05.08.2021 3924
Some patients ask whether pain may appear after cleaning the canal. The concerns are understandable - since the canal has been cleaned, there is no nerve in the tooth. Theoretically, he should not get sick and react to external stimuli. How are things going in practice? Let's look at this issue later in the article.
What is the canal cleaning procedure?
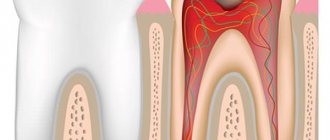
Before moving on to the issue of pain, let’s define what the root canal cleaning procedure itself is. Typically, such surgery is performed because the root is severely damaged. There are two reasons - inflammation or the development of infection.
Most often, root cleaning is performed in patients whom doctors have diagnosed with pulpitis or periodontitis. Cleaning and filling in such a situation are necessary in order to stop the destruction processes and save the tooth. The only alternative is deletion.
During the cleaning process, the soft tissues of the oral cavity are also affected. And here it is important to understand one of the central features of the procedure. Cleaning is done on already inflamed tissues. Since the inflammatory process usually affects large areas and spreads quickly, it will continue to occur for some time. Then the state will fade and stabilize. This usually takes several days.
Due to residual inflammation, the tooth may actually hurt for some time - this is normal. At the same time, the pain itself has a dull, aching character. It is not strong and most patients do not even have to take analgesics. Usually the discomfort intensifies slightly as the evening approaches.
If the patient’s body is in normal condition and nothing affects its regenerative abilities, after two or three unpleasant sensations begin to subside. The feeling of discomfort lasts longer, especially if the operation was traumatic or you have a complex root structure.
You will have to put up with pain much longer if, for some reason, you put off visiting the dentist until the last minute. In this case, the inflammation will become more and more severe, covering large spaces. Also, the rehabilitation process is extended if the patient has any systemic diseases of the body.
What materials are used to fill canals?
The main requirements for such filling materials are dense, hermetically sealed filling of the canals, chemical inertness (the material should not dissolve under the influence of body fluids), radiopacity (it should be clearly visible in the picture). Today, the following types of materials are used for filling dental canals:
- Solid fillers (fillers).
These include gutta-percha (a latex processing product), silver and titanium pins. Silver pins have recently been rarely used, since despite their good antibacterial properties they have a significant drawback - they do not provide complete tightness. - Polymer and natural pastes (sealers)
. A more preferable option is polymer sealers, which adhere better to the walls, do not stain dental tissue and do not dissolve when interacting with tissue fluids. - Glass ionomer cements.
Good adhesion and radiopacity, high biocompatibility and minimal shrinkage are the main positive qualities of such materials. They also have significant drawbacks: low strength, which is why such fillings are short-lived and not designed for serious functional loads. - Calcium hydroxide cements
. Non-toxic, biocompatible, radiopaque materials that exhibit minimal shrinkage, are easily removed if necessary and have bactericidal properties. However, they are considered not too strong and can break under heavy loads on the dental crown. - Polydimethylsiloxanes
. Modern reliable sealants with good therapeutic and operational parameters. Perhaps their only drawback is that this is a new product on the dental market and experience in using such materials has not yet been accumulated. There is no reliable information yet about the experience of patients after such treatment.
In case of inflammation of the tooth canals, the dentist selects the treatment individually, taking into account the type of dental unit, the number and shape of the roots, the patency of the root canals and the further plan for restoring the crown. Taking these factors into account, the filling material is also selected. Many specialists combine materials to achieve optimal characteristics and tightness of closing cavities. Filling techniques
Just 10-20 years ago, the main method of filling dental root canals was to fill them with one type of cement. This is a very simple and not labor-intensive method, but for the patient it has a lot of disadvantages: the channels are filled poorly and unevenly, voids appear in which microbial infection can develop. In addition, such cements quickly shrink and the canals soon have to be re-treated.
