Gum inflammation
Recommended Articles
- Causes of gum inflammation
- Types of inflammation
- Main manifestations and symptoms
- Diagnostic features
- Treatment methods
- Prevention methods
Gum inflammation is a general concept that includes both superficial and deep inflammatory processes. Everyone faces this problem to one degree or another, and in the absence of proper attention to the condition of the oral cavity, inflammation can lead to serious consequences, including the loss of healthy teeth. It is important to recognize in time not only the onset of inflammation, but also to assess the depth of its spread, receive qualified dental care and prevent complications.
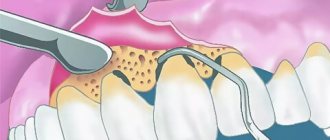
Surgical method of treatment
One of the most expensive, but no less effective methods of treatment is surgery. With the help of certain materials and special membranes that are planted under the gum, bone tissue growth is achieved. As a result of a productive course of treatment, it is possible to achieve the creation of an alveolar process, with the help of which it is possible to fix loose teeth. To restore gums, several types of cells are used: fibroblasts (accelerate the production of collagen, which improves tissue elasticity and increases the protective properties of the oral mucosa), stem cells (produce new mucosal tissue), and platelet growth factors (protein compounds to strengthen and restore blood vessels blood and lymph).
Gingivitis
This is the first and reversible stage of periodontitis. Gingivitis is inflammation of the gums. This disease is very dangerous during pregnancy - due to changes in the hormonal levels of the pregnant woman, the disease progresses faster than usual, can lead not only to the loss of teeth in the pregnant woman herself, but also cause dental problems in the future in the child, and even provoke premature birth.
If you notice the following signs, then most likely these are symptoms of developing gingivitis:
gum inflammation, bleeding,
bright red gum color,
pain and swelling in the gum area,
bad breath, quickly forming plaque and stones.
Antibiotics after tooth extraction
One of the surgical operations in dentistry is the removal of wisdom teeth. Antibiotics in the preoperative period are prescribed for prophylactic purposes to patients with glomerulonephritis, endocarditis, diabetes mellitus, and those with weakened immune systems. Prevention is possible with planned removal, which is carried out in case of atypical position and mobility of the unit, in case of chronic cysts and periodontitis, in case of mechanical damage without the possibility of recovery after sanitation of the oral cavity.
An antibiotic is also prescribed after tooth extraction if the operation is performed as an emergency. More often, Ciprofloxacin. What antibiotics to take after tooth extraction is prescribed by the dentist, taking into account the specifics of the microflora. The main indications for such removal are acute purulent inflammatory diseases localized to bone tissue, abscesses, lymphadenitis, and phlegmon. Antibiotics are used for tooth extraction if it is not subject to conservative treatment, including filling, due to extensive destruction and loss of functionality.
Antibiotics for wisdom tooth removal are prescribed if the integrity of bone or soft tissue was damaged during the procedure, which in the future can provoke infection, inflammation, and the formation of gumboil. Antibiotics after wisdom tooth removal are prescribed for the following complications:
- Alveolitis. It develops 3-4 days after surgery and is characterized by a dry gray lump with a whitish coating. The pathology is characterized by an unpleasant odor, pain, swelling of the cheek, and an increase in temperature to 38-39 °C.
- Apical periodontitis. Periodontal inflammation of an infectious, traumatic or medicinal nature is treated comprehensively. It is necessary to ensure the outflow of exudate, prescribe broad-spectrum antibiotics, antiseptic treatment, and filling the canals.
- Osteomyelitis. A purulent-necrotic process caused by pyogenic bacteria and mycobacteria. With this pathology, hospitalization is necessary. How and what antibiotics to take for this pathology after tooth extraction will be prescribed by the leading doctor.
Cost of periodontal disease treatment
The price of periodontal disease treatment depends on the following factors:
- volume of lesion;
- type of periodontal disease;
- forms of the disease;
- general condition of the oral cavity;
- chosen type of treatment.
On average, periodontal treatment in a good clinic costs from 1000 rubles per tooth. The total price of therapy is calculated individually. To find out the cost of effective treatment in a particular case, sign up for a consultation with a 32 Dent dentist.
