Cleaning the tooth canals is a procedure for removing microparticles of the inflamed pulp from the roots, i.e. affected tissues. This is a particularly labor-intensive process, since the final effect of caries treatment depends on the quality of the work.
Clinical case: a patient has caries that has developed into pulpitis. When opening the tooth, the dentist diagnosed an infection and a severe inflammatory process; it was recommended to remove dead pulp tissue from the roots. If the work is not performed perfectly, an infection gets into the roots, a filling is placed on top, and the pathological process already develops under a thick layer of filling material. The toothache does not subside, the patient goes to the doctor again or endures the pain, quenching it with medications, and eventually loses the tooth. That is why, in case of caries, pulpitis and other problems, it is important to contact trusted doctors who perform high-quality root cleaning. It is advisable for the dentist to work with a microscope - multiple magnification allows you to monitor the process of cleaning the canals from remnants of pulp tissue.
One tooth may have two or more tubules, which are localized in the layers of the periodontium. The main task of the canals is to be a connecting link between the crown pulp and the nerves.
More than 10 years ago, deep caries and advanced pulpitis were the reasons for removing a unit, but now, thanks to effective cleaning and treatment of the canals, it is possible not only to preserve the crown, but also to restore its integrity to an ideal result.
Features of dental canal treatment
Differences in the structure and functions of the “representatives” of the dentition largely determine the nature of the treatment approach. Treatment of canals for different groups of teeth has its own nuances.
Front tooth canal treatment
The front teeth most often have one canal. They are often curved and difficult to pass through for instruments. In order to preserve aesthetics, the opening of the cavity of these teeth is carried out from the vestibule of the oral cavity. Due to their frontal location, it is important to prevent tooth enamel from darkening, so filling materials containing dyes are not used.
Treatment of wisdom tooth canals
Wisdom teeth can have more than 5 canals; they often have a branched structure, which is not always revealed by x-ray examination. These factors, along with the marginal location of the “eights”, significantly complicate the high-quality treatment of root canals. At the final stage of treatment, various filling pastes are traditionally used.
Root canal treatment of temporary teeth
Endodontic treatment of tooth root canals is usually used only at the stage of root stabilization. When choosing the optimal treatment tactics, it is necessary to take into account the specific structure of temporary teeth. The small thickness of the canal walls, the insignificant degree of dentin mineralization and the relatively large size of the apical foramen are the main reasons for special caution during instrumentation. Zinc oxide eugenol and iodoform pastes, as well as materials based on calcium hydroxide, are usually used as filling agents. They are not toxic to the permanent tooth germ and are able to dissolve along with the temporary root.
The dangers of treating periodontitis at home
The desire of some people to avoid visiting the dental office by any means and continue to endure pain cannot be explained. At the same time, patients persistently practice self-medication, search for recipes on the Internet, rinse their mouths with herbs and smear their sore teeth with homemade compounds of dubious content.
Unfortunately, none of the diseases mentioned in the article can be treated at home. Any method that has been proven over the years, which refers to grandmother’s recipes, will not heal, but will only ease the pain and help the outflow of purulent contents. Remember, the use of this or that non-traditional method of treatment must obtain the approval of a doctor.
Painkillers are also only allowed in limited quantities. Many drugs have a strong and negative effect on the liver and gastrointestinal tract. Therefore, it is unacceptable to constantly relieve pain with pills. And heating a sore tooth, trying to reduce the level of discomfort, is strictly prohibited!
Taking self-prescribed antibiotics will not be successful, because the drug is not able to penetrate into the root canals. It will also not be possible to disinfect and eliminate the source of inflammation by rinsing your mouth. In addition to the warnings voiced, let us remind you that the pathogenic microflora of carious tissues is extremely resistant to drugs, so it cannot be destroyed by taking drugs; drilling is required.
It is better to direct all unspent energy to the prevention of dental diseases. Choosing the right toothbrush, getting into the habit of flossing, and getting regular professional teeth cleanings at your doctor's office are the foundations of oral health.
