Many parents have encountered the problem of a red throat in their child, which in most cases indicates inflammation. In this regard, it is very important to correctly determine the cause that caused the pathological process, since the effectiveness and success of treatment directly depends on this. And the first thing the otolaryngologist has to find out is: what is the nature of the disease - viral or bacterial?
We will tell Kaliningraders about all the nuances of the problem: the causes of throat hyperemia, possible diseases, and also how to distinguish a virus from a bacterial infection.
How can you tell if your baby has a sore throat?
First of all, it is necessary to examine the mucous membrane of the larynx. Hyperemia (redness) of the throat is an obvious, but not the only symptom. In addition, other clinical manifestations of inflammation may be present, such as:
- swelling of the tonsils and the presence of plaque on them;
- difficulty and pain when swallowing;
- redness of the visible parts of the throat;
- hoarse voice and sore throat;
- dry, barking cough;
- nasal discharge and nasal congestion;
- enlargement of the submandibular lymph nodes;
- loss of appetite and general weakness;
- headache and fever.
If some of the above symptoms occur, then parents should contact an otolaryngologist to find out the true cause of the inflammation. With adequate treatment, the prognosis is usually favorable.
General rules for treatment
Self-medication is strictly prohibited. If parents discover a red throat in a child, it is necessary to contact a specialist to clarify the diagnosis and prescribe a course of treatment. READ ALSO: A child has a red throat: how to treat inflammation at home?
Medication approach
Depending on the disease, the doctor prescribes medications to relieve inflammation. Medicines, especially antibiotics, cannot be selected independently - many of them have serious side effects. The following agents are used in therapy:
- For bacterial infections of the pharynx and sore throat, the antibiotics Augmentin and Amoxicillin are used.
- The drugs Umkalor, Tonsilgon and Lymphomyosot have antimicrobial and antiviral properties (for more details, see the article: Tonsilgon drops: instructions for use for children under one year old). They are available in the form of drops, which is convenient for treating small children. The remedies fight the disease, eliminate unpleasant symptoms and help improve immunity.
- For herpes and other types of viral infections, interferons, Tamiflu, Remantadine, Lavomax, Acyclovir are prescribed.
- If the disease is caused by fungi, the specialist prescribes Fluconazole or Levorin (we recommend reading: instructions for use of Fluconazole for children).
- For redness of the throat caused by an allergic reaction, antihistamines (Xyzal, Cetrin, Ebastine, Zyrtec) are prescribed. It is necessary to completely exclude the baby’s contact with the irritant.
- If a nonproductive cough is added to the redness of the throat, drugs to thin and remove mucus - Prospan, Ambroxol, etc. - are included in the treatment regimen.
- To reduce body temperature and relieve pain, Nurofen and Paracetamol are used.
Local treatment for a sore throat
To relieve the symptoms of the disease, topical agents are often used:
- Sprays Tantum Verde, Ingalipt, Bioparox, Chlorophyllipt act as antiseptics (we recommend reading: Tantum Verde spray: analogues of the drug for children). The drug sprayed onto the mucous membrane reduces pain and softens the throat. Active components fight pathogenic flora.
- Tantum Verde and Septolete lollipops have a “cooling” effect and reduce pain. Excellent help with dry cough and sore throat. By sucking the lozenges and swallowing saliva, the child removes the mucus accumulated in the throat.
- Miramistin solution, as well as the preparations Tanin (1-2%) and Antiformin are antiseptics used for gargling. Regular procedures gradually clear the mucous membrane of plaque. The active substances in the solutions destroy pathogens and relieve inflammation.
- Silver Nitrate solution 0.25% or Lugol's - for periodic lubrication of the tonsils (we recommend reading: how to use Lugol's as a spray for children?). Used to relieve inflammation and reduce pain.
- A solution of salt and soda with the addition of a few drops of iodine or chamomile decoction reduces discomfort and acts as an antiseptic.
- Compress made of rye flour, honey and vegetable oil. Mix the mixture until it has the consistency of dough, heat it in a water bath and apply it to the sore throat for 20 minutes. The product relieves swelling, inflammation and pain.
What makes your throat red?
