Polyodontia is an abnormal number of teeth.
In medicine, this disease is often called hyperdontia, and “extra” dental elements are called supernumerary teeth. Research is still being conducted into why this pathology occurs. Most scientists associate it with disturbances in the formation of tooth germs.
Nature provides that a person grows no more than 20 milk teeth and 32 permanent teeth in a lifetime, but exceptions occur, and in our time quite often. According to statistics, on average, dental anomalies occur in 2% of the world's population, most often in men.
In 2014 alone, two operations were performed, in one of which 80 teeth were removed, and in the other, a record 232 teeth. Until this time, the maximum figure was 37 teeth.
The most common hyperdontia (anomaly in the number of teeth) is an anomaly of the upper incisors. Supernumerary teeth are less common among the lower incisors and in other parts of the jaw. They can come in a wide variety of shapes and sizes. These are usually small, cone-shaped teeth.
Extra teeth lead to deformation of the dentition, so it is recommended to remove supernumerary elements. Another reason for removal is that most patients with this pathology have a lisp.
The formation of extra teeth is quite common today. According to statistics, 70% of patients have only one extra incisor, in 25% of cases – 2 supernumerary elements, and only 5% of all patients have 3 or more teeth during examination.
How many teeth should a person have?
In fact, 32 is the maximum number of teeth that a person can grow, excluding some diseases when there may be more teeth. However, in life this is not always the case. The process of replacing baby teeth with molars is completed at approximately the age of 14, and there are 28 of them in total. They are divided into the following groups:
- Incisors. They have a sharp, chisel-shaped shape and are located in the front of the jaw (four upper and four lower). Their main function is to bite food.
- Fangs. They have a pointed shape and are designed to grab and tear food.
- Small indigenous. They have two sharp bumps on the chewing surface and are designed for grinding food.
- Molars. They have several tubercles on the upper surface and are designed for grinding food.
In total, their number can range from 28 to 32. What are these 4 lost teeth? They are called molars or, as they are called in medical terminology, third molars. Not everyone grows them and not always in the amount of 4 pieces.
Causes of polyodontia
Medicine has not yet found an exact answer to the question of what are the causes of supernumerary teeth. Scientists put forward several hypotheses:
- Atavism. Supernumerary teeth are explained by the fact that the dental system strives to return to the original number of elements laid down by nature. There is evidence that our ancestors had 6 incisors on both the lower and upper jaws. As a result, many doctors consider atavism to be the cause of the development of polyodontia in humans.
- Splitting of the tooth germ. Even in the embryonic period, the activity of the dental plate is disrupted in the child, as a result of which hyperdontia is formed. Violations can be caused by viruses, poor ecology, drugs, medications prohibited during pregnancy, alcohol and other factors. This hypothesis is increasingly supported today, because recently the disease has been rapidly progressing due to bad habits and poor ecology.
The causes of hyperdontia continue to be researched. Scientists cannot give an exact explanation for this anomaly, but most of them are inclined to the second hypothesis - the splitting of the tooth germ at the embryonic stage.
Complications caused by polyodontia
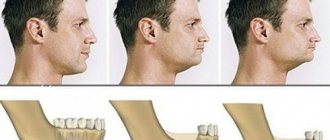
Supernumerary teeth appear more often on the upper jaw in the permanent dentition, and are less common on the lower jaw and in the primary dentition. Their appearance threatens with the following complications:
- Development of anomalies of the dental system: change in the position of complete teeth: their displacement to the sides, forward or backward, rotation around an axis;
- bite deformation, as a result – disruption of chewing and speech functions;
- disruption of the eruption of permanent teeth, up to the loss of their ability to erupt;
- the appearance of a diastema - a pathological distance between the central incisors;
- the formation of three spaces between the remaining teeth.
- chronic gingivitis;
The eruption of supernumerary teeth is often accompanied by the following symptoms:
- increased body temperature;
- pain and swelling in the eruption area;
- increased salivation;
- swelling of the nasal mucosa.