Types of inflammatory and dystrophic gum diseases
Inflammatory manifestations include:
- Gingivitis
- Periodontitis
Dystrophic manifestations include:
Gingivitis: signs, causes and treatment
Gingivitis is the first stage of inflammation, in which the integrity of the periodontal junction has not yet been compromised. This disease can be identified by the following signs:
- Swelling of the gums.
- Blood while brushing teeth.
- Pain when eating cold, hot or solid foods.
Improper brushing of teeth, errors during fillings and dentures, improper bite – all this can cause gingivitis. By the way, this is one of the most popular problems that pediatric dentists encounter.
Treatment of gingivitis involves a set of procedures carried out in a dental clinic and at home. If there is dental plaque, it is necessary to carry out ultrasonic cleaning. In addition, you should pay more attention to hygiene: brush your teeth properly and use antibacterial agents.
Periodontitis
Periodontitis is a pathology that occurs as a result of advanced gingivitis. In this case, the swelling of the gums becomes even stronger, they begin to bleed frequently. If left untreated, infection and pus may form. As a result, the bone tissue begins to atrophy, and this leads to increased sensitivity of the teeth, their mobility, and sometimes even loss.
Treatment of periodontitis is prescribed taking into account the course of the disease. At first, procedures such as removing plaque from the enamel and regular brushing of teeth with antiseptic agents may be sufficient. In more serious situations, when the infection has penetrated deep into the bone tissue, surgery may be necessary:
- Partial gum excision.
- Cleaning periodontal pockets.
- Implantation of bone tissue substitutes.
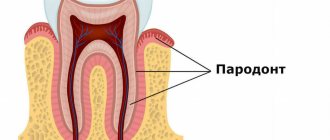
Periodontal disease
Periodontal disease is a systemic disease. As a rule, it is typical for elderly patients. Inflammatory-dystrophic manifestations in this case are concentrated in the periodontal tissue.
Periodontal disease develops at a leisurely pace, gradually erasing tooth enamel. The presence of this disease can be determined by exposed tooth roots and cervical chips of tooth enamel. In most cases, no pain occurs, but if you ignore the problem, you can “lose” your teeth.
To eliminate periodontal disease, it is necessary not only to observe and treat the dentist, but also to related specialists.
Treatment of inflammation at home
The course of treatment of teeth and gums is always selected taking into account the individual characteristics of the disease:
- A type of inflammatory process.
- Neglect of pathology.
- Patient's age.
For example, in adult patients, inflammatory processes most often occur due to chronic diseases. To eliminate the problem, as a rule, pharmaceutical products are required - antiseptics, gels, ointments, antibiotics, toothpastes. If a child’s gums become inflamed, this is almost always associated with teething and herbal medicine, that is, rinsing with herbal decoctions and using other methods of traditional medicine, is sufficient for treatment.
Whatever the situation, adequate treatment is only possible after consultation and diagnosis by a qualified doctor. Remember that the wrong choice of procedures can not only fail to produce results, but also cause painful complications.
Antiseptics
Rinsing with antiseptic agents is the most important step in the fight against inflammatory processes. Let's name well-proven drugs that can be purchased at the pharmacy:
- Malavit - reduces inflammation and prevents its development, but does not eliminate pain effectively enough.
- Kamistad – recommended in the presence of severe pain. It also copes well with swelling.
- Chlorhexidine is a suitable treatment for gingivitis in children. Daily rinsing after meals is recommended.
- Listerine is a good drug for eliminating swelling. Suitable for all types of gum inflammation.
- Stomatophyte is an antiseptic made from natural raw materials: chamomile flowers, oak bark and sage leaves.
- Furacilin is an excellent antimicrobial agent. Penetrates inside the microbial cell, preventing its division.
- Miramistin is an anti-inflammatory drug with a pronounced antimicrobial effect.
Gels and ointments
Therapeutic gels and ointments are applied to the inflamed gums after rinsing with antiseptic agents. They provide effective protection to the mucous membrane, preventing infection from entering wounds and helping to cope with pain.
List of the most effective gels and ointments:
- Metrogyl Denta is a powerful antiseptic gel. It has pronounced anti-inflammatory and analgesic properties.