In 80% of cases, the cause of redness of the throat is viruses and bacteria, less often fungal infections. However, it makes sense to voice non-inflammatory causes. These include:
- mechanical microtrauma of the mucous membrane;
- eating hot or coloring foods;
- contact with allergens or smoke;
- prolonged vocal load.
Without a doubt, chronic diseases of the nose and nasopharynx contribute to the spread of infection when inflammation spreads to the throat (the so-called “postnasal drip”). In such cases, it is important to promptly treat rhinitis and sinusitis, preventing the diseases from becoming chronic or protracted.
Anatomy of the pharynx
The pharynx is located behind the nasal and oral cavities; begins at the base of the skull and reaches the lower edge of the 6th cervical vertebra, where it narrows in a funnel-shaped manner and passes into the esophagus.
There are three sections of the pharynx:
- upper – nasopharynx
- middle – oropharynx
- lower – laryngopharynx
Nasopharynx
In the nasopharynx there is an accumulation of lymphoid tissue, which forms the pharyngeal tonsil - adenoids. Also in the nasopharynx are the tubal tonsils, which are located around the pharyngeal openings of the auditory tube.
This part of the pharynx is visualized only with the help of instruments or video endoscopic examination.
Oropharynx
The oropharynx is precisely that part of the pharynx that attracts attention when examined by an otolaryngologist and is accessible for examination by the patient himself.
It is located behind the oral cavity and is delimited by the pharynx. The pharynx is an opening formed above by the soft palate and uvula, on the sides by the anterior and posterior arches, and below by the root of the tongue. Between the anterior and posterior palatine arches there are another lymphoid accumulations - the palatine tonsils.
The palatine tonsils, arches, and uvula are subject to friction at the time of swallowing, due to which their mucous membrane may appear redder (hyperemic), in contrast to the entire oral cavity, gums, etc. But this is just a physiological factor.
The mucous membrane of the posterior pharyngeal wall contains elements of lymphoid tissue that visually resemble granules. The mucous membrane of the oropharynx has a dense network of vascular and lymphatic capillaries with rich sensory innervation, and therefore pathological processes are accompanied by symptoms - pain and discomfort in the throat, sensations of dryness, etc.1
hypopharynx
The laryngopharynx begins at the level of the upper edge of the epiglottis and passes into the initial part of the esophagus.
This part is also visualized only using instrumental and video endoscopic methods. This area is visually inaccessible to the patient.
Diseases of the oral mucosa are accompanied by various pathomorphological changes. Inflammation is one of the most common pathological processes of the mucous membrane of the mouth and pharynx and is a manifestation of the body’s protective reaction to the influence of a pathogenic factor. The course and outcome of the inflammatory process depends on the reactivity of the body, localization, activity and duration of action of the pathogenic factor.2
How to distinguish a viral infection from a bacterial one?
Let's start with the fact that bacterial infection is much less common than viral infection. In such cases, the disease is more complicated than a regular ARVI, and lasts from 5 to 14 days. Typical signs of bacterial attachment include:
- high body temperature;
- swollen lymph nodes;
- thick yellow-green sputum produced when coughing;
- the appearance of white plaque on the pharyngeal tonsils;
- clinical symptoms are expressed locally (ear, throat or nose).
The virus is characterized by:
- hyperemia of the throat is combined with sore throat and runny nose;
- expectorated sputum is clear and flowing;
- the appearance of a rash (with measles, rubella and scarlet fever);
- general weakness and aches throughout the body.
There are also significant differences regarding the treatment regimen. If the inflammation is bacterial in nature, antibiotics are indicated; only they can solve the problem. Accordingly, with viruses, antibacterial drugs will be useless; in such cases, it is necessary to take antiviral drugs. Therefore, it is very important to consult a doctor who will identify the true cause of the red throat and prescribe the right solution.
Symptoms to watch out for
The development of tonsillopharyngitis in a child is difficult to miss. Children are extremely sensitive to sore throats1,5,6. With its appearance, babies' sleep and appetite are disrupted, they become capricious and whiny1,6. Older children complain of a sore throat and sore throat when swallowing6,7. They develop a dry, superficial cough1,7.
A runny nose, red throat and fever in a child, especially in the autumn-winter period and early spring, most often indicate a cold, that is, ARVI1. The mucous membrane of the pharynx looks reddened, swollen, loose, dry or moist, covered with cloudy mucus1,2.