Supernumerary teeth affect not only the visual component of the smile, but also cause systemic disorders that lead to deterioration in chewing food and disruption of the stability of the main teeth. All this also affects a person’s psychological comfort: he becomes withdrawn, does not smile, so as not to demonstrate smile defects.
What does polyodontia look like?
Quite often, extra teeth are almost indistinguishable from normal ones. It is not uncommon for them to grow in the form of a drop or a thorn. These dental elements can appear either individually or fused with permanent ones. They can form tooth-like formations and entire arrays of teeth.
Also in medical practice, there are cases where polyodontia was hidden and was detected only by radiography. There are many different cases of abnormal development of the number of teeth, and if you notice symptoms, you should definitely contact the dentist.
Types of polyodontia disease
Polyodontia in the oral cavity manifests itself in different ways. By studying the statistics, signs and symptoms of the disease, dentists were able to classify the types of this anomaly.
Depending on the origin, the disease is divided into two types:
- False polyodontia. Provides for a baby tooth that does not fall out, regardless of the person’s age. At the same time, it fulfills its functions, does not create discomfort to the bite, and is firmly fixed in the patient’s jaw. In addition, teeth fused together and other anomalies are classified as a false type of disease.
- True polyodontia. It can be caused by genetic predisposition, as well as terogenic factors. At the same time, extra molars begin to form in the human jaw.
As for the placement of extra teeth, dentists distinguish the following types of disease:
- Typical hyperdontia. Applies to those patients in whom extra teeth appear only in the dentition and do not extend beyond it. Many scientists are confident that this is simply heredity, because our ancestors had a more developed dental system than modern people.
- Atypical hyperdontia. It occurs much less frequently and is characterized by the appearance of teeth outside the dentition.
In case of anomalies with baby teeth, the latter pose almost no threat. On the contrary, such a tooth can last a lifetime. But the permanent molars, over which the supernumeraries grow, should be removed, if only because it is not aesthetically pleasing.
Often, the patient grows extra fangs or incisors, or even several front teeth at once. In addition to a ruined smile, the disease can cause serious complications if the necessary measures are not taken in time.
You probably have 28 teeth or even all 32. And their importance for the body is much greater than simply chewing food.
When it comes to teeth, we usually focus on aesthetic aspects. Straight white teeth are a status symbol, and many people pay top dollar for it. The teeth straightening and whitening industry is growing rapidly.
“We don’t just have white teeth in our mouths. The surrounding tissue is also important and must be looked after to reduce the risk of a wide range of diseases,” says Björn Klinge, senior lecturer and chief periodontist at the Faculty of Odontology at Malmö University.
The mouth is often viewed as a part of the body, separate from the rest of the body. This is absolutely not true - there is a close connection between them. However, the connection between oral health and diseases of other organs is not direct. This is a complex medical field. Bacteria in the mouth can, for example, affect a particular organ for years before a diagnosis can be made. Several factors play a role in the development of the disease.
But in a nutshell, it all starts with bleeding gums.
Ilta-Sanomat 09/03/2021 Sabah 03/28/2021 Milliyet 03/13/2021 Keji Daily 01/04/2021
If you see blood when you brush or floss your teeth, it's most likely bacteria. They probably accumulate and multiply in the space between the tooth and gum. A protective reaction is triggered in the gum: it swells, which, unfortunately, only complicates access to bacteria.
“Nothing hurts you. At best, you will notice blood while brushing your teeth - this is a signal that it is time to improve your oral hygiene,” says Björn Klinge.
Imagine a wound on your hand. If it does not heal and infection begins, few people will turn a blind eye to it. But when this happens in the mouth, it is much easier to ignore the infection.
If bacteria get to the edge of the gum or even into a tooth pocket, the infection can spread lower - to the tissues that fix the periodontium. In this case, your dentist frowns with concern and makes a diagnosis of periodontitis.