Mistakes and complications in the treatment of dental pulpitis
Dental treatment during pregnancy 2nd trimester
Treatment of dental caries using the Icon method without preparation
Treatment of pericoronitis of the wisdom tooth in the lower jaw
Restoration of tooth enamel, price, drugs
Cervical caries on the front teeth: causes and treatment
Retreatment of tooth canals before prosthetics, with granuloma, cyst and aching pain
Stages of tooth canal treatment
Endodontic treatment usually lasts several hours and includes a number of stages.
- Removal of the pulp (pulpectomy).
The inflamed soft tissue of the tooth is eliminated. - Root canal sanitation.
The procedure is a “cleaning” of bacteria and dead tissue elements. Pulpectomy and canal sanitation pursue one of the most important goals - eliminating existing inflammation. - Channel formation.
The root canal, freed from pathological contents, undergoes appropriate treatment. In addition to ensuring good passage of the canal, it is imperative to ensure that its apex reaches the apical part of the tooth. - Canal filling.
The last stage of the intervention is filling the root canal with filling material, followed by grinding.
When is endodontic intervention indicated?
Endodontic treatment is carried out in the following cases:
- Inflammation of the coronal and root pulp - pulpitis. Moreover, the form of the disease can be both acute and chronic.
- Periodontitis.
Inflammation of blood vessels and nerve fibers is observed in complicated forms of caries, with a cracked tooth. Inflammation can also be a consequence of injury.
Are there any contraindications for this procedure?
Like any dental procedure, endodontics is contraindicated in a number of cases:
- Vertical incisor fracture.
- Too narrow, impassable dental canals.
- Damage to periodontal tissue.
Treatment of teeth with problematic root canals
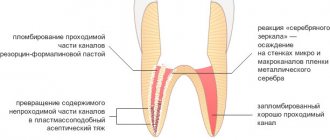
Filling dental canals
A relatively simple technology for treating tooth canals is filling with a special paste with or without a pin. According to the “gold standard” of endodontics, the canals are also filled with a latex-like material - gutta-percha. Several methods of its use have been developed, including the Termafil system, lateral condensation, injection or liquid thermogutta-percha (vertical condensation). In some cases, in particular when treating a tooth canal cyst, filling is carried out with a substance based on calcium hydroxide (copper-calcium hydroxide “depopheresis” method). However, special nanocomposite materials are increasingly used in dentistry.
Treatment under a microscope
The age-old “tough nut to crack” for the dentist is curved or branched root canals of the teeth. A dental microscope, often in combination with a laser, allows you to completely pass through them and adequately process them along their entire length to reduce tissue trauma. Sometimes it becomes necessary to treat a sealed tooth canal with the evacuation of remaining material of various nature, for example, fragments of fillings, tissue fragments and even instruments. Then a microscope also comes to the rescue. Read more about the technology in a separate article.
What are the types of tooth impaction?
There are two types of retention - partial, in which part of the tooth is visible from the gums, and complete - in which the tooth is completely located under the gum tissue and/or jaw bone.
Such teeth can also be positioned differently, both being in “their” place in the dentition and occupying an incorrect position outside the dentition.
- Vertical
- Horizontally.
- At an angle to the jaw
If a tooth does not erupt in the right place beyond the border of the dentition, they speak of tooth dystopia.
There are even reverse retentions, when the tooth lies “upside down,” that is, upside down with its roots.
There may be only one impacted tooth in the dentition, or two impacted teeth may be located symmetrically. This problem concerns both milk and permanent teeth.
If your tooth hurts after root canal treatment
If after root canal treatment your tooth hurts when you press it, this is normal. This phenomenon is associated with insufficient anesthesia in the area of endodontic intervention. Another reason why a tooth hurts after canal treatment is excessive treatment with the instrument moving beyond the apical foramen.
