necrosis of teeth
Acid necrosis of hard dental tissues is an occupational disease that occurs in people working in the production of inorganic acids. It is assumed that acid vapors reduce the pH of saliva, and the capacity of the buffer systems of the oral fluid and the remineralizing properties of saliva are also reduced. This contributes to rapid wear (abrasion) of the hard tissues of the tooth. Dental damage is widespread and the process develops slowly.
Clinical picture
Acid necrosis of teeth develops slowly. With chemical necrosis, fangs and incisors are more often affected: in the area of the cutting edges, the enamel disappears, resulting in the formation of sharp edges. In the initial stage, patients have a feeling of teeth on edge, and there may also be a feeling of teeth sticking, which is associated with the “washing out” of minerals from the tooth enamel, resulting in a feeling of softness of the teeth when they are closed. In later stages of the disease, pain from temperature and chemical stimuli appears. However, it should be borne in mind that pain may not be observed, due to the fact that tertiary dentin is being produced. As necrosis progresses, the enamel loses its shine, becomes dull and rough. And after complete loss of enamel, dentin becomes pigmented and becomes dark. In advanced cases, complete dissolution and abrasion of the tooth crown may occur.
Differential diagnosis of acid necrosis
Acid necrosis of teeth must be differentiated from enamel erosion. Erosion is characterized by a hard, shiny surface, and with necrosis, softening of the enamel occurs.
Prevention of acid necrosis
Prevention
acid necrosis is to improve working conditions, use individual products, and conduct regular alkaline rinses.
Bruxism in adults
Bruxism
is a disease characterized by involuntary, periodic and very strong (spastic) contraction of the masticatory muscles, as a result of which the jaws are clenched to the point of grinding the teeth. Typically, attacks of bruxism last a few seconds, but sometimes it can last much longer - several minutes. At the same time, the pulse may increase, blood pressure may rise, and the respiratory rhythm may become disrupted.
Bruxism can appear in a person at any time in life. According to scientists, bruxism occurs in 15% of adults and approximately 50% of children (childhood bruxism). However, not every person knows about his illness, since it manifests itself at night. Most often, family members and relatives tell him about this.
Scientists have not yet fully determined the causes of bruxism, which significantly affects the prevention of this disease. There is an opinion that the causes of its occurrence may be somnambulism, severe snoring, and nightmares. This disease usually affects people with pathologies of the facial skeleton and temporomandibular joint. They say that bruxism most often occurs in a person whose life is full of stress and great emotional stress.
The danger of bruxism is that it can:
- provoke increased tooth wear;
- cause loosening and damage to teeth;
- disrupt the correct bite;
- increase tooth sensitivity;
- develop pathology of the temporomandibular joint;
- cause headache;
- cause pain in the facial muscles.
In addition, the consequences of this disease can be various mental disorders, since the patient feels discomfort in communicating with other people.
Types of disease
There are two types of bruxism: daytime and nighttime. Daytime bruxism is characterized by the habit of intensively clenching the jaws at a time of strong emotional stress, which causes teeth grinding. With night bruxism, a person clenches his jaw tightly and grinds his teeth while sleeping. Several attacks can occur in one night. Most patients suffer from this type of bruxism.
You should not worry if attacks of this disease do not last long (about ten seconds) and are repeated irregularly. Overcoming this disease on your own will not be successful. As soon as a person realizes that he is suffering from bruxism, he should immediately consult a doctor for advice and begin timely treatment.
Treatment of bruxism
Correct treatment consists of identifying the cause and eliminating it. Since the nature of the disease is not completely clear, bruxism is treated by a general practitioner, a neurologist and a dentist. People visit the dentist most often because of symptoms that arise in the maxillofacial area.
How can a dentist help in this situation? Make special silicone mouthguards that are worn at night and significantly soften the load on the dental system. The specialist will also eliminate diseases of the temporomandibular joints, restore defects in the dentition with orthopedic structures, and sanitize the oral cavity.