Chronic periodontitis affects approximately 40% of Swedish adults. Due to the disease, they lose fragments of the tissue that holds the roots of the teeth in the gums. Extensive degradation of this tissue occurs in 7-20 percent of cases, according to the Swedish National Commission for Health and Social Assessment. In Swedish, periodontitis is often referred to as “tooth loss,” and this can be confusing. In fact, teeth begin to become loose and fall out only in the late stages of the disease.
Periodontitis
Periodontitis affects up to 40% of adults. From 7% to 20% of cases lead to widespread tissue damage.
In other words, four out of ten people have periodontitis, according to the Swedish National Commission for Health and Social Assessment.
It has been known for more than 30 years that periodontitis is more common in patients with cardiovascular disease.
“However, it is difficult to establish whether there is truly a cause-and-effect relationship between cardiovascular disease and periodontitis, or whether it is due to other associated risk factors such as smoking, diabetes or poor socio-economic status,” says Anna Nurhammar. Norhammar, visiting professor specializing in cardiology at Karolinska Institutet.
The periodontal pocket is one of the few pathways leading to the body’s circulatory system. That's why scientists thought about the existence of a connection between diseases of the teeth, heart and blood vessels. In this way, bacteria from the oral cavity can enter the body and cause inflammation in one or another part of it.
To study the connection between periodontitis and myocardial infarction, researchers at the Karolinska Institutet conducted a large study called Parokrank. Cardiologists, odontologists and epidemiologists worked together. Data from about 800 patients who had their first heart attack were compared with data from a corresponding number of people who had not had a heart attack. Gender, age and place of residence were taken into account. Everyone had their teeth x-rayed.
“We found that severe periodontitis was more common in patients with a history of heart attack, even after taking into account additional factors such as smoking, diabetes and education level. In other words, our study clearly indicates an association between periodontitis and myocardial infarction. Now we are continuing our work to find out whether patients with periodontitis are more likely to have cardiovascular problems than other study participants. Our goal is to establish a direct cause-and-effect relationship, if there is one,” explains Anna Nurhammar.
In the first part of the study, the researchers also found that subjects with severe periodontitis were more likely to have previously undiagnosed diabetes.
“It has long been known that periodontitis is more common in diabetics, and diabetes often increases the risk of periodontitis when blood sugar levels are poorly controlled. As it turns out, this also applies to people with undiagnosed diabetes.”
Our teeth
Permanent teeth usually begin to grow at age six. At the age of 12-13, large molars appear, and the total number of teeth reaches 28. But not everyone - every tenth resident of Scandinavia is missing one or more permanent teeth.
Wisdom teeth do not appear until the age of 18. If all four have grown, then a person has 32 teeth. But approximately every fourth person is missing one or more wisdom teeth - simply because there is not enough space in the jaw.
However, introducing screening for hidden diabetes during a visit to the dentist is not the best idea, because dentistry is a completely separate specialization.
“Based on the results we obtained from the Parokrank study, we can recommend that those suffering from severe periodontitis see a GP and be checked for the risk of cardiovascular disease and diabetes. And for those who have had a heart attack, it wouldn’t hurt to go to the dentist and look for signs of periodontitis,” says Anna Nurhammar.
Daily Mail 09/21/2020 Sohu 07/18/2020 Al-Ain 07/05/2020 Huanqiu shibao 01/07/2020
Scientists are still debating whether periodontitis should be considered a separate risk factor. Be that as it may, oral health is closely related to general health, the specialist emphasizes. First of all, if a severe tooth infection or other infections in the mouth are left untreated, bacteria can enter the bloodstream and settle on the heart valves, especially if the valve is worn, sclerotic, or does not close completely. Bacteria also get on artificial valves and pacemakers. In such cases, the infection must be treated with heavy antibiotics for several weeks.
And for people with type 2 diabetes, oral health is especially important.
“When periodontitis is cured, a diabetic’s blood sugar level drops, this is a proven fact,” notes Björn Klinge.
Varieties of rheumatism and even some types of cancer can be associated with oral health.