How long does a tooth hurt after root canal treatment? Sometimes pain persists for several days due to intensive intervention in the tissue structure in such a limited area. A similar situation occurs when an excess amount of filling material is placed into the canal, which causes discomfort when pressure is applied to the walls. As a result, the tooth “aches” after canal treatment. In any case, the presence of post-filling pain signals the need for a second visit to the dentist.
Doctor's orders during therapy
At the beginning of treatment of periodontitis, a specific medicine such as Crezofen, which is considered an excellent antiseptic, is usually placed inside the opened tooth canals.
Additionally, rinses with Miramistin or analogues are prescribed, a drug against the development of allergic reactions (Suprastin, for example) and an anesthetic are suggested.
If necessary, the doctor prescribes antibiotics if he sees that the situation is advanced and almost borders on sepsis. A locally acting antibiotic like Lincomycin, which is routinely preferred by dentists, is not suitable here. You will need weapons of mass destruction of bacterial microflora - Ciprofloxacin, Augmentin, Amoxicillin, etc.
If the patient experiences undesirable changes in health status or increased pain, it is recommended not to delay going to the hospital.
In case of exacerbations of chronic periodontitis, when the acute picture of the disease is leveled, therapy involves the installation of temporary fillings in the root canals. This is both obstruction and treatment at the same time. Calcium hydroxide, which is part of the filling material, acts as the basis for the regeneration of bone tissue in the area of inflammation. This procedure takes up to 90 days and all this time a temporary filling in the canal promotes healing of the affected area.
Such conservative therapy for small granulomas becomes a great help for the doctor in healing the disease and allows, in most cases, to avoid traumatic surgery. However, intervention cannot be avoided if the diameter of the cyst exceeds one and a half centimeters. It is not possible to heal formations of this size in a gentle way.
Possible complications
Not all cases go smoothly. Let's consider the main problems that arise after the procedure.
- Perforation.
The phenomenon is the formation of holes between the dental canals and surrounding tissues. Treatment of perforation consists of medicinal treatment and filling. - Cheek swelling.
The reason why the cheek is swollen after root canal treatment is believed to be the impregnation of the periodontal tissues and mucous membranes with an anesthetic drug, which themselves are quite loose and easily absorb liquid. - Instrument fracture.
The probes for passing through the channels are very thin. If they break during medical procedures, the fragments are removed with special devices. Modern dental instruments made of nickel-titanium alloys are less susceptible to wear and break less often. - Adverse reactions to medications.
The range and severity of side effects of modern anesthetics are minimal. Before treatment, the doctor must collect an allergic history - information about drug intolerance - and the likelihood of a full-blown allergic reaction is practically reduced to zero. Adverse reactions of moderate and minor degrees are mostly short-term, can be easily corrected or can be overcome by changing the drug. - Other complications.
Situations such as swallowing particles of fillings, tooth dust, and small instruments now practically do not occur thanks to the use of a rubber dam - a latex plate that separates the tooth or teeth being treated from the oral cavity.
What is dangerous about severe inflammation of tooth tissue?
If measures are not taken in time, the inflammatory process can lead to:
- to the formation of granulomas, cysts, abscesses;
- pulp death;
- loosening of teeth;
- removal or loss of teeth;
- spread of infection to the jaw bone (flux);
- development of general diseases, including myocardial infarction.
It is very important to start treating tooth inflammation on time, and even better, to prevent it. Many clinics provide services for the treatment of dental inflammation. It is worth choosing one that has gained a lot of experience, has its own diagnostic base, and provides guarantees for the doctor’s work.
When is tooth extraction necessary after root canal treatment?
It happens that you have to part with a treated tooth. Typically, such a sad outcome is due to the following factors:
- initially unsatisfactory root canal treatment with the development of poorly controlled inflammation;
- some cases of wisdom teeth treatment;
- the complexity of the anatomical structure of roots and canals in a particular patient;
- late request of the patient for specialized help, in which adequate therapeutic measures do not lead to the desired result.