- Cholisal is one of the best options for combating inflammation that occurs due to internal reasons. Relieves pain well.
- Kamistad - suitable for both preventing gingivitis and combating complications (severe swelling, pain).
- Gengigel is an excellent healing agent. Improves blood supply, promoting rapid healing of wounds in the oral cavity.
- Stomatophyte A – recommended for severe and prolonged pain.
- Asepta - contains propolis, which provides accelerated tissue regeneration and reduces inflammation.
- Solcoseryl is a healing agent with a pronounced anesthetic effect.
Vitamins and minerals
To restore damaged tissues, the body needs a wide variety of nutrients, which are not always contained in the required quantities in the daily diet. That is why the drug treatment regimen for periodontal disease often includes taking vitamin complexes. The best effect can be achieved by taking special complexes, for example, the vitamin-mineral complex for teeth ASEPTA.
The ASEPTA complex includes a whole range of substances necessary to strengthen gums and teeth. Vitamin C strengthens the walls of capillaries and blood vessels, helping to improve blood circulation in the gums, disruption of which is one of the main causes of periodontal disease. Vitamins B3 and B6 help reduce gum sensitivity, strengthen bone tissue and promote healthy mucous membranes. Vitamin A is involved in all metabolic processes occurring inside the body and increases protection against inflammatory and infectious diseases that often accompany periodontal disease.
In addition to vitamins, the complex also contains green tea extract - a natural component that has an antimicrobial effect, eliminates unpleasant odors, and slows down the aging process of tissues. An equally important component of the complex is coenzyme Q10, a substance that is a rich source of energy for the growth and restoration of cellular structures. Taking coenzyme promotes accelerated regeneration of damaged gums.
The complex also includes substances intended to strengthen the hard parts of the tooth, which are subject to increased stress during periodontal disease - coral calcium, which is well absorbed by the body, and vitamin D3, necessary for the proper absorption of calcium and phosphorus.
Description
Compound
active ingredients: metronidazole benzoate, chlorhexidine digluconate
1 g of gel contains metronidazole benzoate in terms of metronidazole 10 mg, chlorhexidine digluconate solution 20% in terms of chlorhexidine digluconate 0.5 mg
excipients: carbomer, propylene glycol, sodium saccharin, trilon B (trilon B), triethanolamine, peppermint oil, purified water.
Dosage form
Basic physical and chemical properties:
gel is white or almost white in color with a specific odor. It should be uniform in appearance.
Pharmacological group
Products for use in dentistry . Antimicrobial and antiseptic agents for topical use in dentistry.
Pharmacological properties
Antimicrobial combination drug for the complex treatment and prevention of certain infectious and inflammatory diseases of the oral cavity.
The effectiveness of the drug is due to the presence of two antibacterial components - metronidazole and chlorhexidine.
Metronidazole is a nitroimidazole derivative that has antiprotozoal and antibacterial effects. Active against anaerobic bacteria that cause periodontal diseases: Porphyromonas gingivalis, Prevotella intermedia, Prevotella denticola, Fusobacterium fusiformis, Wolinella recta, Eikenella corrodens, Borrelia vincenti, Bacteroides melaninogenicus, Selenomonas spp.
Chlorhexidine is a bactericidal antiseptic. Active against a wide range of vegetative forms of gram-negative and gram-positive microorganisms, as well as yeast, dermatophytes and lipophilic viruses.
The minimum inhibitory concentration (MIC50) of metronidazole for anaerobic bacteria is below 1 μg/ml. When applied topically (applied to the gums), the concentration of metronidazole in the gum area is significantly higher than when the drug is administered orally, and the level of systemic absorption of metronidazole when applied topically is significantly lower than when administered orally. The main route of excretion of metronidazole and its metabolites is the kidneys. Reduced renal function does not alter the pharmacokinetics of a single dose of metronidazole.
If excess chlorhexidine is ingested, when applied topically as part of a dental gel, about 1% of the dose that enters the stomach is absorbed from the digestive tract. Chlorhexidine does not accumulate in the body and is minimally metabolized.