Modern dentistry offers completely different filling methods:
- Depophoresis
is the hardware introduction of medicinal and filling materials into the root canal. The technique allows you to effectively fill even curved and hard-to-reach canals. - Obturation with thermophiles
(plastic carriers coated with gutta-percha). A fast, fairly simple and reliable method, which still has the disadvantage of the possibility of material being removed beyond the root tip. - Filling with gutta-percha pin
. - Lateral condensation
is a dense filling of the canals with gutta-percha pins coated with a hardening sealer. A fairly reliable method, however, when using it there is a high risk of tooth root fracture. - Thermomechanical
(sometimes also called rotating condenser sealing) condensation. Recently, it has been used very rarely due to the high risk of complications. - Vertical condensation of heated gutta-percha
. A rather complex and lengthy, but at the same time reliable and durable filling method. - Injection filling with hot gutta-percha
. - Injection of heated gutta-percha
using the continuous wave method. One of the options for vertical condensation, characterized by greater simplicity and at the same time sufficient reliability and tightness of filling the channel. - Thermoplastic injection
of hot gutta-percha. A simple and fast method, which, however, does not always make it possible to densely fill the lateral tubules. - E&Q Plus
is a mixed technique using an injection gun to inject gutta-percha into the canal.
If you have a problem similar to that described in this article, be sure to contact our specialists. Don't diagnose yourself!
Why you should call us now:
- We will answer all your questions in 3 minutes
- Free consultation
- The average work experience of doctors is 12 years
- Convenient location of clinics
Single contact phone number: +7
Make an appointment
What to do if your tooth hurts after root canal cleaning
So when should you start worrying if your tooth hurts after root canal cleaning? The first reason to sound the alarm will be prolonged and severe pain. This gives reason to think that for some reason complications began to develop.
There are several key warning signs that should make you see a doctor:
- The pain does not go away for a long time.
- Instead of calming down, there is a constant increase in pain.
- Instead of a dull and aching pain, the pain becomes sharp, and a sensation of pulsation appears in the tooth.
- The gums become very swollen, and significant tissue swelling occurs.
- The temperature rises and the patient's general condition becomes worse.
In this case, timely consultation with a doctor becomes the key to maintaining your health. This also allows you to prevent the removal of a tooth for which the dentist cleaned the canals.
Toothache disappears immediately after the procedure
Wrong. After completing the treatment procedure, the patient will feel a significant improvement. However, it is normal for the tooth to remain sensitive for a few days after the procedure - in this case, taking painkillers may help. Minor pain may be present, especially when chewing, and may persist for several weeks. After this period, the pain should completely disappear.
Is it possible not to experience any pain after root canal treatment? Yes, this is possible, and it depends on how difficult the treatment process was and whether the tooth was infected before the dental intervention.
Reasons for the development of complications
The very cause of severe pain in the case of each patient must be considered separately. Among the most common sources of such pathology may be the following:
- Incorrectly chosen treatment method, gross mistakes made.
- The channel was not cleaned correctly.
- The doctor left foreign objects inside the canal, did not clean out the tooth fragment, and broke the instrument.
- The patient had a sudden allergic reaction to anesthesia or root canal filling agents, or various medications taken during treatment.
- The filling was placed poorly.
- Severe periodontitis developed and gum damage began.
- The canal walls were perforated during the cleaning process.
- The root of the tooth has received any damage.
Against the background of all of the above, the inflammatory process can actively develop. It becomes the cause of severe pain experienced by the patient.
Allergy
This complication of pulpitis treatment is easier to differentiate - an allergic reaction is often accompanied by tissue swelling. If it is a consequence of material moving outside the root canal, there may be swelling of the gums around the treated tooth. In some cases, it spreads to other areas - cheek, lip, depending on the specific tooth.
When pressure is applied, the pain becomes stronger, it is difficult to relieve with painkillers, and over time it only intensifies.
What to do if your tooth hurts after root canal cleaning
There can be many answers to the question of why a tooth hurts after root canal cleaning. For this reason, it is very important to pay attention to the characteristics of the individual patient’s body.
If you notice the first signs of the inflammatory process described in this material, you should consult a doctor as soon as possible.
The dentist carries out several basic actions:
- Collecting an anamnesis, taking into account the characteristics of the patient’s condition, the nature of the pain, medications taken, and personal characteristics of the body.
- X-ray of the affected tooth, examination of the condition of the gums, canals, assessment of the quality of the work performed.
- Opening the seal, re-cleaning, using disinfectants.
- Prescribing the patient a course of anti-inflammatory drugs and other medications.
Timely actions help to significantly reduce potential harm to the human body and ensure that the tooth can be saved.
One of the root canals was not processed
This is one of the rarest complications, since before starting endodontic treatment the doctor will definitely prescribe an x-ray diagnosis. It allows you to reliably determine the number of channels and evaluate their structure. But there are cases of abnormal location of root canals or their extremely small sizes, which makes them unnoticed in the image.