Symptoms of tooth inflammation
Inflammation is the body's response to bacterial attack. Tissues begin to produce immune cells, signaling the hematopoietic organs that more white blood cells are needed. As a result, the vessels dilate, and the place where the microbes have penetrated swells and turns red. Nerve endings connect the pain syndrome so that we react as quickly as possible.
What is the cost of treatment?
How much does root canal treatment cost? The cost largely depends on the method used and the quality of the materials. When using laser and microscopic technology, nanocomposites and other advanced developments, the cost of tooth treatment with canal filling increases significantly. Approximate prices for root canal treatment in Moscow with gutta-percha filling and composite filling are presented in the table below.
| View | Price |
| Single channel tooth | 9,500 – 12,5000 rubles |
| Double channel tooth | 11,000 – 14,500 rubles |
| Three-channel tooth | 13,500 – 17,000 rubles |
The cost of root canal treatment should not be the determining factor in choosing a clinic. Contact only dentistry with a good reputation and experienced specialists who use modern equipment and the latest techniques in their work. Remember - the future fate of your teeth and the aesthetics of your smile depend on the quality of canal treatment!
Causes
Accurate diagnosis is important for a positive treatment outcome. It is this that allows you to determine why the tooth is inflamed. There are 3 diseases hidden under the general term.
Pulpitis
Microbes penetrate through the dentin layer to the neurovascular bundle - the pulp. People call it a nerve. Usually, this happens with deep caries. The pulp is penetrated by nerve endings. The pain is often acute and difficult to endure. But sometimes it is not strong, periodic. We ignore it and the inflammation becomes chronic, destroying the pulp. A small bun makes a huge difference:
- produces secondary dentin, therefore, although the height of the teeth changes throughout life, they do not disappear completely;
- participates in tissue metabolic processes;
- conducts nerve impulses.
When the pulp dies, the tooth is said to become “dead.” Such teeth are quickly destroyed.
To treat pulpitis in dentistry, therapeutic and surgical methods are used. In the first case, medications are placed into the tooth cavity and closed with a temporary filling. After some time, the tampon with the medicine is removed and the tooth is filled. This method does not always help relieve inflammation inside the tooth.
If the process has gone far, the pulp or part of it is removed and then a permanent filling is placed.
Periodontitis
Under the crown of the tooth there is connective tissue - periodontium. As a result of injury or poor treatment, microbes penetrate there, causing inflammation of the tooth root - periodontitis.
.
There is an apical form, when only the apex is affected, and a marginal form, when all the tissue around the root is infected.
Symptoms of periodontitis:
- pain while eating or when jaws touch;
- feeling that the tooth stands out from the row (has become taller);
- temperature increase;
- tissue redness;
- tooth mobility;
- discharge of pus.
Periodontitis is an insidious enemy. Often the disease occurs without symptoms. It can only be suspected when the signs of the disease become pronounced: roots are exposed, gums bleed, pus is released, bone tissue decreases.
Treatment depends on the type of periodontitis and severity:
- Therapeutic method
The doctor opens access to the root canals, removes part or all of the pulp, and installs drainage to drain the pus. After a few days, the drainage is removed, the canals and tooth are processed and filled. It is recommended to place a crown on such a tooth.
- Surgical method
They resort to it if fibrosis has developed or there are granulomas.
Dentist:
- Cuts off the root tip
- Removes 1 root in multi-rooted teeth
- Amputates the root but leaves the crown intact
- Removes a tooth
- Performs separation (cuts the tooth in half, cleans it and puts it back together)
A course of antimicrobial tablets helps relieve inflammation inside the tooth.
Periodontitis
Periodontium is the fibers that hold the tooth in its socket. Plaque allows bacteria from it to penetrate into the periodontium and begin to rapidly multiply, forming a periodontal pocket. From the pocket, it is easy for them to get under the crown of the tooth and cause an inflammatory process there.
