All tissues of the oral cavity, both teeth and gums, are interconnected and naturally have a complex structure. Gums, just like teeth, require careful and thorough care. Periodontology is a separate science in dentistry that deals with the study of gum disease. Inflammation from the teeth can spread to periodontal tissue, and vice versa. Therefore, it is so important to maintain careful hygiene of the entire oral cavity and promptly treat any dental diseases.
Gum structure
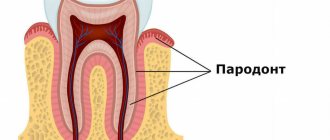
The periodontium consists of a complex of tissues that form the entire periodontal space.
- Periodontium is a complex of fibers that hold the dental unit in the socket. The periodontium is located between the cementum and the alveolar wall. Nerve fibers, lymphatic vessels, veins and arteries are also located here, which together are responsible for the proper metabolism of the tooth.
- The gums are the outer part of the entire complex. The gums are the first to bear the brunt of harmful microorganisms that enter the oral cavity.
- The alveolar process is a bone plate that has a spongy structure and serves as a bed for the dental unit.
- Cement is the outer covering and protection of the tooth root.
- Enamel covers the crown of the tooth and is the hardest element of the entire complex.
- The pulp is the main source of metabolism in the tooth. Consists of blood vessels and nerve endings.
- Dentin is a substance located around the pulp and consisting mainly of mineral components.
Anatomical and physiological features of periodontium
Basic concepts and provisions of the topic:
Periodontium is a complex of tissues that have genetic and functional similarities: dental tissue, periodontium (ligamentous apparatus of the tooth), alveolar bone and gums.
Dental cement is acellular and cellular (in the area of the apex and bifurcation); under pathological conditions it can undergo resorption. Cellular cement contains cells (cementocytes and cementoblasts) and calcified intercellular substance.
Periodontium is the ligamentous apparatus of the tooth. It consists of bundles of collagen fibers that combine bone and dental cement (Sharpey's fibers), and immature elastic fibers. They go in different directions and perform a supporting function. Between the bundles of fibers there are spaces filled with loose fibrous connective tissue containing blood vessels and nerve fibers; epithelial remains (islands) of Malasse, which are involved in the development of cysts, are also located here.
Periodontal cells are represented by:
— cementoblasts necessary for cement formation;
— osteoblasts located in the lacunae of bone tissue;
- fibroblasts oriented along the collagen
fibers;
- poorly differentiated progenitor cells.
On the surface of the tooth root and bone there are odontoclasts (cementoclasts) and osteoclasts that destroy these tissues; The interstitial periodontal tissue contains macrophages, mast cells, and leukocytes that perform protective functions.
The bony wall of the dental alveolus (the alveolar bone itself) is a thin plate of bone that surrounds the root of the tooth. It consists of lamellar bone tissue. Alveolar bone includes:
1 - compact bone that lines the tooth socket and covers the septa of the alveolar bone, which have a different structure: in the area of the front teeth - pointed; premolars – rounded, dome-shaped; molars - a type of truncated pyramid;
2 – spongy bone, which is formed by anastomosing trabeculae; between them there are bone marrow spaces filled with bone marrow.
The cortical plate of the alveoli has its own characteristics: elements of the periodontal ligament (Sharpey's fibers), Volkmann's canals are embedded into it, through which vessels and nerves penetrate into the periodontium. The presence of such structures during the development of acute inflammation in the periodontium can contribute to the spread of the process into the bone, and lymphatic capillaries and venules associated with the general blood flow can become the basis for the generalization of the process up to the development of sepsis and bacterial endocarditis.
The gingival mucosa is part of the oral mucosa that covers the alveolar processes of the jaws. There are three zones that differ in structure: attached, free gums and sulcular gums.
The attached gum is relatively inactive, since it does not have a submucosal layer and is tightly fused with the periosteum by connective tissue fibers.
The free part of the gum is not connected to the surface of the tooth and does not have a strong attachment to the periosteum by connective tissue fibers. Free and attached gums are formed by stratified squamous keratinizing epithelium and the lamina propria of the mucous membrane, consisting of loose connective tissue with a rich network of microvessels.
Periodontal functions
In a healthy state, the periodontium performs a number of functions assigned to it:
- Support. The main function is due to which the tooth is held between bone plates.
- Shock-absorbing function. Correctly distributes pressure over the entire dentition.
- Trophic. A function responsible for nutrition and ensuring metabolism of the tissue complex.
- A protective function that helps create a barrier against the effects of bacteria.
- Reflex – affects the correct distribution of the chewing load.