“In-depth research is now being carried out in these areas, and each of them adds another piece of the puzzle to the overall picture, which in the end will probably reveal that oral health causes a whole range of other diseases. This can probably be explained by the fact that constant inflammation in the mouth weakens the body's immune defenses. In addition, the bacteria that cause this inflammation can reach other organs through the saliva we swallow or through the blood,” says Björn Klinge.
The list of diseases that are caused by poor oral hygiene can be extended. “But so far science only speaks of a potential connection. If you want a concrete answer to the question of whether bad teeth cause other diseases, I can’t say “yes” right now,” adds Björn Klinge.
The only way to establish a cause-and-effect relationship between bad teeth and diseases of other organs would be a study in which participants in a separate control group were deliberately not treated for periodontitis. And this would be extremely unethical, so you shouldn’t expect anything like that.
Scientists are digging deeper and deeper in search of answers. The pandemic has made the question of how exactly viruses trigger diseases against the background of inflammation in the mouth especially relevant. Saliva is a dangerous carrier of COVID-19, notes Björn Klinge.
If you're already getting a stomach ache just thinking about how your mouth can affect the rest of your body, Björn Klinge's advice will help put your mind at ease.
- Do not smoke. Smoking aggravates the damage to root tissues during inflammation during periodontitis.
— Brush your teeth in front of the mirror. The gums are swollen and red, which means there is inflammation. If you find such signs - and they are more reliable than bleeding - think about how to improve your oral hygiene.
- Several weeks have passed and your gums are still swollen, red and bleeding? So, it's time to make an appointment with the dentist.
InoSMI materials contain assessments exclusively of foreign media and do not reflect the position of the InoSMI editorial staff.
Symptoms of the disease in children
The first supernumerary teeth in children appear before birth or in the first six months of life. The main inconvenience they cause is difficulty in feeding.
Polyodontia of primary teeth in older children occurs with symptoms similar to the eruption of regular teeth. In this case it is observed:
- temperature increase;
- swelling of the gums in the place where the tooth should erupt;
- pain;
- excessive salivation;
- swelling of the nasal mucosa;
- loose stool.
Symptoms are especially severe when extra teeth appear in the upper palate.
If hyperdontia makes itself felt in a two-year-old child, this can interfere with the formation of normal speech. In turn, due to injury to the tongue and mucous membranes, some kind of inflammation constantly appears in the oral cavity.
When supernumerary teeth appear in very noticeable places in school-age children, ridicule towards the patient may occur, which is fraught with the development of psychological problems and complexes in the future.
Polyodontia (supernumerary teeth) - symptoms and treatment
For a successful prognosis in treatment, high-quality and timely diagnosis of patients is very important. The dentist-therapist must know the basic clinical manifestations and principles of diagnosing hyperdentia. This is especially important in the work of a pediatric specialist during periods of medical examination and planned sanitation of the oral cavity in children. This makes it possible to identify the presence of this anomaly at an early age and carry out appropriate treatment in the early stages.
Most often, “extra” teeth are located in the anterior part of the upper jaw. The question of the exact location of supernumerary teeth is very important, since the surgical stage of treatment depends on this. The more accurately the position of various anatomical formations is determined, the less surgical trauma (damage to the growth zones of complete teeth, the formation of large defects in the bone of the alveolar process) will result from the surgical stage of treatment. The volume and time of the procedure will be reduced, which is very important when it comes to treating children. The position of the causative tooth can be determined using instrumental examination methods:
- CT scan;
- orthopantomography;
- intraoral radiography;
- visiography;
- Magnetic resonance imaging.
Computed tomography allows you to obtain a cross-sectional, layer-by-layer image of any area of the human body, including the skull. Dental (dental) X-ray computed tomography allows you to make 4 types of images in different planes in one and a half minutes. The radiation dose with this examination method is less than other types of CT. The procedure is easily tolerated by patients and does not require special training, which is convenient when working with children. In addition, it is as informative as possible for the doctor.
