Drainage is a complex procedure
It is widely known that in the treatment of a patient, not only the choice of a medical institution and the timeliness of seeking help, but also the qualifications of the doctor treating him are of great importance. The knowledge, experience and skill of a specialist are embodied not only during the operation, but also directly during the patient’s rehabilitation period. In general, the postoperative period is a very difficult period of time, during which all human vital functions are restored. At this time, he is still under the supervision of a doctor who monitors the patient’s condition and carries out all necessary medical procedures to care for the patient. The main problem that can await a patient during this period of his rehabilitation is considered to be inflammation of postoperative sutures. This phenomenon can increase the patient's time in a medical facility, as well as interfere with the healing and recovery process. One of the techniques that prevents the onset of inflammation is the wound drainage method.
Postoperative wound drainage
This technique is aimed at preventing processes that cause irritation and inflammation of the skin. It is based on the use of special drainages, which promote wound healing after surgery and serve as an antibacterial means of protection against external damage and viruses. And this is an incredibly important point that occurs in most cases after complex surgical interventions. Drainage is installed if there is a risk of wound infection, if there is bleeding or discharge from other postoperative departments. Thanks to its use, the process of releasing blood clots or lymph outside the wound occurs. If the wound festers, but drainage allows you to remove clots of pus, which contribute to the proliferation of bacteria and microbes. In most cases, multilayer gauze dressings are used as drainage; latex or silicone dressings are also used, sometimes Teflon. The choice of drainage lies with the surgeon who performed the operation, depending on the degree of infection of the wound. All drainages are treated with special antiseptic substances (like the wound itself), which increases the chances of rapid healing of the suture.
How to make an appointment with a specialist? It's simple. You just need to call the number listed above and make an appointment with a doctor
Why cut the gum?
Pain in the gums continues for a long time - this is a natural accompaniment of tooth growth. Contact your doctor if you notice any of the following symptoms:
- Severe pain when chewing food or occurring spontaneously, without reason.
- If you have bad breath, this is a sign of pus under the hood.
- If the gums not only hurt, but also became red and swollen.
- The temperature has risen, severe weakness and headaches are felt.
Dentists will offer to cut the gum, be strong - this is not such a terrible procedure as it seems. After the incision, the rot will come out, the gums will heal, the pain will subside and the tooth will no longer cause concern. In different patients, the gums healed at different times: it usually takes from two days to two weeks.
Types of drainage
Drainage has its own types:
- Active - installed for the outflow of liquids through a special tube or hole from the bottom up;
- Passive - on the contrary, is installed according to the top-down principle.
The use of any of the presented types of drainage depends on the patient’s well-being, the degree of complexity of the operation performed, and the presence or absence of signs of inflammation. It is worth noting that failure to use wound drainage greatly contributes to the deterioration of suture healing time and can lead to the entry of microorganisms and infections into the wound, which are especially dangerous for patients in the postoperative period.
You can ask all questions on the topic by phone: +7-(928)-900-32-69
What to do if the drainage falls out of the gums
If the drainage randomly falls out of the gums, you should contact a specialist to determine the cause. This is often caused by improper installation of the system, weak fixation, intensive brushing of teeth and frequent rinsing.
In this case, you should pay attention to whether the swelling has subsided or not, whether there is suppuration.
The decision to return the system is made by the dentist; under no circumstances should you install drainage yourself.
Incorrect actions by the patient can lead to the development of complications and relapse of the infectious-inflammatory process. In this case, a rapid overgrowth of soft tissue occurs, blocking the exit to the outside for pus and excess fluid. As a result, the gums hurt, a lump forms, where purulent secretions accumulate abundantly.
If a child pulls out a drain, you should immediately contact a specialist for an examination of the oral cavity and further observation and treatment.
Drainage after cholecystectomy for acute cholecystitis
A large prospective randomized study in 1991 and a meta-analysis of 1920 patients (ACA) summarized 10 similar studies. It was shown that when comparing patients with and without drainage in terms of mortality, reoperation or drainage due to bile accumulation, there were no differences. Wound infection more often accompanied patients with drainage (5). Thus, on the eve of the end of the era of BCI, routine drainage - the sacred cow of biliary surgery - was abandoned in many centers.
What is the trend in emergency LCE? In a recent study of Australian surgeons, drainage was left routinely in 1/3 of cases (6). Another small randomized trial comparing patients with and without drainage for LCE examined the effect of drainage on postoperative pain and nausea, in terms of gas removal, and found no difference (7). If routine drainage is pointless in ACE, why is it indicated in LCE? Therefore, Petrowsky et al. (3) drainage is not recommended for both ACE and LCE. In a prospective study of 100 patients who underwent LCE for acute cholecystitis, all of them underwent cholescintigraphy one day after surgery. Bile leakage was detected in 8, but all of them were asymptomatic (8). Most postoperative collections, be it bile, serous fluid or blood, remain asymptomatic, the fluid is absorbed by the peritoneum and this is well known from ultrasound studies since the time of AChE.
Drainage is much more effective at removing bile than stool or pus. Therefore, it is logical to leave a drain if the surgeon is concerned about possible bile leakage. For example, if a subtotal cholecystectomy is necessary, or when there are difficulties with sealing the cystic duct, or there is a suspicion of additional bile ducts in the area of the gallbladder bed, which manifests itself in the form of bile leakage from the surface of the bed.