This leads to the following situation: the doctor removes the pulp in each canal, but one remains unattended - the inflamed pulp continues to hurt, and pathogenic bacteria continue to multiply. Such pain is difficult to confuse with other complications - the patient simply does not receive relief after treatment, and the pain characteristic of pulpitis itself remains. The sensations are pulsating in nature, the pain intensifies when eating, exposure to temperature on the tooth, and becomes unbearable at night.
The same symptoms can be observed with incomplete removal of the pulp in the diagnosed canal. In both cases, other symptoms may be observed:
- headache, sensations “radiate” to the ear, temple - depending on the specific tooth;
- increased body temperature;
- symptoms of general malaise.
Most complications are related to the complexity of the canal structure, and the following is no exception.
How to prevent pain and complications
Regardless of the field of medicine, doctors agree with a simple statement - it is much easier to prevent complications from developing at all than to treat them. There are a few simple recommendations that you should follow:
- Pay close attention to who is performing the operation on you. In our clinic, the task is performed by experienced surgeons who are well aware of all the features of the process. This ensures that mistakes are eliminated - the canal is filled correctly, and there are no fragments or dental instruments left inside.
- If you have previously had an allergy to any analgesics or anti-inflammatory drugs, tell your doctor.
- Don't put off visiting your doctor. The longer you leave a tooth untreated, the greater the risk of numerous potential complications.
- Ask how long the tooth hurts after root canal cleaning in your specific case. The doctor can make a prognosis based on information about the health status of a particular patient.
Also remember that if after cleaning the canals you have any signs of inflammation, you need to see a doctor as soon as possible. It is strictly forbidden to use self-medication, drugs without recommendation, or folk remedies. All this can only make the situation worse.
What not to do?
If, after treatment, a tooth hurts when pressed or without mechanical action, you should under no circumstances resort to folk remedies such as heating, hot compresses, heating pads - if there is an inflammatory process, this can greatly worsen the condition. In case of allergic reactions, heat will also increase swelling.
It is also not recommended to use folk remedies for rinsing, which can cause a burn to the mucous membrane - iodine, tinctures of alcohol or vodka, liquids with the juice of “scorching” plants, etc. Even if there is no gum damage, such measures can worsen the situation.
It is also not worth taking various painkillers uncontrollably - firstly, you need to see a doctor in any case, and the effect of analgesics will not allow you to fully evaluate the clinical picture. Secondly, it can be dangerous to health.
It is important to visit a doctor at the first opportunity and perform all the necessary procedures to eliminate unpleasant consequences and improve the condition.
Contact us for the right treatment
Our clinic employs dentists with extensive experience. They perform high-quality cleaning of dental canals and carefully ensure that the person does not experience any complications. We will also give all the necessary advice regarding the course of the recovery process, and recommend the necessary means to reduce pain and relieve inflammation.
We offer our customers competitive prices and special discounts. To get your first appointment and get professional advice, call the numbers listed on the website or leave a request.
Root canal treatment is expensive
Right. Although root canal treatment is expensive, it allows you to preserve the tooth, as well as its functionality and chewing functions. If you have a root canal and install a crown on the tooth, the cost of treatment will be less than if you remove the tooth and replace it with a bridge or dental implant.
The cost of treatment will depend on how many root canals the tooth has, whether it is the first time it has been treated, and on the qualifications of the dentist (general dentist or specialist).
After extraction
Extracting the root unit is a surgical procedure. It is associated with a violation of the integrity of oral tissues. It is not surprising that the human body reacts so sharply to the treatment.
Normally, after removal, the thermometer can show up to 38.5°C for no longer than three days. It is not advisable to take antipyretics - such tactics can change the course of recovery reactions. However, in some cases, doctors prescribe anti-inflammatory drugs to speed up regeneration processes. Some of them not only stop inflammation, but also normalize body temperature. If the doctor told you to use pills, you should do so. Any amateur activity is prohibited here.
In difficult clinical situations, antibiotics are prescribed after extraction. There are patients who are critical of such prescriptions. It seems to them that antibacterial drugs lower the immune system and their use after an ordinary removal of a unit is unjustified.
This attitude towards antibiotics is wrong. They help damaged tissues heal faster and eliminate the development of postoperative complications. Dentists never prescribe them just like that. Therefore, if a specialist issues a prescription after extraction, you need to take its prescription seriously.
Most often, an elevated temperature is recorded after removal:
- "eight";
- incisors, fangs, molars, if the operation was preceded by an advanced purulent process;
- several units at once.