Orthopantomography is a method of x-ray examination in which you can obtain an image of all the patient’s teeth, upper and lower jaws, adjacent tissues and areas of the facial skeleton. Conducted for children from 3-4 years old. This is a quick, simple, highly effective method that helps identify oral diseases in the early stages. It has virtually no clinical contraindications and is actively used by dentists.
Intraoral radiography is the simplest, most common diagnostic method in therapeutic dentistry. The picture shows from one to 3-4 teeth and adjacent formations. For the pathology under consideration, the method is not informative enough, but can be used if the above types of diagnostics are unavailable.
Visiography is a system for obtaining X-ray images without the use of film. In this type of research, instead of film, a special sensor is used, from which the image is transferred to a computer, after which it is processed and then saved. Advantages of this technique:
- The radiation exposure to the patient is tens of times lower compared to the most advanced film X-ray, which is extremely important for both the patient and the radiologist.
- Scalability and the possibility of mathematical image processing (measuring the size, density of objects, etc.).
- It is possible to store the received information and create your own database for each patient.
- There is the possibility of instant transfer of diagnostic data directly from the treatment room to the computer monitor of the attending doctor, wherever he is. This is very convenient if you need to consult doctors from different clinics or from different cities.
But, as with intraoral radiography, the image produces a low-informative planar image of the area under study, limited to 1-4 teeth.
Magnetic resonance imaging is a radiation diagnostic method that can be used to obtain an image of the layers of the human body in any plane. The method is simple and does not have any harmful effects on the body of the subject. A contraindication for MRI is the presence of metal foreign bodies (dentures, braces, surgical pins, etc.) in the patient’s body.
Sometimes, to determine the level of location of problem teeth, Yu.I.’s technique Zhigurta (1994). It consists of studying an orthopantomogram of the jaws and marking on it the four levels of occurrence of unerupted incisors and canines. However, this method is imperfect and does not allow an accurate assessment of where the supernumerary tooth is located. It is more advisable to use modern diagnostic methods described above.
To more accurately determine the relationship of the additional tooth with the roots and rudiments of the complete teeth, contact intraoral radiographs are taken in the preoperative period and 1, 3, 6 and 12 months after the operation. They are used to determine the degree of change in the position of the impacted tooth, the condition of the root of the complete tooth and the morphological structure of the bone of the alveolar process in the studied area [1][7][8].
Symptoms of hyperdontia in adults
Polyodontia affects permanent teeth more often than baby teeth. An adult usually develops dystopic and impacted supernumerary teeth.
Dystopic teeth are those that appear outside the dental arch. Most often they erupt on the lingual surface of the gums and in the palate. With this form of the disease, the patient typically:
- poor pronunciation of sounds;
- noticeable malocclusion;
- change in the usual arrangement of teeth: curvature of the angle at which they grow, as well as their rotation
- around its axis;
- frequent injury to the oral mucosa and, as a result, its inflammation;
- disruption of chewing processes, resulting in digestive problems.
Among other things, dystopic teeth often cause psychological problems. Due to a non-aesthetic, and sometimes completely unattractive smile, the patient becomes withdrawn and uncommunicative. Psychological problems, in turn, cause chronic diseases of the endocrine, digestive and nervous systems.
Impacted supernumerary teeth are teeth that do not erupt, but continue to remain in the bone tissue of the human jaw. Often they hardly make themselves felt until complications begin. Dentists diagnose this anomaly during a routine examination of the patient.
This abnormality in the number of teeth is accompanied by the following symptoms:
- normal teeth begin to loosen (the condition is considered pathological);
- the bone begins to protrude (if the impacted tooth is too close to the edge of the jaw);
- Aching pains appear periodically.
One of the most difficult situations is when extra teeth grow in place of impacted third molars. Wisdom teeth cannot grow and begin to negatively affect the roots of other teeth, which in turn can lead to serious complications.
What should a parent be wary of in this case?
The strange shape of the erupted tooth, as well as its position in the dentition.