- The plastic function is responsible for the elasticity of periodontal tissues.
Publications in the media
Periodontitis is an inflammation of the entire complex of periodontal tissues, characterized by progressive destruction of the periodontium and alveolar bone tissue, and accompanied by the formation of pathological periodontal pockets.
Etiology. The most important local etiological factors include oral microflora (Porphyromonas gingivalis, Peptostreptococcus, Fusobacterium nucleatum, Veillonella parvula, etc.), dental plaque, anomalies in the position of teeth, bite, and others. Common disorders include diseases of the gastrointestinal tract, endocrine and nervous systems, metabolic disorders, and vitamin imbalance. Bad habits can contribute to periodontal damage. Pathogenesis. Periodontitis is always preceded by inflammation of the gingival margin (gingivitis). During the development of the pathological process, a violation of the epithelial attachment of the gum to the tooth occurs, destruction of the ligamentous apparatus, and resorption of the bone tissue of the alveolar process. A periodontal pocket is formed, which constantly deepens, reaching the root apex. Progressive resorption of alveolar bone leads to pathological tooth mobility. Destruction of the ligamentous apparatus of the tooth is accompanied by overload of individual teeth or groups, and traumatic occlusion occurs. With generalized periodontitis, gradual destruction of the entire complex of periodontal tissues occurs, which ultimately ends in tooth loss. Classification. According to the course, acute, chronic, aggravated periodontitis (including abscess formation), and remission are distinguished. Based on the severity of the process, they distinguish between mild, moderate, and severe periodontitis; according to its prevalence, localized and generalized.
Clinical manifestations. They are mainly determined by the severity and prevalence of the disease. • Localized periodontitis. It is characterized by aching pain, bleeding and severe swelling of the gums. Limited destructive inflammatory process in the area of one or several teeth (up to 5 teeth). Examination with a periodontal probe on all four sides of the affected teeth reveals a violation of the periodontal attachment and periodontal pockets of varying depths with purulent discharge or granulations. Tooth mobility of varying degrees appears. With exacerbations of the process, there is a sharp pain in the gums and alveolar part of the mucous membrane, painful percussion of the tooth, difficulty in eating and brushing teeth. If the outflow of purulent contents through the periodontal pocket is difficult, a periodontal abscess can form. • Generalized periodontitis. The initial stage is characterized by bleeding, swelling of the gums, pain in the gum area, bad breath and shallow periodontal pockets, mainly in the interdental spaces. In the developed stage of periodontitis, multiple pathological periodontal pockets of varying depths appear - with serous-purulent contents in chronic cases or abundant purulent contents in aggravated course of the disease. Based on the depth of these periodontal pockets, degrees of the disease are distinguished: I, II, III. Mobility of teeth develops, and subsequently traumatic occlusion is formed. Characterized by an abundance of soft dental plaque, supra- and subgingival dental plaque. Exposure of the necks and roots of the teeth may be accompanied by hyperesthesia. Sometimes retrograde pulpitis occurs. A chronic progressive course can lead to exacerbations accompanied by pain of a spontaneous nature. Abscesses and fistulas form one after another at intervals of several days. At the same time, changes in the general condition of the body occur—a rise in body temperature, weakness, and malaise. Enlargement and tenderness of regional lymph nodes are observed. The state of remission is characterized by dense gums of a pale pink color, possibly exposing the roots of the teeth. There is no dental plaque or discharge from pockets.
Diagnostics. In addition to clinical data, radiography (panoramic or orthopantomography) is of great importance. With localized periodontitis, destruction and foci of directed resorption along the tooth root are detected. In the initial stage of the generalized process, a compact plate is determined at the apexes of the interdental septa and an expansion of the periodontal fissure in the cervical region. The developed stage is characterized by resorption of interdental septa with a decrease in the height of the alveolar process and the formation of bone pockets; lesions of osteoporosis are detected. In the remission stage, the radiograph shows no signs of active destruction of the interdental septa; the bone tissue is dense. Differential diagnosis • Chronic gingivitis • Periodontal disease • Periostitis and osteomyelitis of the jaw.
