Mechanism of disease development
Acute laryngitis is an inflammation of the mucous membrane of the larynx. The larynx is located in the front region of the neck. It connects the pharynx to the trachea and performs three vital functions:
- sound-producing (the vocal apparatus is located in it);
- respiratory;
- protective (prevents food and foreign particles from entering the trachea).
Under the influence of a number of factors (hypothermia, overstrain of the vocal cords, allergies, infectious diseases, etc.), the mucous membrane of the child’s larynx becomes inflamed. As a result, a sharp dilation of blood vessels occurs, edema develops, the lumen of the glottis narrows (or completely closes), speech function is impaired and breathing becomes difficult.
Nasal cavity and paranasal sinuses
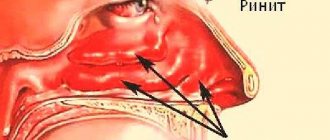
The size of the nasal cavity in newborns and infants is relatively small. The nasal cavity is shorter, narrower and located lower, compared to other age groups, due to underdevelopment of the facial skeleton. The vertical size of the nasal cavity is significantly reduced due to the absence of a perpendicular plate of the ethmoid bone, which is formed only by 6 years of age. The lower wall of the nasal cavity is in close contact with the tooth germs in the body of the upper jaw, which is associated with the risk of developing osteomyelitis of the upper jaw due to inflammation of the nasal cavity and ethmoid sinuses. Acceleration of growth occurs already in the first half of life and is associated with intensive development of the skull, mainly the maxillary region, and teething.
Along with the small size of the nasal cavity, a sharp narrowing of the nasal passages, closed by well-developed nasal conchas, is important. The inferior turbinates are located low and fit tightly to the bottom of the nasal cavity, as a result of which the lower nasal passages are impassable for air. The upper and middle nasal passages are practically not expressed; children are forced to breathe through a narrow common nasal passage. In this age group, severe difficulty in nasal breathing often occurs, especially when mucous secretions or crusts accumulate in the nasal cavity.
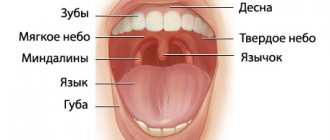
As a result of the discrepancy between the significant volume of the nasal concha and the narrow respiratory area, acute rhinitis in newborns and infants is severe, with a predominance of general symptoms and the frequent development of complications. Even a slight swelling of the mucous membrane of the narrow and small nasal cavity leads to the cessation of nasal breathing. The child’s breathing takes on a “volatile” character: children breathe frequently and shallowly, but the wings of the nose do not swell, as with pneumonia. Sucking is severely difficult or impossible, sleep is disturbed; the child is restless, body weight decreases, and dyspepsia and hyperthermia may develop. Breathing through the mouth leads to aerophagia with flatulence, which further complicates breathing and leads to disruption of the general condition of the child. When the nose is stuffy, the child tilts his head back to make it easier to breathe, and convulsions are possible. Due to the pronounced tendency to generalize any inflammatory processes in newborns and infants, acute rhinitis occurs as acute nasopharyngitis. At the same time, on the soft palate you can see reddened tubercles protruding anteriorly - clogged mucous glands.
This age group is characterized by the so-called posterior runny nose, caused by the accumulation of infected mucus in the posterior parts of the nose, associated with difficulty in draining secretions into the nasopharynx due to the structural features of the choanae. On the back wall of the pharynx, stripes of viscous sputum descending from the nose are visible, hyperemia of lymphoid granules in the back wall of the pharynx; Enlarged occipital and cervical lymph nodes can be identified.
The mucous membrane of the nasal cavity in young children is very delicate and well vascularized. The folding of the mucous membrane of the nasal septum observed in newborns soon disappears. The ciliated epithelium directly passes into the stratified epithelium of the nasal vestibule. An important feature of the nasal cavity in newborns and children in the first half of life is the absence of cavernous (cavernous) tissue in the area of the free edge of the lower and middle turbinate. In this regard, children of this age practically do not experience spontaneous nosebleeds, unlike older children. If bloody discharge from the nose appears, it is necessary to conduct a thorough examination to exclude congenital hemangioma or a foreign body in the nasal cavity. For the same reason, in newborns and children in the first six months of life, it is not advisable to use vasoconstrictor nasal drops, the action of which is designed to reflexively contract the cavernous tissue of the nasal turbinates. The rarity of spontaneous nosebleeds is also explained by the underdevelopment and deep location of the branches of the nasopalatine artery and its anastomoses in the anteroinferior part of the nasal septum (Kiesselbach's bleeding zone).