In adults, as a rule, there are no symptoms. Supernumerary teeth simply erupt and create discomfort, injuring the mucous membrane and making the bite incorrect, or they remain in the bone tissue without showing themselves.
In some cases, if there are impacted extra teeth, an adult may have:
- loosening of permanent units,
- periodic discomfort at the location of the extra tooth,
- bone deformation if the tooth is located at the edge of the jaw.
Consequences of polyodontia disease
Polyodontia in humans can often be the cause of retention. This is a phenomenon in which normal teeth are unable to erupt due to the interference of supernumerary teeth. The former may remain in the jaw or take an abnormal position.
In addition, even if the complete incisor grows before the supernumerary one, the latter will be able to displace it. This will lead to the person being unable to chew food normally. And if several extra incisors grow at once, they can cause the loss of permanent teeth.
Consequences
Untimely or improper treatment of hyperdontia can cause serious consequences, the correction of which may take a long time:
- severe malocclusion;
- speech defects that cannot be corrected;
- constant injury to soft tissues leads to chronic inflammation with a high risk of developing benign and malignant neoplasms in the oral cavity;
- Impacted teeth are a common cause of chronic osteomyelitis of the jaw.
The lack of correction of hyperdontia in children is especially dangerous, since it often causes disturbances in the correct formation of jaw tissues. Supernumerary teeth can cause the death of the rudiments of permanent teeth or their improper eruption.
Therefore, if there are any signs indicating the appearance of excess dental elements, or if impacted teeth are detected, you must urgently seek advice from a dentist!
Diagnostics
Examining supernumerary teeth during an x-ray is not as easy as it seems. They can be superimposed along the contour onto the permanent ones and remain invisible. In such cases, patients are recommended to undergo a computed tomography scan, which shows a more accurate picture of the disease.
If the extra dental elements have already erupted, the dentist can easily detect them. In practice, the patients themselves find the erupted supernumerary teeth and already at the initial appointment with the dentist they complain about the pathology.
When should supernumerary teeth be removed?
Reasons for removal may vary: from aesthetics to obvious damage to the health of the main dentition. Therefore, it makes sense to remove excess teeth if:
- There is a risk of losing a permanent healthy tooth.
- Retention of normal dental units is possible.
- Supernumerary teeth are carious or affected by other pathologies.
- Polyodontia distorts the normal dentition and spoils the smile with its unaesthetic shape and location in the mouth.
- Due to the growth of abnormal teeth, bite and diction are impaired, and the mucous membrane is injured.
- Threat of resorption of permanent row roots.
- The germ of an extra tooth produced a cystic formation.
When supernumerary teeth are “not conspicuous”, do not cause discomfort, and do not harm the normal dentition, then, in principle, they can be left alone. But still, in order to finally make a decision, careful studies using X-rays and computed tomography are needed, as well as consultation with an experienced specialist, so as not to miss any hidden problems from this dental pathology.
Symptom relief
Most often, in adults, extra teeth erupt without any symptoms, but for children this can become a problem that needs to be addressed.
Supernumerary teeth erupt with the same symptoms as regular teeth, so the treatment for them is the same.
- To lower the temperature, it is recommended to give your baby Paracetamol or Ibuprofen. If the child is very small, these drugs can be used in the form of suspensions or rectal suppositories. In addition to lowering the temperature, these medications do an excellent job of treating pain and inflammation.
- To relieve gum pain, local anesthetics are used - ointments and gels (for example, Kalgel, Dentinox, Solokoseryl). These remedies cope well with painful sensations and slightly relieve inflammation.
- Adults and children over 2 years of age can be treated with folk remedies: propolis, honey, decoctions of calendula, chamomile and lemon balm. Some decoctions help reduce pain and relieve inflammation. Traditional methods of treatment should be used only after consultation with your doctor.
- If primary supernumerary teeth have partially erupted, stimulation of eruption is prescribed. For this purpose, vibration and electrical stimulation, as well as special massage, are used.
