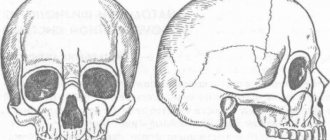
Exostosis of the jaw is a benign formation that manifests itself in the form of an osteochondral growth (osteophyte). The protrusions can be single or multiple and are located on the jaw bone. Maxillary osteophytes most often form on the outer (buccal) surface of the alveolar ridge, and exostosis on the lower jaw - from the inside, on the lingual side. A palatal bone growth (palatal torus) is also found.
Exostoses are painless and do not cause any discomfort at an early stage. But as it increases, the formation begins to cause a lot of discomfort - it complicates eating, affects sound pronunciation, interferes with prosthetics, etc. Treatment of osteophytes is only surgical. Removing exostosis on the gum is a low-traumatic operation that takes about an hour. The operation is performed under anesthesia, so the patient does not experience any discomfort. The method of surgical intervention depends on the location of the osteophyte.
Reasons for appearance
It is not precisely determined why osteophytes appear on the gums. But factors contributing to the disease include:
- Hereditary predisposition;
- frequent inflammation, purulent processes leading to atrophy, deformation of the jaw bone and nearby tissues;
- injuries of the dental system, especially accompanied by fractures of the facial part of the skull with improper reposition of bone fragments;
- complex tooth extraction;
- advanced periodontitis, periodontal disease;
- bite pathologies;
- congenital abnormalities of the jaw.
Often the pathology appears in childhood or adolescence. Also, the appearance of jaw growths may be associated with dysfunction of the endocrine system.
Exostosis in a child
It is in children that osteochondroma is most often first diagnosed, which is due to its formation from cells of the epiphyseal plate that is present only until the end of the growth period, which is adjacent to the metaphysis. It is also called the bone growth zone, since it is a hyaline cartilage whose cells are in constant miotic division. As a result, new chondrocytes (cartilaginous tissue cells) are formed, forming the epiphyseal plate, and the old ones are shifted to the metaphysis and subsequently replaced by osteoblasts (bone tissue cells).
In infants, violation of the rules for the prevention of rickets, in particular excessive use of vitamin D preparations, increases the likelihood of the formation of exostoses.
After puberty, the growth plates gradually close and are replaced by bone tissue, transforming into a thin epiphyseal line. If hormonal imbalances occur during this period, it is possible that the growth zones may remain open, which creates the preconditions for the formation of osteochondromas.
Usually, until the age of 7-8 years, bone exostosis does not manifest itself in any way in a child and makes itself felt only during the period of intensive growth, i.e., at 8-16 years, since it also begins to grow actively. In young children, such growths are present in the metaphysis area immediately near the epiphyseal plate, but subsequently move away from it and approach the diaphysis. Therefore, by how far the bone exostosis in children is from the epiphysis, the time of its formation is determined.
The growth of the neoplasm continues until the end of the growth period.
Symptoms
Exostosis of the tooth appears in the form of a convex growth that appears for no apparent reason. Main symptoms:
- Sensation of a foreign body in the mouth;
- discomfort when eating, talking (with large osteophytes);
- pain when pressing on the tumor;
- redness, thinning of the mucous membrane in the pathological area.
A small anomaly can only be detected during a dental examination, since visually it does not manifest itself in any way.
Types and stages of development
Exostosis can be present only on one bone, i.e., be solitary, or affect all metaphyses of the bones of the skeleton. In the second case, they talk about a generalized form of the disease, which is more common in men and is mainly hereditary. It is also called multiple exostotic chondrodysplasia. In this case, several bones or the vast majority of them are affected, but the formations have different shapes and sizes.
Depending on the shape and direction of growth, there are:
- hilly;
- linear;
- spherical exostoses.
Single exostoses have a narrow or wide base, while multiple ones are usually spherical or oval growths measuring 2-12 cm, sometimes more.
In its development, any osteochondroma goes through 3 successive stages:
- the formation of cartilaginous exostosis, which is not determined by palpation (palpation);
- ossification and active growth of growth;
- stopping the growth of the bone part of the neoplasm while maintaining the possibility of increasing the size of the cartilaginous cap.
Bone exostoses can already be felt during examination and can lead to discomfort, pain during physical activity and other symptoms.
Based on the nature of development and clinical picture, osteochondromas are divided into the following types:
- With normal growth rate. The osteochondral formation grows slowly, and there is a correspondence between the growth rate of the cartilage and the affected bone. Such osteochondromas have the most favorable prognosis, since after the end of the growth period they do not tend to continue to grow and almost never become malignant.
- With a high growth rate. An increase in the size of the growth occurs due to the proliferation of cartilage tissue and can also continue after the completion of the formation of the skeleton due to the preservation of the growth zone. In such cases, removal of exostosis is indicated, since there is a fairly high risk of malignancy.
- Malignant exostosis has the most unfavorable prognosis. Most often, osteochondral neoplasms of the ribs, pelvic bones, scapula and spine degenerate into chondrosarcoma or osteogenic sarcoma.
Why should jaw osteophytes be removed?
A bone growth on the gum is not dangerous until it begins to grow. Increasing in volume, the osteophyte puts pressure on the dentition and bone structures. This leads to tooth displacement, malocclusion, and jaw deformation. Large growths impede the movements of the tongue, complicate diction, and interfere with normal chewing of food. Large growths prevent prosthetics and implantation. Osteophyte of the jaw will not disappear on its own. The only effective method of treatment is surgical removal of the pathological formation.