The paranasal sinuses in newborns are underdeveloped and are formed during the development of the facial skeleton and the growth of the child. At birth, there are two paranasal sinuses: a well-developed ethmoid sinus (anterior and middle cells of the ethmoid labyrinth) and a rudimentary maxillary sinus in the form of a narrow slit (mucosal diverticulum) at the inner corner of the orbit in the thickness of the bone of the upper jaw. The frontal, sphenoid sinuses and posterior cells of the ethmoid bone are in their infancy. In this regard, among diseases of the paranasal sinuses in newborns and infants, damage to the ethmoidal labyrinth (ethmoiditis) predominates, which is especially severe with orbital and septic complications.
Causes of acute laryngitis in children
In order for assistance to a child with acute laryngitis to be as effective as possible, you must first find out what caused the development of the disease. The main provoking factors include:
- ARVI, influenza;
- bacterial respiratory tract infections caused by pneumococcus, staphylococcus, streptococcus, hemophilus influenzae;
- complications after scarlet fever, measles;
- inflammation of the paranasal sinuses;
- local/general hypothermia of the body;
- inhalation of cold, smoky air;
- congenital weakened resistance of the respiratory tract;
- unfavorable environmental conditions;
- contact with allergens;
- uncontrolled use of sprays and aerosols for the throat, leading to a reflex spasm of the larynx in a child;
- overstrain of the vocal cords (strong screaming, loud singing);
- infectious diseases of the oral cavity;
- stress factors.
Symptoms of acute laryngitis
In childhood, acute laryngitis develops quite rapidly. At an early stage of the disease caused by a virus, the child experiences:
- general weakness,
- nasal congestion,
- soreness,
- redness of the throat,
- painful swallowing.
In some cases, body temperature may rise to 38–39°C.
Further added to the above symptoms are:
- rhinorrhea (excessive mucus discharge from the nasal passages);
- dry barking cough;
- hoarseness or complete loss of voice.
Over time, during intensive complex treatment of laryngitis, the cough becomes more rare and productive, that is, accompanied by the discharge of sputum.
Prevalence
The incidence of epiglottitis decreased sharply after the introduction of the Hib vaccine into the routine childhood immunization program. Before the vaccine was available, the incidence was approximately 5 per 100,000 children under 5 years of age. Among immunized children, the incidence of epiglottitis ranges from 0.6 to 0.8 cases per 100,000. The average age of children with epiglottitis has increased from 3 to 6–12 years.
The incidence of epiglottitis in adults has been largely stable over the past few decades, ranging from 0.6 to 1.9 cases per 100,000 people annually.
Complications of acute laryngitis in children
One of the most dangerous complications of acute infectious laryngitis, characteristic of early and preschool childhood, is stenosis (narrowing of the lumen) of the larynx. It is also called false croup or acute airway obstruction. This complication may be due to the structural features of the child’s respiratory tract. Most often it develops against the background of influenza, parainfluenza, adenovirus, measles infection or chickenpox.
When the space under the vocal cords swells, the lumen of the larynx narrows, acute obstruction of the airways occurs, and oxygen deficiency develops. Symptoms of laryngeal stenosis are:
- heavy wheezing,
- barking cough
- hoarseness or complete loss of voice,
- excessive excitement of the child,
- enlarged lymph nodes,
- increase in body temperature,
- the appearance of light dry wheezing.
If you notice these symptoms, you should immediately consult a doctor. But it’s better not to let this happen and start treating acute laryngitis on time.
How to make an appointment with a doctor
To receive highly qualified medical care, you must make an appointment with a pediatrician who will conduct an examination and comprehensive medical examination of the child. If necessary, the pediatrician will consult with or refer other specialists.
To make an appointment with a specialist in the pediatric department of JSC "Medicine" (clinic of academician Roitberg), use one of the following methods:
- a quick entry form on the main page of the center’s website;
- by telephone 24/7;
- using a mobile application.