With an adenovirus infection, these symptoms include redness of the white membrane of the eyes, swelling of the eyelids, lacrimation, and “films” typical of adenoviral conjunctivitis appear in the eyes. 1.2. Lymph nodes enlarge. Sometimes nausea, vomiting and abdominal pain occur1. Upon examination, the pharyngeal mucosa appears slightly reddened, loose, with whitish deposits and lumps of thick mucus1,2.
The development of tonsillopharyngitis may be associated with enterovirus infection caused by Coxsackie viruses1,2. Enteroviral vesicular pharyngitis is called herpetic sore throat, since the rash resembles the blisters of herpes 2. Blisters filled with cloudy liquid appear on the reddened mucous membrane of the pharynx and oral cavity, and even on the plantar surface of the feet and palms. Possible muscle and abdominal pain1.
Fever, red throat and cough in a child may be manifestations of infectious mononucleosis associated with Epstein-Barr viruses1,2. In this case, in addition to redness and swelling of the mucous membrane of the pharynx, purulent “films” on the tonsils, all lymph nodes, liver and spleen are also enlarged1,2.
Tonsillopharyngitis caused by beta-hemolytic streptococcus is considered the most dangerous form of the disease2,3. This is due to the large number of complications that infection2 can lead to if it is not treated or treated incorrectly.
Streptococcal tonsillopharyngitis sometimes leads to the development of peritonsillar abscess, rheumatic fever, glomerulonephritis, and bacterial endocarditis2.
The following symptoms will help you suspect that redness in the throat is the result of the activity of streptococci:
- high temperature (> 380 C);
- absence of runny nose and cough;
- severe sore throat, forcing you to refuse food;
- severe swelling of the tonsils;
- the appearance of pinpoint hemorrhages (petechial rash) on the mucous membrane of the tonsils, soft palate and pharyngeal walls;
- purulent plaque on the tonsils, tightly connected to the underlying tissues;
- the appearance of ulcers and erosions on the tonsils in places where plaque is rejected;
- enlarged cervical lymph nodes2,3,7.
If a child has a red throat, but no temperature, this is a reason to think about non-infectious causes. Redness of the pharyngeal mucosa in a baby can be caused by prolonged crying, staying in a smoky room, eating too cold or hot food, or trauma to the pharynx with sharp objects. Sometimes the mucous membrane is colored red by dyes found in foods. The doctor takes all this into account when diagnosing tonsillopharyngitis1,2.3.
Diagnostic methods
Diagnostics consists of examining the patient, collecting anamnesis and a comprehensive examination, including:
- pharyngoscopy - visual examination of the pharynx;
- mirror laryngoscopy – examination of the larynx using a laryngeal mirror;
- endoscopic method - examination of the larynx using an endoscope;
- clinical blood test;
- bacteriological method (culture of mucus from the oropharynx will help determine the causative agent of the disease).
When examining a small patient, the doctor assesses:
- general view of the mouth, throat and larynx;
- color of mucous membranes and presence of swelling;
- size and color of tonsils;
- condition of the submandibular lymph nodes.
As soon as the causative agent of the disease is known (virus, bacteria, fungus or allergen), the doctor will prescribe appropriate treatment. If necessary, the otolaryngologist will refer the child to a specialized specialist.
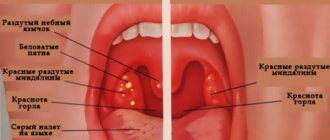
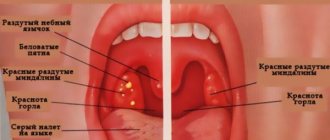
External signs of a sore throat
The condition of the oral cavity is influenced by the environment, past diseases, and inhaled microbes, so an absolutely healthy pharynx is rare. According to statistics, by the age of seven, almost every child suffers from various chronic throat diseases. You can determine whether the throat is affected or not by the following signs:
- The tonsils become red and increase in size, swollen follicles are clearly visible on them, which are sometimes filled with pus, and there is a white, yellowish or gray coating. With herpetic tissue damage, blisters and small ulcers form.
- The soft palate becomes inflamed and a rash may appear on it.