Before treating tooth inflammation under the crown, periodontal pockets are curetted, freeing the surface from tartar and plaque. Then they begin other manipulations: getting rid of caries, splinting teeth. Often, for periodontitis, a course of antibiotics is prescribed. The inflammation must be stopped so that the tooth does not have to be removed.
Medicines from the pharmacy
It is better to use antibacterial and antimicrobial agents that do not contain alcohol. This way, you will protect the delicate tissue of the damaged gum from unnecessary burns.
- Miramistin.
It has the power to destroy bacteria, viruses, and fungi. You need to use a solution with a concentration of one hundredth of a percent. It is practically harmless. Suitable for babies and pregnant women. Use both as a solution and as a spray. Apply 3 times a day for a week.
- Chlorhexidine is
active against bacteria and some types of viruses. A solution with a concentration of no more than 0.05% is used. Miramistin is an order of magnitude cheaper. Maintains effect for up to 4 hours.
- Hydrogen peroxide
is a classic option. ITS three percent solution is a powerful antiseptic. However, use it yourself with caution. Contact with the wound produces foam, which can damage the blood clot. The liquid itself can cause irritation of the mucous membrane.
- Furacilin solution.
Used for purulent inflammation of the wound. In pharmacies it is available in liquid form and in tablets, from which you need to make a solution yourself. Crush 10 yellow tablets and dissolve in a liter of water. Rinsing is not recommended; it is better to use baths.
You can use decoctions
from chamomile
,
calendula, oak bark, sage, St. John's wort and eucalyptus.
On the effectiveness of anti-inflammatory herbs
in
In this case, you need to consult a dentist.
If the wound after tooth extraction is large and there is a risk of damaging the blood clot, it is better to prefer baths to rinses.
Take a sip of the solution into your mouth, maintain the liquid in the wound area and spit it out.
Attention! Do not use potassium permanganate. Reasonable people abandoned it long ago - it burns mucous tissue.
How are impacted teeth diagnosed?
Impacted teeth are often “found” by accident during an X-ray diagnosis for another dental reason. If a patient asks about orthodontic treatment and is missing some teeth, or has symptoms that may be caused precisely by the presence of hidden impacted teeth, then a special diagnosis is carried out.
The problem of impacted teeth is solved by two specialized dentists - an orthodontist and a surgeon, so the patient will have to undergo diagnostics by an orthodontist and diagnostics by a surgeon. Most of the diagnostic procedures will be general, and the key is x-ray diagnostics, and it is preferable to do CT - computed tomography (3D diagnostics). Unlike an orthopantomogram (OPTG), it shows the spatial location of the impacted tooth in the jaw and relative to other teeth, which is very important for the surgical stage of traction - exposing its crown, because allows the surgeon to choose the optimal “approach”.
What complications do impacted teeth cause and why do they need to be “extracted”?
It is difficult for the patient to immediately understand what danger “hidden” teeth can pose, but it is really serious.
Semi-retinated teeth cause inflammation of the “hood” with which they are covered and adjacent tissues, and this provokes purulent inflammation.
Fully impacted teeth that lie in the jaw can behave like a foreign body; they put pressure on neighboring teeth, causing their displacement and a number of other problems.
In this case, the patient experiences pain and fever in case of inflammation, a feeling of pressure and discomfort in the jaw, neuralgia or numbness of part of the face.
If we list the diseases that can result from impacted teeth, it will become clear that this is a real “time bomb” that can detonate at any moment.
What diseases can be caused by an impacted tooth:
- periodontal cyst,
- caries of neighboring teeth and their roots,
- pulpitis,
- pericoronitis,
- periostitis,
- periodontitis,
- purulent lymphadenitis,
- inflammation of the trigeminal nerve,
- odontogenic sinusitis,
- abscess,
- phlegmon,
- resorption (resorption) of the roots of adjacent teeth,
- bad habits: mouth breathing, infantile swallowing, inserting the tongue into a dental defect,
- problems with biting food,
- malocclusion, displacement of interdental contacts, crowding of teeth.