Treatment of periodontal disease - effective techniques
- removal of dental plaque by professional cleaning (air flow, laser, ultrasonic, mechanical);
- drug treatment (taking immunomodulatory, hormonal drugs, antibiotics);
- local therapy (rinses with antiseptic solutions, applications using anti-inflammatory gel);
- injections into the gums, when vitamins, antitoxic serums, and antibiotic-containing compounds are injected;
- physiotherapy (darsonvalization, laser treatment, electrophoresis, use of vacuum), aimed at actively supplying the gums with oxygen.
Metrogyl Denta - composition and release form of the drug
The drug is available in the form of a white or almost white gel. Active ingredients : metronidazole benzoate, chlorhexidine gluconate.
1 gram of gel contains: metronidazole benzoate - 16 mg (in terms of metronidazole 10 mg); chlorhexidine gluconate solution (20%) (2.5 mg, based on chlorhexidine gluconate 0.5 mg).
Excipients : saccharin, sodium hydroxide, disodium edetate, levomenthol, propylene glycol, carbomeric homopolymer (type C), purified water.
Dosage regimen
The gel is intended for topical use in dentistry only.
For adults and children over 6 years of age with gum inflammation (gingivitis), Metrogyl Denta ® is applied to the gum area in a thin layer with a finger or with a cotton swab 2 times a day. After applying the gel, you should refrain from drinking and eating for 30 minutes. It is not recommended to wash off the gel. The duration of treatment is on average 7-10 days.
In case of periodontitis, after removing dental deposits, periodontal pockets are treated with Metrogyl Denta ® gel and the gel is applied to the gum area. Exposure time - 30 minutes. The number of procedures depends on the severity of the disease. In the future, the patient can apply the gel independently:
- Metrogyl Denta ® is applied to the gum area 2 times a day for 7-10 days.
For aphthous stomatitis, Metrogyl Denta ® is applied to the affected area of the oral mucosa 2 times a day for 7-10 days.
To prevent exacerbations of chronic gingivitis and periodontitis, Metrogyl Denta ® gel is applied to the gum area 2 times a day for 7-10 days. Preventive courses of treatment are carried out 2-3 times a year.
To prevent post-extraction alveolitis after tooth extraction, the hole is treated with Metrogyl Denta ® gel, then the gel is applied 2-3 times a day for 7-10 days.
Non-surgical adjuvant therapy for the treatment of periodontal diseases
Periodontal disease is an umbrella term used to describe an infectious inflammatory process that can affect one structural element or a complex of periodontal elements. The structures that support the tooth are alveolar bone, periodontal ligament and root cementum. Periodontal diseases are mainly provoked by the action of dental plaque or microbial biofilm, which is a heterogeneous structure of pathogenic microorganisms. More than 500 species of microorganisms are considered potential etiological agents that provoke damage to periodontal tissues. In addition to them, viruses and fungi also play an important role in the pathogenetic process. As the disease occurs and progresses, pathogenic microorganisms colonize the gum area surrounding the tooth, and as a result of their impact on the tissue, a periodontal pocket begins to form. Up to 109 species of bacteria can be found in deep periodontal pockets, but despite the potential of many pathogens that are associated with periodontal disease, only a small number are associated with active disease.
Socransky et al divided pathogens involved in disease progression into two main groups: the “red” and “orange” complexes. The red complex includes the following Gram-negative anaerobic bacteria: Porphyromonas gingivalis, Treponema denticola and Tanneralla forsythia, while the orange complex consists of Prevotella nigrescens, Peptostreptococcus micros, Campylobacter rectus, Centruroides gracilis, Campylobacter showae, Eubacterium nodatum and Streptococcus constellatus. In addition, Aggregatibacter actinomycetemcomitans and Eikenella corrodens are closely associated with periodontal diseases. As a result of numerous studies, it has been established that in order to achieve a successful treatment result, one aspect of therapy must be aimed specifically at neutralizing these bacteria, the activity of which is directly related to the course of the disease.