Normal deletion
If the dentist decides that in a particular case, polyodontia can only be treated by removing an extra tooth, the patient should count on the following procedures:
- First of all, the patient should be sent for radiography. This is necessary in order to determine the size and number of roots, as well as the ratio of supernumerary and normal teeth.
- After collecting research, the doctor gives the patient anesthesia and removes excess teeth.
- In some cases, soft tissue sutures may be necessary after surgery.
Removal of impacted teeth
In order for the operation to be successful and polyodontia to be cured without any complications, the doctor must fully examine the patient and plan his further actions.
- To begin with, X-rays and/or computed tomography are performed to determine the exact topography of the anomaly.
- Removal is performed under local anesthesia, but there are cases when general anesthesia can be used on the patient.
- First, the mucous membrane is peeled off, then the bone tissue is opened and the root and crown parts of the tooth are removed.
- If necessary, bone defects are covered with osteoplastic material, and the mucous membrane is sutured.
After tooth extraction, the patient continues treatment at home: takes antibiotics (if prescribed by the attending physician), rinses the oral cavity with antiseptic solutions.
Until the wound heals after surgery, it is not recommended to eat too hot, hard or spicy food. You should also brush your teeth carefully, especially on the operated side.
Treatment
Relief of teething symptoms
Teething may be accompanied by the usual symptoms for this process: pain, itching, swelling of soft tissues, and sometimes fever; Children are especially sensitive to the teething process. To relieve symptoms use:
- Nonsteroidal anti-inflammatory drugs: paracetamol, ibuprofen. They are taken orally to reduce fever and reduce inflammation.
- Products for topical use: gels Dentol, Dentinox-N, Kamistad. The products are applied to the teething area and have analgesic and anti-inflammatory effects.
- From the age of three, rinsing with propolis tincture is allowed: 15 ml of tincture is diluted in 100 ml of warm boiled water, rinse the mouth up to five times a day.
- It is advisable to consult a doctor.
Tooth extraction
As a rule, the treatment of polyodontia consists of the removal of supernumerary teeth, which is carried out under local or general anesthesia. Extraction of an erupted, evenly positioned supernumerary tooth is usually not difficult; removal of impacted teeth is difficult. In this case, the surgeon makes an incision in the soft tissue to access the tooth, then saws it out of the bone tissue, completely removing it. After this, biomaterial is placed into the hole to restore bone tissue, and the wound is sutured.
Removal of a supernumerary tooth can be complicated by the proximity of its roots to the roots of permanent teeth, the large depth of the tooth and the irregular shape of the tooth being removed. Data from studies conducted using computed tomography provide great assistance in choosing a removal technique and making a treatment prognosis.
To avoid serious disorders of the dental system, it is advisable to visit an orthodontist. And children are recommended to have a consultation for prevention from the age of 3.
Sometimes, in order to prevent injury to the tooth germs of adjacent teeth, it is necessary to delay the removal of supernumerary teeth until they have fully or partially erupted. A delay is indicated if the extra teeth, when erupting, do not cause changes or deformations in the jaw bone.
It happens that supernumerary teeth have a normal shape and a well-developed healthy root, while the permanent tooth is damaged, incorrectly positioned or susceptible to retention (delayed eruption). If an X-ray examination confirms the futility of a complete tooth, it is removed, leaving the supernumerary one.
Orthodontic treatment
This type of treatment is usually required for children and adults with existing pathology to restore normal jaw development and correct the bite. Also, the help of an orthodontist will be required to place a supernumerary tooth into the dentition if a decision was made to replace a complete tooth that was removed for some reason.
To correct any abnormalities, braces are used, which the doctor selects individually for each patient. The braces system consists of locks that are attached to the teeth and connected to each other by a metal arch that maintains a given shape. While wearing an orthodontic device, under the influence of the arc force, the teeth take the correct position, the smile becomes even and beautiful. Dental plates are made for children at a young age. The sooner the problem is identified and measures taken, the faster the solution will be.