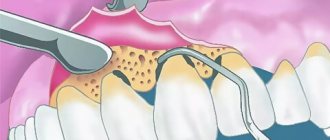
TREATMENT Local treatment • It must begin with careful removal of dental plaque, especially subgingival plaque using a scaler (Pieson-master-400). It includes the whole range of local effects: medication, orthopedic and physiotherapeutic. Eliminate local causes that led to the development of inflammation. For longer contact of drugs with periodontal tissues, gingival dressings or forms with a prolonged action are used. • Of particular importance are surgical methods (curettage, gingivitomy, flap operations, etc.) performed on the gums and bone tissue, which are aimed at removing granulations, eliminating periodontal pockets, restoring defects in the bone tissue of the alveolar process, etc. Surgical intervention is recommended to be combined with drugs , promoting the regeneration of periodontal tissue (keratoplasty). Teeth that have mobility are splinted. It is mandatory to remove teeth that have no functional value. To avoid overloading the existing/remaining teeth, direct prosthetics are recommended. • Physical therapy can be varied, including ultrasound and low-level laser radiation. Hydrotherapy in the form of irrigation of the oral cavity with water saturated with carbon dioxide has not only a therapeutic effect, but also improves oral hygiene.
General treatment is mainly carried out for exacerbations of chronic generalized periodontitis and in the presence of severe general somatic pathology (hereditary neutropenia, type 1 diabetes, etc.). It includes: broad-spectrum antibiotics, desensitizing and sedatives, immunotropic drugs (imudon, xymedon). Sometimes hormonal therapy and drugs that affect mineral metabolism (thyrocalcitonin) are prescribed. General treatment is combined with specific therapy for the general disease and vitamin therapy. Prevention • Timely treatment of gingivitis • Careful oral hygiene • It is advisable to use resort factors (balneotherapy and peloid therapy). The physico-chemical properties of mineral waters, therapeutic mud and climatotherapy have a healing effect on the oral cavity and the entire body.
ICD-10 • K05.2 Acute periodontitis • K05.3 Chronic periodontitis.
Periodontal diseases
Reasons why gum disease occurs:
- soft and hard plaque on teeth;
- anomalies in the location of dental units;
- poor-quality prosthetics or treatment;
- genetic predisposition;
- reduced immunity;
- diseases of internal organs;
- hormonal imbalances in the body;
- constant stress;
- various bad habits;
- Irregular oral care.
In contrast to the large number of causes influencing the development of periodontal diseases, there are not so many diseases themselves:
- Gingivitis is the initial stage of gum inflammation.
- Periodontitis is an inflammatory process in the gums, gradually spreading to the alveolar processes of the jaw.
- Periodontal disease is a fairly severe form of the disease, characterized by exposure of the roots of the teeth.
- Periodontoma is the formation of tumors in soft tissues.
General factors:
These are diseases of the body that contribute to the development of periodontal diseases. These primarily include:
- atherosclerotic vascular lesions (as a result of poor nutrition, increased cholesterol levels or hereditary predisposition);
- deficiency of vitamins C, B, A, E (poor nutrition, spring-autumn vitamin deficiencies);
- decreased body resistance to infections (most often respiratory);
- endocrine diseases (diabetes mellitus, parafunctions of the thyroid and parathyroid glands);
- diseases of the gastrointestinal tract (peptic ulcer, gastroesophageal reflux disease);
- blood diseases (anemia, pathology of the blood coagulation system).
Treatment
Treatment of major periodontal diseases is as follows:
- removing all plaque and then polishing the teeth;
- treatment of existing carious formations;
- carrying out high-quality prosthetics, if necessary;
- splinting of the dentition (also carried out if necessary);
- treatment of existing common diseases;
- taking vitamins or medications;
- Regular cleaning of the oral cavity not only at home, but also in the dental office.
In the most difficult situations, in addition to the listed treatment, surgical intervention may be necessary.
Etiology and pathogenesis (causes and development) of periodontal diseases
Calculus
The main point in the development of gum diseases such as gingivitis and periodontitis is dental plaque (plaque), which turns into tartar (calculus).
Photo 3. Soft plaque (plaque). Marginal periodontitis.
It is believed that organic soft dental plaque, which is formed from food debris due to poor hygiene, is gradually saturated with calcium from saliva and serum exudate of the gum pockets and is converted into hard tartar.
The latter can be of different hardness and color, which is determined by its composition. It consists of 18-25% organic matter (microbes and dead cells) and 75-82% inorganic matter (calcium, phosphorus, metal salts).
Tartar causes traumatic compression of the gums and prevents the cleaning of the periodontal pocket, promoting the development of microbial agents.
Microorganisms diffuse deep into periodontal tissues, lingering on the surface of the basement membrane and further into the bone tissue of the alveolar process.
Traumatic closure of teeth
In the absence of part of the teeth, in case of violation of the position of the teeth, in case of partial destruction of teeth and other traumatic factors, the remaining teeth are subjected to excessive and inadequate load. The latter, in turn, destroys the periodontium of the teeth.
Improper functioning of the temporomandibular joint (TMJ).
The ANS may be a significant factor in the development of gum disease.