Antibiotics
Systemic antibiotic therapy should be considered as an acceptable treatment option for patients with periodontitis. This approach is relevant for patients who are resistant to conventional disease therapy or who have the following health problems: the presence of an abscess, a compromised or weakened immune state, uncontrolled diabetes mellitus, the presence of signs and symptoms of systemic lesions, fever and lymphadenopathy. The choice of the most appropriate systemic antibiotic should be based on the results of culturing microorganisms and testing their sensitivity to a particular drug. Thus, it is possible to find out, firstly, what microorganisms are present in the affected area, and, secondly, to select the most effective and active agent. But it should be remembered that systemic antibiotic therapy should not be the only method of treatment, but only represent a segment of an integrated approach to examination, diagnosis and development of adequate systemic therapy. Antibiotic therapy, like any other treatment method, has its advantages and disadvantages. Since taking these drugs is a fairly well-known method of treatment, patients, as a rule, understand the main key points of this treatment, and without any problems agree to the proposed algorithm for the course of medications. But at the same time, patients can often confuse the official main names of medications, forget the dose, time, or even the very fact of taking them, thereby disrupting the effect of their action. Systemic antibiotics may cause side effects and gastrointestinal disturbances in the form of diarrhea or abdominal cramps. Other possible negative effects of drugs are associated with allergic reactions and the emergence of bacterial resistance to antibiotics during prolonged and uncontrolled use. Bacterial resistance is a major concern in medicine because it creates a number of other scientific and clinical dilemmas regarding the therapeutic trade-off between the risk of treatment and the potential benefit of antibiotics.
Systemic antibiotics reach periodontal tissues by extravasation from the blood serum, after which they pass through the junctional epithelium and lining of the gingival pocket to enter the gingival sulcus area. The effective concentration of the antibiotic when it reaches the gingival sulcus during a course of treatment differs from that in any other tissue system or organ with signs of infection, which is associated with the specific structure of the periodontium. There are a number of well-tested antibiotic regimens for the treatment of periodontal diseases, which are usually used in combination with mechanical removal of supra- and subgingival deposits and bacterial plaque. This approach, combined with effective home oral hygiene, is aimed at reducing the bacterial load in the area of the gum tissue above and below the marginal border. Some physicians commonly prescribe antibiotic regimens for the treatment and management of periodontal disease based on amoxicillin (375 mg) and metronidazole (500 mg) taken 3 times a day for 7 days in combination with oral scaling and complete root planing for the first time. 48 hours. This approach helps to achieve a reduction in pocket depth and reduce bleeding, which was found when comparing treatment results in the study and control groups. An alternative treatment regimen is to take azithromycin (500 mg) for 3 days prior to scaling and root planing to reduce red complex bacteria and reduce gingival scores. In the absence of the ability to culture bacteria and determine their sensitivity to antibiotics, you can use the empirical principle of prescribing drugs for the treatment of periodontitis. Evidence-based treatment options include a combination of amoxicillin and metronidazole (250 mg - 500 mg each) taken 3 times a day for 8 days, or a combination of metronidazole and ciprofloxacin (500 mg) for 8 days, 2 times a day.
Topical antibiotic therapy is an alternative adjuvant treatment option that can also be used during the treatment of periodontal lesions. The essence of the procedure is to deliver the antibiotic directly to the periodontal pocket - that is, directly to the site of colonization of pathogenic bacteria, while the concentration of the antibiotic in the affected area increases markedly compared to systemic administration. Another advantage is the absence of potential gastrointestinal disorders and allergic reactions. The first antibiotic used for topical treatment was Actisite (periodontal tetracycline). It consisted of non-resorbable, tetracycline-impregnated fibers that were placed directly into the periodontal pocket and remained there for 10 days until the next visit to the dentist. Over time, drugs and methods of their delivery to the area of periodontal lesions have been improved. Thus, Atridox (Denmat) was developed, which is the first resorbable topical antibiotic consisting of a gel form of doxycycline. This drug is injected into the pocket using a syringe, and upon contact with saliva, it hardens, acquiring a waxy consistency. Thus, the antibiotic can be released from the solidified phase within 21 days. Arestin (Orapharma) is also a topical absorbable antibacterial that consists of minocycline granules in powder form. It is supplied in the form of ampoules charged into a syringe. The powder is injected directly into the periodontal pocket, the high level of its therapeutic effect continues for 14 days, and the drug itself remains in the pocket for 28 days. Studies have proven that the use of topical antibiotics together with the procedure of complete removal of tartar and root surface cleaning allows to achieve clinically effective results: a decrease in the depth of the pockets and partial restoration of the damaged biological attachment are observed.