The clinic of JSC "Medicine" (clinic of academician Roitberg) is located in the center of Moscow at 2nd Tverskoy-Yamskaya lane, 10, a five-minute walk from the Mayakovskaya metro station, as well as not far from the Belorusskaya, Tverskaya, Chekhovskaya and Novoslobodskaya metro stations .
Diagnosis of the disease
Diagnosis of acute laryngitis is not particularly difficult. The diagnosis is based on the presence of acute respiratory infections symptoms, as well as hoarseness, shortness of breath, and barking cough. Call a doctor: he will listen to complaints, examine the child, measure the temperature, listen to the lungs and make a diagnosis.
Non-drug therapy
Treatment of acute laryngitis depends on the age of the child. This may include:
- compliance with bed rest;
- limiting vocal load (for 5–7 days it is better for the baby to remain silent or talk as little as possible);
- maintaining the optimal temperature (+18…+20°C) and air humidity (50–70%) in the room where the sick child is located;
- drink plenty of fortified drinks (the liquid should be warm and unsweetened);
- following a hypoallergenic diet - if there are symptoms of laryngitis, it is strictly not recommended for a child to give sour, spicy, too hot or cold foods and carbonated drinks.
When treating inflammation of the mucous membrane of the larynx, children are allowed to apply wet and dry warming compresses to the neck area and gargle with a warm infusion/decoction of chamomile or sage, if recommended by a doctor.
Treatment of epiglottitis
If epiglottitis is suspected, the patient requires emergency medical care.
The main goal of managing patients with epiglottitis is to establish a definitive diagnosis and immediate treatment (before the onset of airway obstruction).
In standard cases, empirical antibacterial therapy is prescribed taking into account the most common pathogens, priority is given to third-generation cephalosporins. In cases of severe disease, the presence of sepsis, meningitis, and a high probability of MRSA epiglottitis, the antibiotic Vancomycin is prescribed. For patients with immunodeficiencies (including HIV infection), antibiotics are selected taking into account the most common pathogens in this group of patients, as well as based on the results of bacteriological testing, if possible.
The optimal duration of antibiotic therapy for epiglottitis is unknown. Most clinicians provide treatment for 7–10 days, depending on the patient's condition.
Drug therapy
How to fight infection?
Drug therapy for laryngitis that appears in a child against the background of an acute respiratory infection includes the use of antiviral and immunomodulatory drugs.
Antihistamines, which are usually prescribed for allergies, help relieve swelling of the mucous membrane and calm the baby. They should be given before bedtime, strictly according to the recommendation of the attending physician. What to do if you have a cough?
Remedies for this symptom are another essential component of treatment.
In the early stages of laryngitis, if a child has a dry hacking cough, drugs that block the cough center are used. Next, at the first signs of coughing, mucolytics are prescribed to thin the mucus and improve expectoration of sputum. Doctor MOM® cough syrup has similar properties. This complex herbal medicine, containing extracts of 10 medicinal plants, helps not only to liquefy mucus, but also to relieve swelling and inflammation. Herbal syrup is approved for long-term use in the treatment of laryngitis in children over 3 years of age. Actions at temperature.
If a child has a hard time tolerating a high temperature, he is prescribed an antipyretic. Treatment of laryngitis with antibiotics is justified only in the presence of serious bacterial complications and only as prescribed by a doctor.
How to relieve swelling of a child’s throat before the doctor arrives?
Sore throat medications for children should not be given to children before consulting a doctor. But the mother can alleviate the baby’s condition at home.
- The most important thing is calm. When a child is nervous, breathing quickens and shortness of breath intensifies. You need to talk to your baby in a quiet and confident voice, without showing your fears.
- Humidifying the air will help relieve spasms and make breathing easier. Containers of water placed around the room or a damp cloth on the heating radiators help a lot. You can take your sick baby to the bathroom and sit him next to a bathtub filled with hot water.
- If the throat is swollen, you should not allow the child to lie down, much less fall asleep. In a horizontal position, blood flow to the larynx increases, which provokes further development of edema. The best position is half sitting, in mom or dad's arms.
- Fresh cool air makes breathing easier when the throat is swollen. The child can be wrapped in a blanket and taken out to the balcony or at least open the window in the room.
- It is worth giving more fluids to drink. Warm alkaline drink, for example, heated milk with mineral water or soda, thins mucus, helps relieve inflammation and reduce swelling.