- The back wall of the pharynx looks swollen, loose, the follicles are enlarged. Upon examination, a pronounced network of small vessels can be detected. The presence of ulcers indicates infection with the herpes virus (see also: symptoms of herpes on the tonsils in a child). The tongue is hyperemic.
- The tongue is coated. If it has a brown or gray tint, affecting the tongue and teeth, this may indicate chronic pharyngitis.
Methods for treating throat diseases
Therapeutic measures, as in the treatment of any other diseases, involve solving two main problems:
- Elimination of intoxication and local syndromes.
- Prevention of the development of complications from other organs and systems.
As a rule, when treating red throat, drug treatment is used, taking into account the age of the child and the severity of the pathology. Depending on the etiology of the identified disease, the following drugs can be used:
- antiviral;
- antibacterial;
- antifungal;
- antiseptic;
- antihistamines;
- antipyretics and painkillers;
- immunomodulators and vitamins.
Treatment can be effectively complemented by physiotherapy: UV and UHF therapy, quartz, electrophoresis. Note that in 90% of cases, infectious diseases of the upper respiratory tract have a viral etiology, so antibiotic therapy is indicated only if a bacterial infection is detected. Only a doctor can determine it. We remind parents once again that it is categorically unacceptable to prescribe antibiotics on their own.
Otolaryngologist M.G. Goncharova
Red throat ” – with these complaints, parents often turn not only to an otolaryngologist, but also to a pediatrician. What is a red throat, and in what cases does it happen? In any case, a red throat implies inflammatory changes in the mucous membrane in the pharynx. What diseases does this happen with? The most common disease that causes hyperemia of the pharyngeal mucosa is acute catarrhal pharyngitis. At the same time, we see hyperemia of the mucous membrane of the posterior wall of the pharynx, the side walls of the pharynx, and the soft palate. This condition occurs very often with respiratory viral infections, influenza, and childhood infections such as chicken pox, measles, and rubella. Redness of the back wall of the pharynx can also be caused by exacerbations of diseases of the gastrointestinal tract, such as biliary dyskinesia, chronic gastroduodenitis.
Sore throat in children
But such a simple disease as acute pharyngitis should not be confused with a more serious disease such as tonsillitis, because sore throat is usually called sore throat. Unlike acute pharyngitis, with angina, in addition to hyperemia of the posterior pharyngeal wall, we note hyperemia, filtration, edema of the anterior and posterior palatine arches. The palatine tonsils, which are located on the lateral surfaces of the pharynx, in this case increase in size, swell, and turn red.
At different stages of tonsillitis, either a whitish coating may appear on the surface of the tonsils, or purulent compartments may appear in the lacunae. Sore throat, unlike acute pharyngitis, is a serious infectious disease that most often occurs with fever and symptoms of intoxication.
What other diseases cause the “red throat” symptom?
In addition, a red throat can occur with various inflammatory diseases of the oral mucosa, such as stomatitis, or during teething in children. In this case, as with acute pharyngitis, the anterior and posterior palatine arches are not involved in the process and the tonsils are not involved.
The throat may be red even in the absence of any acute changes in the pharynx. Redness of the palatine arches or the so-called “congestive hyperemia of the palatine arches” may be a sign of a chronic inflammatory process or a sign of chronic tonsillitis. In this case, we see congestive hyperemia of the anterior and posterior palatine arches, hypertrophy of the lateral ridges of the pharynx without any acute disease. Depending on the symptoms, this condition may not require treatment at the time of examination.
What symptoms are noticeable to parents when their child’s throat is red?
Now let's talk about how the child behaves, and what parents can observe if the throat is red. If parents look into the child’s throat and see that the back wall of the pharynx is hyperemic, in this case it is very important to take into account the general condition of the child.
If the child’s condition is good, there are no symptoms of intoxication, there is no increase in temperature, he does not actively complain of a sore throat, then this non-serious condition can be regarded either as symptoms of acute pharyngitis, which require symptomatic therapy, or require treatment of an underlying disease, such as respiratory viral infection or any of the childhood infections.
In the case when a child actively complains of a sore throat, while he has an increase in temperature, symptoms of general intoxication, this condition must be differentiated from a sore throat, and in this case the child must consult a doctor and carry out active treatment, including (if necessary) general antibacterial therapy.