Antimicrobial mouth rinses
Antimicrobial rinses are well-known and acceptable procedures that effectively complement the comprehensive treatment of gum tissue inflammation. Examples of their justified use are situations where the patient is unable to provide optimal oral care using conventional hygiene products at home, for example, in the postoperative period. To choose the right mouth rinse that will effectively cope with gum inflammation and at the same time prevent plaque, you need to find out whether it has a Certificate of Approval from the American Dental Association. If yes, then this product has gone through a series of clinical, biological and laboratory tests that have proven its anti-inflammatory and antibacterial effectiveness. However, it should be understood that this assessment is advisory, but not prescriptive regarding the drug. The only rinses available on the market with the appropriate rating of the Association are representatives with phenolic components, such as Listerine and other similar versions. Chlorhexidine gluconate (0.12%) is also considered the gold standard among antimicrobial rinses, which is available only by prescription in the United States and is known under the commercial names Peridex and PerioGuard (Colgate-Palmolive). Chlorhexidine is the most effective antimicrobial rinse, reducing bacteria and providing effective treatment for gingivitis. The drug is more effective against gram-positive bacteria and yeast, and less effective against gram-negative pathogens. It is usually prescribed postoperatively to reduce the bacterial load during the healing period. Chlorhexidine has a high substance content, which ensures its prolonged action. Some side effects associated with the use of chlorhexidine include potential staining of the teeth and dorsum of the tongue; change in taste perception; the risk of possible formation of supragingival stone, the formation of signs of mucositis and desquamation of the epithelium. Other antimicrobial rinses available to the general public, but less often recommended by specialists, are quaternary ammonium derivatives such as Cepacol (Reckitt Benckiser). Sanguinarine-based products, like Viadent, are no longer widely available on the market. Oxygenate-based products, such as hydrogen peroxide, are recommended to be used more often in paste form. They have anti-inflammatory properties, which reduce signs of bleeding. The latter is an important critical indicator for assessing periodontal inflammation. However, these representatives have only a small effect on the level of bacterial contamination, and recently opinions have increasingly been expressed about their possible carcinogenic potential. Triclosan is another antimicrobial agent available in the form of toothpastes and rinses. However, according to research, it also shows minimal effects on the microbial flora of the oral cavity, and the safety of its use is still in question.
Anti-inflammatory agents
We must remember that periodontal diseases are infectious in nature, and inflammatory phenomena are the body's immune response to microbial contamination. In inflamed tissues, the process of proliferation of pathogenic bacteria occurs faster, which leads to the progression of pathological and destructive effects of the inflammatory process, through the activation of cells of the body's immune system (macrophages and their precursors, monocytes, lymphocytes, and polymorphonuclear leukocytes, such as neutrophils). Components of the microbial structure, such as lipopolysaccharide, which is found in the cell walls of gram-negative anaerobic microorganisms, activate macrophages to produce and secrete proinflammatory cytokines such as interleukin-1 (IL-1) and tumor necrosis factor-alpha (TNF-alpha). Interleukin-1 stimulates bone resorption and also promotes the release of PGE2 by fibroblast cells, which are the main and most abundant types of connective tissue cells. Fibroblasts synthesize collagen, the main structural protein of connective tissue, which is also the main component of gum and bone fibers. These cells and inflammatory response cells (neutrophils and macrophages) synthesize matrix metalloproteinases (MMPs), which are enzymes or proteins involved in a number of biological reactions. For example, MMP-1 and MMP-8 are enzymes that are involved in the degradation of collagen, which significantly weakens the periodontal structure. Activation of the immune system is inherently a protective reaction of the body - a response to bacterial invasion, however, during the mechanism of implementation of the immune response, tissues of the host organism itself are destroyed. This phenomenon is associated with the release of cytokines, pro-inflammatory mediators and MMPs, since these agents act not only locally on periodontal tissue, but when entering the bloodstream they can also cause undesirable systemic effects.