Thus, although most patients do not require drainage, if the surgeon is concerned about possible bile leakage or excessive serous fluid, drainage is appropriate. In most cases, almost nothing is separated through such drainage. It is extremely rare that preventive drainage becomes therapeutic in the case of profuse and persistent bile leakage. In cases where the need for an existing drain is questionable, it is extremely important to remove it as soon as possible. “Dry” drainage for 24 hours indicates that it has served its role. Finally, Howard Kelly (1858-1943) said: “Drainage is the recognition of defective surgery.” Clinicians must be careful not to confirm this statement in practice: if it is safer to switch to an open procedure and carefully close the ultrashort cystic duct than to rely on questionable clip closure and safety drainage, then the choice is clear.
Endoscopic method
Using an endoscope, doctors perform nasobiliary drainage of the biliary tract. Indications for endoscopic drainage of the biliary tract are:
- obstructive jaundice caused by malignant and benign neoplasms;
- acute purulent cholangitis;
- external biliary fistulas;
- damage to the walls of the extrahepatic ducts, retroduodenal perforations;
- acute cholecystitis.
There are no contraindications to endoscopic drainage, except in cases where the tube for drainage of the biliary tract cannot be passed through the area of tumor narrowing. The endoscopic kit for drainage of the biliary tract through the nose includes:
- conductor wire;
- drainages of various shapes;
- a connecting tube for collecting bile and flushing the drainage;
- nasal tube, clamp and spatula.
The operation of endoscopic drainage of the biliary tract includes the following steps:
- cholangiography to determine the level and location of drainage;
- introduction of drainage with a metal guide-conductor;
- removal of the guidewire and endoscope;
- control cholangiography;
- assessment of drainage position;
- transferring the drainage from the mouth to the nose and fixing it on the head.
After using the endoscopic method of drainage of the bile ducts, complications do not develop. They may occur due to the progression of the disease.
How to remove the drainage system, why can it fall out?
The stripe is small, sometimes it interferes with eating and creates a lot of inconvenience for its owner. Many people are interested in how long it will take to use the system, and whether it can be delivered ahead of schedule. During the application process, the dentist warns that if the drainage falls out of the gums, it will be safer to seek help from a specialist than to remove it yourself.
If an edge falls out, carefully adjust it and try to put it back in place. If you remove it yourself, you will need to wash your hands, disinfect your mouth, stand in front of a mirror, pull the edge of the strip with your fingers, and pull it completely out. Doing procedures at home is not so much difficult as it is dangerous. It’s better not to take risks and seek professional help. Gently rinsing the treated area will help speed up the tissue healing process. If the tape falls out in the first days of treatment, it must be promptly replaced to avoid possible infection with sad complications.
When is drainage placed in the gum?
Why is drainage in the gum needed:
- drainage prevents early tissue healing (before the wound is completely cleared of inflammation products);
- drainage on the tooth ensures removal of pus, blood and ichor from the injured area without creating discomfort for the patient;
- often drainage is also used as a channel for direct administration of medication into infected tissue.
If the drainage in the gum is installed correctly, then its design is practically imperceptible and invisible.
The need for such treatment can be caused by almost any disease of the oral cavity if it is accompanied by an infection.
Most often, severe suppuration (and, as a consequence, the need to install gum drainage) is provoked by:
- flux (inflammation of the periosteum);
- pericoronitis;
- alveolitis;
- periodontitis;
- cyst or abscess of a tooth.
Sometimes suppuration occurs against the background of trauma to soft and bone tissues, which is accompanied by complex tooth extraction or mechanical damage to the jaw.
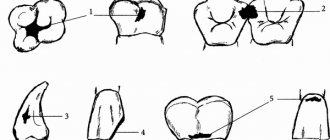
Photo. What does surgical drainage look like to remove pus?
Methods of drainage of the biliary tract
Oncologists prefer to perform external internal or, if technically feasible, external drainage of the bile ducts in patients with obstructive jaundice of tumor origin. Both methods are quite effective in preoperative preparation for radical surgery or as a final treatment method. Their advantage is:
- constant monitoring of bile flow;
- the possibility of active removal of blood, pus, and clots from the bile ducts;
- washing the ducts with aseptic solutions;
- dynamic x-ray monitoring of the location of the drainage tube.
Unlike external-internal drainage, bile completely flows out through the external drainage of the gallbladder. The disadvantage of external drainage of the bile ducts compared to external internal drainage is the complete flow of bile through the drainage to the outside. To compensate for the vital substances contained in bile, patients are forced to drink their own bile or medical personnel administer it through a nasogastric drainage. With external internal drainage, the distal end of the tube is located further than the narrowing site and most of the bile flows directly into the intestine. It remains possible to control the patency and flush the drainage and replace it with an internal transpapillary endoprosthesis.
Internal endoprosthetics of the bile ducts is performed after the elimination of jaundice. This is the final stage of treatment for inoperable patients. To successfully perform external or external internal cholangiostomy, oncologists use a set of special instruments: wire guides, special puncture needles, bougies and catheters.
Under local anesthesia using a Shiba needle, the surgeon tightly fills the bile ducts with a contrast agent. A long needle with a diameter of 1.5-1.7 mm performs a puncture of one of the segmental ducts. A conductor wire is then passed through it. The end of the conductor is passed beyond the narrowing, the narrowed area is widened with bougies, and a drainage tube is installed. It is fixed to the skin and the bile ducts are washed with sterile solutions.
This drainage method has disadvantages: there is a risk of bile and blood leaking into the abdominal cavity when the needle is removed, when passing a guidewire or bougienage the canal. Additionally, this complication may be encountered if the outer diameter of the needle is larger than the outer diameter of the guidewire. In order to reduce the number of complications associated with liver puncture, oncologists use the technique of installing a cholangiostomy using a stylet catheter.