Content:
- After caries closure
- After root canal treatment
- After extraction
- After implantation
- After sinus lift
The problems that dentists have to solve can be serious or not so serious.
But any medical intervention must be carried out in accordance with established norms and rules. Only then will the likelihood of complications develop to a minimum. One of the most common unpleasant symptoms after dental treatment is fever. Many patients are confused and do not know what to do when it increases. After all, it is not always clear whether a fever is related to a recent dental course.
Dentists insist that if the temperature rises after dental treatment, patients immediately consult a doctor. Timely receipt of qualified medical care is the most reasonable decision in such situations.
Insidious periodontitis: crept up unnoticed, left without a tooth
Periodontitis is the next stage of inflammation after pulpitis. The infection is localized at the apex of the tooth root and surrounding tissues. The disease is often asymptomatic, but without timely help it leads to tooth loss.
Causes:
- Untreated pulpitis. If a tooth hurts and then stops, it means that the inflammation has entered a chronic stage. Chronic pulpitis will slowly spread throughout the tooth and turn into periodontitis.
- Pulpitis treated using outdated methods. Before the advent of the apex locator, there was nothing to measure the length of the root canal, and the doctor acted blindly. If the canal is not completely treated and particles of infected pulp remain in it, complications arise. To avoid this, the doctor may have overdone it and brought the dental material beyond the root apex. Over the years, a focus of infection sometimes develops around a lump of paste.
- Tooth injury. A common problem in active children. Due to injury (the incisors are often affected), the pulp dies, and periodontitis develops after this. In fact, the reason is the same pulpitis that was not noticed and not treated in time.
Types of periodontitis
| Form | View | How it hurts |
| Spicy | Serous | Mild aching pain in the tooth area. |
| Purulent | Throbbing pain. Tooth mobility may increase. Possible swelling of the cheek, weakness, fever, flux. | |
| Chronic | Fibrous | No symptoms or slight darkening, dull color of the crown of the tooth. |
| Granulating | Mild pain when biting eventually turns into pain from heat, chewing, or pressure. The gums become red and swollen. | |
| Granulomatous | No symptoms. A fistula appears to drain the discharge, but the patient cannot always see it. |
The most aggressive is granulating periodontitis, which very quickly spreads to neighboring tissues. With this diagnosis, most often the tooth cannot be saved.
In the granulomatous type of the disease, the inflammation site has a hard shell, and inside it is filled with pus. Depending on the size, these neoplasms are called granuloma (up to 5 mm), cystogranuloma or radicular cyst (more than 1 cm).
Thus, granuloma and tooth root cyst are manifestations of chronic periodontitis.
Diagnostics
Do not confuse fistula with stomatitis. The fistula looks like a pimple, is located on the gum near the roots of the tooth, and does not hurt when pressed. If a fistula appears, contact your dentist as soon as possible.
The doctor can suspect a problem before the formation of a fistula or gumboil based on complaints. It is very important that the patient describes all the symptoms and does not hesitate to complain about mild, unexpressed, occasional pain and discomfort.
X-rays help to accurately establish the diagnosis. Periodontitis is visible even on a small targeted photograph. Next, to plan treatment, the dentist will suggest taking a panoramic image (all teeth in one frame) or a computer tomogram (a three-dimensional image of the dental system).
CT - 3D computer tomogram
allows you to see the type of periodontitis, the location and size of cystogranuloma, and give a prognosis for treatment.
Positive dynamics
visible on a repeat tomogram 2 years later
From all sides
The advantage of CT is the ability to examine the tooth and the tissue around it from different angles
Treatment
Depending on the stage and form of the disease, the doctor will select the optimal method.
1. Therapeutic treatment. Typically, three visits to the dental office are required.
- Urgent Care. The dentist will remove the source of inflammation: clean and disinfect the canals using medications and laser sterilization. If necessary, the doctor will install a drainage to drain the pus.
- Treatment of tooth canals and installation of a temporary filling. If there are doubts that the immune system will cope with the remaining microorganisms, the dentist may prescribe antibiotics, physiotherapy, rinses and medicinal baths.
- Tooth restoration. At the last visit, the dentist will take an x-ray to make sure that the inflammation has been removed. After this, you can begin filling and restoring the aesthetics and chewing function of the tooth.
- Observation. We can talk about the positive dynamics of the tissues surrounding the tooth after 1-2 years based on the results of an x-ray examination.