MMPs are a group of proteolytic enzymes found in periodontal tissues, which contain collagenase and gelatinase. The function of these enzymes is to remodel the extracellular matrix. Since doxycycline was found by researchers to have anticollagenlytic properties, they proposed its use as a modulatory agent for the treatment of periodontitis. Subantimicrobial doses of doxycycline (20 mg twice daily) are effective in inhibiting collagenase activity while having no effect on antimicrobial resistance when used in combination with complete scaling and root planing. This approach provides the maximum effect for restoring biological tissue attachment and reducing the depth of periodontal pockets.
Oral medications
Nonsteroidal anti-inflammatory drugs (NSAIDs) have also been studied as inhibitors of the host response in the treatment of periodontal disease. Their mechanism of action is to prevent the production of prostaglandins. Prostaglandin E2 (PGE2) is directly associated with the processes of inflammation and bone resorption, which is confirmed by its verification in affected periodontal areas. In the course of studying various NSAIDs (flurbiprofen, ibuprofen, ketorolac, naproxen, aspirin), which were administered systemically or locally, it was found that when they were combined with the procedure for complete removal of plaque and root surface cleaning, it was possible to maintain the existing height of the alveolar ridge, preventing it resorption. Bisphosphonates are a class of drugs that inhibit alveolar bone resorption that have also been used as host-modulating agents in the treatment of periodontal disease. Studies have shown that bisphosphonates, when used in conjunction with full mouth cleaning, reduce periodontal pocket depths and levels of bleeding during probing, as well as improve restoration of biological attachment and maintain ridge height. However, despite the potential benefits of bisphosphonates, studies have shown that long-term use and high doses of the drugs initiate osteonecrosis of the jaw. Obviously, for reasoned conclusions, it is necessary to conduct further more detailed studies that will help determine the ratio of the potential benefits of drugs and the relative risk of complications in the treatment of periodontitis.
Host modulation therapy
Local application of host-modulating agents, such as enamel matrix proteins, bone morphogenetic proteins and platelet-derived growth factors, can be quite effective in the complex treatment of periodontitis. Enamel matrix proteins are available in the form of Emdogain (Straumann) and have been successfully used in the restoration of periodontal defects. These proteins play the role of healing modulators, stimulating the regeneration of all periodontal components of the supporting apparatus of the tooth. Bone morphogenetic proteins promote the modulation and differentiation of mesenchymal cells into bone progenitor cells. They act as a scaffold onto which new bone tissue can grow and are often used in guided bone regeneration during alveolar ridge augmentation. Finally, platelet-derived growth factors enhance the chemotaxis of neutrophils and monocytes, stimulate the proliferation of fibroblasts and, accordingly, the synthesis of the extracellular matrix, and also increase the level of differentiation of mesenchymal progenitor cells, fibroblasts and endothelial cells. It is platelet-derived growth factors that are most often used during surgical interventions on periodontal tissues in order to accelerate their regeneration.
conclusions
New knowledge regarding host-bacterial interactions and host immune responses that provoke periodontal tissue damage will be useful for the development of newer and more effective concepts for the treatment of periodontitis using systemic and local antibiotics, antimicrobial rinses and principles of host-modulating therapy. The results of further studies may shed light on auxiliary adjuvant therapy, which can be used to correct treatment algorithms in order to achieve the most successful effect of complex therapy for lesions of the supporting apparatus of the tooth.
Posted by Alison Glascoe, DDS, MS
Metroxidine denta
- Description
- Quality control
Dosage form
Composition per 1 g
Active ingredients:
- Metronidazole benzoate – 16.0 mg
- Equivalent to metronidazole – 10.0 mg
- Chlorhexidine digluconate solution 20% – 2.5 mg
- Equivalent to chlorhexidine bigluconate – 0.5 mg
Excipients:
propylene glycol – 50.0 mg, carbomer-980 – 15.0 mg, disodium edetate – 0.5 mg, saccharin – 1.0 mg, levomenthol – 5.0 mg, sodium hydroxide – 4.0 g, purified water – up to 1 year