Pain after a filling falls out and other unpleasant consequences
Simple recommendations for patients on what to do when a filling falls out and a tooth hurts:
- You need to rinse with a solution of baking soda and salt.
- You can take a painkiller, it could be Ketanov or Analgin.
- During the inflammatory process, the temperature may rise. It must be knocked down after exceeding 38.5° C. For this, antipyretics are used.
- If there is bleeding from a tooth, you should immediately consult a doctor. There can be many reasons for this phenomenon, and it will be possible to accurately determine the possible problem only after an appropriate examination.
You can find many tips on how to numb a tooth at home, but the most effective option is to rinse and take appropriate medications.
When a filling with arsenic falls out, you need to carefully remove the remaining medication with a cotton swab and rinse the tooth cavity with a soda solution.
Diagnostic methods
Diagnosis of tooth perforation is based on patient complaints and visual examination of the oral cavity. In most cases, perforation in the crowns of teeth can be recognized using an x-ray. If there is a suspicion of perforation localized in the area of the bottom of the dental cavity, an X-ray with contrast is performed. In any case, an image is taken that allows you to determine not only the presence of perforation, but also to identify complications caused by the pathology.
When holes form in the dental canal, additional equipment and tools are required to identify them. It is easier to diagnose perforation when there are already symptoms: sharp pain, mild bleeding, changes in the movement of the instrument during dental treatment.
With old perforation formed in the canal, symptoms appear, which in their manifestations resemble periodontitis. It is diagnosed along with inflammation, which affects the tissues located near the roots of the teeth. In the presence of such perforation of dental units, characteristic pain in the tooth is observed, which appears when pressing on the damaged segment, swelling of the gums, concentrated in the area of inflammation.
Tooth perforation, localized in the root of the teeth, is diagnosed using a paper pin by immersing it in the canal. The location of the perforation is determined by the trace of blood that remains on the paper.
How is surgery performed to expose the crown of an impacted tooth?
- As a preliminary stage, preparation for the operation is carried out. The patient undergoes professional hygiene and sanitation to reduce the amount of infection in the oral cavity and speed up postoperative healing.
- The operation to expose an impacted tooth is performed under local infiltration anesthesia and is considered a fairly serious surgical intervention.
The operation to expose the crown of an impacted tooth and install an orthodontic element on it can be carried out according to 2 schemes:
I Delayed bracket installation.
- The mucous membrane in the projection of the crown of the impacted tooth is excised, the entire crown of the tooth is exposed, and a special tampon is installed in the wound.
- After 2-3 days, a button or bracket is installed on the crown of the exposed tooth, which is tied to the orthodontic arch and traction begins.
II Bracket installation during surgery
- The dentist-surgeon peels off a small mucoperiosteal flap and exposes part of the crown of the impacted tooth, onto which the locking element is immediately fixed.
- The bracket is tied to an orthodontic arch or additional devices.
- After installing the orthodontic element, the flap of tissue is placed in place and the wound is sutured.
The disadvantage of this method is that in this case, repeated surgical intervention is possible if the bracket on the tooth comes off.
After surgery, the patient is prescribed antibiotics and antiseptic rinses, if necessary, to speed up healing. Light, non-traumatic food is recommended.
Loss of fillings in children
When a child’s filling falls out, you should not ignore the problem, even if the teeth are baby. Caries and other diseases can provoke severe pain and the development of an inflammatory process.
What to do if a temporary filling falls out of a baby tooth:
- Call your doctor, consult and make an appointment as soon as possible.
- Ensure that your child maintains good oral hygiene.
- Rinse your teeth regularly to remove food debris.
Important! Fillings on baby teeth fall out for various reasons, and only a specialist can determine what causes this phenomenon. So, in any case, you cannot do without a visit to the dentist.