2. Tooth-preserving operations. Sometimes conservative methods are not enough. A dental surgeon can perform a cystectomy (removal of the cyst) or apex resection (cutting off part of the tooth along with the cyst).
3. Tooth extraction. In advanced stages, it will not be possible to completely defeat foci of infection. Attempts to save a tooth will lead to large financial expenses and jeopardize neighboring teeth. The best solution would be to install an implant in place of the affected tooth.
If a tooth is left without treatment, it will be removed prematurely. The inflammation will grow and go into an acute stage, and at the most unfortunate moment.
Doctors call chronic periodontitis a ticking time bomb. Exacerbation is provoked by stress, exertion, hypothermia or climate change. That is, it will happen on a long-awaited trip to the sea, while working on an important project, before an exam, or during an infectious disease.
Periodontitis in children
In a child, periodontal inflammation can develop on both milk and permanent teeth. Features of childhood periodontitis:
- high flow rate,
- severe symptoms (temperature, pain, swelling, possible suppuration),
- increased risk of complications. If urgent measures are not taken, the rudiments of permanent teeth will suffer.
Treatment follows the same scheme as for adults. If there is less than a year left before a baby tooth falls out or the roots have already resolved, the pediatric dentist will suggest removing the tooth.
Prevention
Simple and inexpensive measures will reduce the risks of periodontitis and tooth loss.
- Maintain good oral hygiene.
- Eat right. Excess carbohydrate foods provoke the development of pathogenic microorganisms.
- Contact a specialist for dental treatment in a timely manner. Come for a routine examination every six months, even if nothing hurts. Voice all complaints.
- Treat with understanding the doctor’s suggestion to undergo a panoramic radiography or computed tomography. Complete information will allow you to notice and cure the disease.
For expert assistance in writing the article and providing examples of work, we thank dentist-therapist Olga Yuryevna Yuryeva.
The effect of treatment is short-lived
Wrong. Although nothing can completely replace a healthy tooth, quality root canal treatment followed by a suitable filling or crown can be very successful. In approximately 85% of cases, the effect of treatment is lifelong.
If a tooth becomes affected again several years after root canal treatment, it often needs to be re-treated. However, in some situations, such as a crack in the tooth, very severe tooth root decay, or severe loss of bone around the tooth, the dentist has no choice but to remove the affected tooth.
Need to take painkillers
Right. Relatively, this is true. The pain experienced after root canal treatment is usually caused by inflammation around the tooth and may only last for a limited period of time. This process can be successfully managed with the help of common anti-inflammatory drugs: ibuprofen (Advil, Motrin), acetaminophen (Tylenol).
If severe pain continues for several months after the procedures, you should consult a dentist or endodontist to avoid possible complications.
After caries closure
Sooner or later, everyone faces the need to close carious cavities. With caries, the pathological process does not extend beyond the hard tissues. If your health condition worsens after filling, you can assume:
- development of a viral, infectious or bacterial infection not related to a recent medical intervention;
- the addition of complications such as pulpitis, abscess, phlegmon.
Determining the root cause of the problem is actually not difficult. If the sealed molar looks healthy and does not hurt, the gums are not swollen or swollen, and the mucous membranes are not ulcerated, it means that with a 90-95% probability the temperature has not increased due to treatment at the dental center. It’s just that at the time of therapy the patient was already sick, but the symptoms of the disease had not yet manifested themselves or were barely noticeable.
The stress experienced during the operation of the drilling machine can create conditions for the rapid spread of infection. Then, upon coming home, a person will see frightening numbers on the thermometer.
Mild but prolonged pain after treatment is normal
Wrong. It is not normal to experience constant pain for up to several months after root canal treatment. Causes of pain include hidden canals that were not cleaned during the procedure, or a crack in the tooth.
In these rare cases where pain persists, patients should be referred to an endodontist who specializes in root canal treatment for a diagnosis and appropriate treatment. In cases where the root or tooth is destroyed and no treatment method is suitable, the dentist has no choice but to remove the tooth.
Root canal treatment is a lengthy process that requires several visits to the doctor.
Wrong. Today, root canal treatment can take one to two hours if there are no complications. The number of visits to the dentist often depends on the condition of the tooth and the number of canals in it.
In cases where the damage is severe, your dentist or endodontist may place medication inside the canal to prepare (disinfect) the inside of the tooth and then finish treatment after a few days. But if there are no lesions or complications, all procedures can be performed in one visit.