Treatment issues. What to give and when to give for a red throat.
As for the treatment and approach of parents to the problem of a red throat, it is very important to pay attention to the following points: a red throat is a symptom, I repeat, of a number of diseases, and in some cases, treating only the red throat itself will not lead to the desired result.
Therefore, active independent local therapy using antiseptics, local antibacterial drugs, sometimes even saline solutions, can lead to the development of pharyngeal dysbiosis.
Dysbiosis of the pharynx is a disruption of the normal microflora in the oral cavity, which, in turn, leads to a decrease in the protective functions of the mucous membrane itself in the oral cavity, and in this case it itself becomes an entry point for infection.
On the other hand, during self-medication, the adaptation of pathological microorganisms to antiseptics or local antibacterial drugs quickly develops, which in the future can significantly complicate the treatment of acute inflammatory diseases in the pharynx when necessary.
Therefore, before using any drug to rinse or irrigate the pharynx, you need to very clearly define the purpose of this treatment, because such a concept as “treating just a red throat” is unacceptable.
In some cases, a red throat may not be treated and does not require any special treatment, and the problem will be solved only by treating the underlying disease that led to the symptom of a red throat.
What inconveniences does the problem of red throat cause for parents?
Why is this problem inconvenient for parents? First of all, parents are worried about the fact that the child has a red throat.
Remember, it is very important to always take into account, in addition to the fact that we see a red throat, also general clinical symptoms: are there any other symptoms of disease, how disturbed is the child’s general condition, is there an increase in temperature? And only in this case it is necessary to somehow deal with this problem.
On the other hand, a red throat may be a symptom of some chronic disease in the pharynx, the most common of which are chronic tonsillitis or chronic pharyngitis, which can exist as independent diseases or, in the case of chronic pharyngitis, as a symptom of some disease in the underlying parts of either the gastrointestinal tract or lower respiratory tract. Therefore, if you often observe a red throat in your child, then in this case you need to consult a pediatrician, or better yet, an otolaryngologist, because it is with him that you can clearly determine what this pathology is associated with. An otolaryngologist will be able to teach you to differentiate a mild disease such as acute pharyngitis, which is a symptom of a respiratory infection, from a more severe condition, and also to rule out a chronic disease in the tonsils of the back of the pharynx.
A visit to an otolaryngologist is the ideal solution
I repeat once again, what would be the most logical solution if you often observe a red throat in your child? This problem should be discussed with an otolaryngologist, who will analyze the diseases that the child suffered from, analyze the objective picture, and, if necessary, can examine the microflora in the oral cavity, on the back wall of the pharynx, in the lagoons of the tonsils. And only then will it be possible to come to some correct conclusion, on the basis of which treatment will be selected or the dynamics of observations will be selected, i.e. a certain concept will be formulated according to which this child will be observed or treated.
Is the red throat effect related to respiratory function?
How can a red throat and respiratory dysfunction be connected? In general, these are two rather related problems, if only because when a child’s breathing function is impaired, the child switches to mouth breathing. Breathing through the mouth is not physiological: the child breathes through the mouth, while the inhaled air is insufficiently warmed and moistened, and in any case this will lead to certain changes, and then inflammatory changes in the mucous membrane, primarily the back wall of the pharynx. This will manifest itself in the form of hyperemia or redness of the mucous membrane of the back wall of the pharynx.
If we talk about how quickly this problem can be dealt with, then it is impossible to answer this question unequivocally; a lot here depends on the reason why the red throat appeared. Therefore, it is quite difficult to give any recommendations here; it all depends on the condition that led to the redness of the throat.
Recovery criteria
The following signs indicate successful treatment and speedy recovery:
- normalization of temperature;
- absence of signs of intoxication and asthenic syndrome;
- redness and swelling of the oropharynx disappeared;
- the size of the lymph nodes decreased.
Note that it is equally important during the treatment process to strictly follow medical recommendations, which consist of following bed rest, a gentle diet and drinking plenty of fluids.
We remind Kaliningrad residents that you can make an appointment with a pediatric otolaryngologist by filling out a preliminary application on our website or by calling: +7 (4012) 357-773 or +7 (4012) 973-100.