Treatment and prevention of exostosis of the jaw
Surgical excision of the bone growth is the only effective treatment for exostosis. The intervention is performed under local anesthesia, so the patient does not experience discomfort. It is worth saying that there are two techniques for performing the operation. The choice of a specific technique depends on the location of the osteophyte:
- Removal of the palatine torus. In this case, the doctor makes a small linear incision, as well as two releasing incisions - in front and behind. After this, the dentist peels off the mucous membrane and removes the osteophyte. Extraction can be carried out either as a single block or in fragments. Next, the bone tissue is smoothed, and then interrupted sutures are applied.
- Removal of alveolar osteophytes. The procedure for performing the manipulations is no different from the previously discussed technique. The main difference is the configuration of the cut - in this case it has a trapezoidal shape. Otherwise, surgical treatment of maxillary and mandibular osteophytes is the same as removal of the palatine torus.
As for prevention, there are no specific measures to prevent this disease. The only thing that can be recommended is to visit the dentist regularly, at least twice a year, for examinations.
Still have questions? Sign up for a consultation at our clinic or call:
Indications
- Rapid growth of osteophyte;
- exostosis after wisdom tooth removal;
- discomfort, pain;
- the appearance of cosmetic defects on the lower or upper jaw (they look like white balls on the jaw, noticeable when smiling or talking);
- the need for implantation, removable or fixed prosthetics;
- the risk of tumor transformation from benign to malignant.
If you need to install prostheses or implants, exostoses will become an obstacle to the procedure. Dentures will injure the bone growth on the gum, and implants will not be able to take root normally in the bone due to the pressure of osteophytes.
How is exostosis removed?
If the exostosis does not grow, does not disturb the aesthetics of the dentition and does not cause any discomfort at all, then the doctor only monitors the situation at regular consultations.
Stages of the operation:
- administration of anesthesia,
- cutting and peeling of the gums,
- cutting down the exostosis with a bur, laser or piezoelectric device: when removing the formation, part of the periosteum that is adjacent to the growth is scraped off. This will prevent the re-formation of exostoses,
- returning the gum flap to its place and applying sutures.
The operation to remove bone growths is quite simple and takes no more than an hour and a half. After it is performed, the patient does not need to stay in the clinic for a long time.
Recommendations after surgery
At the Smile-at-Once clinic, surgery to remove bone growths is performed by professional surgeons. The procedure is not complicated, and the only thing that may occur is suture dehiscence or exacerbation of chronic diseases (for example, cardiovascular or nervous system, diabetes). Therefore, patients with health pathologies need to take prescribed medications, monitor blood pressure and blood sugar levels.
To protect the sutures, the patient must, in the first few hours after surgery, avoid eating hard foods, hot or excessively cold drinks, and not touch the surgical site with his tongue or fingers. It is also necessary to reduce physical activity for at least 1-2 days, refrain from drinking alcohol and smoking, since bad habits disrupt and significantly slow down tissue regeneration processes.
After the operation, the doctor also prescribes drug therapy, and, if necessary, rinses and baths for the oral cavity.
Progress of the operation
Before you begin the operation, you first need to carry out some kind of preparation. The patient must undergo blood tests to exclude the presence of contraindications. These include diabetes mellitus, HIV, and poor blood clotting. In order to confirm the diagnosis, an x-ray is required. The operation itself is performed as follows:
- Thorough treatment of the oral cavity with antiseptic drugs.
- Introduction of an anesthetic drug.
- Removal of exostosis. This can be done with a standard set of cutting tools or using a laser. The latter method is practiced only in prestigious clinics where the appropriate equipment is available.
- Finally, stitches are placed to stop the bleeding. After a couple of days they are removed; some dentists use absorbable surgical thread.
List of sources
- Zatsepin, S.T. Bone pathology of adults / S.T. Zatsepin. – M.: Medicine, 2001. – 640 p.
- Neustadt, E.L. Tumors and tumor-like bone diseases / E.L. Neustadt, A.B. Markochev. – St. Petersburg: Foliant, 2007. – 344 p.
- Epidemiology of skeletal tumors: educational manual / Chernyakova Yu.M., Ivanov S.A., Yadchenko V.N. – 2012.
- Volkov, M.V. Bone diseases in children / M.V. Volkov. – M: Medicine, 1985. – 511 p.
- Lanzman Yu.I. Benign tumors / Bone tumors. – Tomsk: Tomsk University Publishing House, 1990. – P. 88158.
Features of the postoperative period
In order for the wound to heal as quickly and easily as possible, it is important to follow the doctor’s recommendations during the rehabilitation period.
- Do not damage the seam
- Carry out hygiene procedures carefully (but under no circumstances abandon them)
- Take prescribed medications, including antibiotics, if the dentist considers it necessary to prescribe them
- Refuse hot or spicy foods, follow a semi-liquid diet, consume food and drinks only at room temperature.
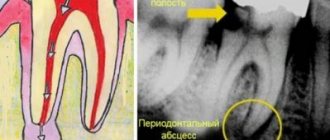
Tests and diagnostics
The diagnosis is made on the basis of the patient’s complaints, medical history, results of a physical examination and X-ray data in 2 projections, in which the tumor is visualized as an additional shadow with smooth, clear contours, connecting to the bone with a wide base or pedicle. If the cartilaginous cap does not contain calcifications, then it is not visible on the images. Additional methods of instrumental examination are:
- CT scan, which makes it possible to track the presence of a connection between the central part of the formation, which is filled with bone marrow contents directly with the medullary canal of the maternal bone.
- MRI - allows you to obtain data on the thickness of the cartilage cap, which allows you to determine the nature of the tumor (a thickness of more than 2 cm is a sign of malignant transformation).
- Differential diagnosis is carried out with other types of benign tumors ( chondroma , osteoma , osteoblastoma , chondroblastoma , osteoid osteoma ).