Anatomy, physiology
The periodontium
is a complex organ of the oral cavity surrounding the teeth, formed from specialized tissues. It is located on the jaws and its main functions are to support (support) the teeth and their nutrition and innervation.
Nutrition (trophism) is provided by blood and lymphatic vessels that supply oxygen and metabolic products to the periodontal tissue.
There are four main anatomical and functional elements of the periodontium:
- gum,
- periodontium,
- alveolar bone with periosteum,
- root cement
The gum is a soft tissue - a mucous membrane covering the alveolar processes, with an underlying connective tissue layer.
It contains lymphatic vessels (they are involved in regulating fluid pressure in tissues and protecting against microbial agents).
Through the periodontium - the ligament of the tooth, the latter is fixed in the jaw bone.
Periodontium
(otherwise known as desmodont) is a connective tissue formation surrounding the tooth and located between the root cement and the inner cortical plate of the alveolar bone.
This ligament, consisting of the main substance, fibers and cellular elements, like an elastic gasket, absorbs the load on the tooth, giving it minimal mobility. When periodontal disease and death occur, fusion of the bone with the tooth – ankylosis – can occur.
The next element of the periodontium is cement, which is also a hard tissue covering the root of the tooth. It is formed by collagen fibers directed along the root and an adhesive substance.
Bone
The alveolar process, in which the tooth is strengthened by periodontium, is composed of outer and inner dense plates and a spongy part between them.
Spongy bone consists of trabecular septa, the direction and shape of which is determined by the load on the jaws and teeth, and bone marrow.
Bone tissue contains mainly crystals of hydroxylapatite (inorganic) and small amounts of water and organic substances.
The cellular elements of bone - osteoblasts, osteoclasts and osteocytes, under the influence of the nervous and humoral system, determine changes in the shape, volume and quality of this tissue.
The bone tissue of the alveolar process is covered with a dense connective tissue structure - the periosteum; it, with the vessels located in it, plays a significant role in the blood supply to the bone.
The blood supply provides tissues and anatomical formations with organic and mineral substances.
At the level of the enamel-cement junction (neck of the tooth), an anatomical formation stands out in the marginal part of the gum - a vascular cuff, which, like an elastic band, ensures a tight fit of the gum to the tooth due to hydrostatic pressure.
The main source of blood supply to periodontal tissue is the external carotid artery with the maxillary and mandibular arteries branching from it.
Venules and veins collect blood into the internal jugular vein. The periodontium is innervated by the trigeminal nerve and the superior cervical sympathetic ganglion.
Among others, there is an anatomical formation - the dentogingival junction
. This is the connection between the gum epithelium and the neck of the tooth.
It is physicochemical: molecules of epithelial cells adhere to cement structures through gingival fluid cells.
Gingival fluid produced by periodontal tissue plays the role of a protective barrier against microorganisms through the activity of phagocytes and its chemical properties. It should be noted that the periodontium is washed by saliva. It is secreted by the major and minor salivary glands.
In addition to water (99.42%), saliva contains organic substances, salts and trace elements. Organic substances enter the oral fluid from blood serum and are secreted by the salivary glands and microorganisms present in the mouth.
Of the inorganic substances, calcium phosphate and calcium bicarbonate (they take part in the formation of tartar), phosphate and sodium chloride are important.
Diagram 1: periodontium
. a – submucosal layer with lymphatic vessels; b — mucous membrane of the attached gum; c - spongy bone of the alveolar process between the plates of the compact substance; d – periodontal fibers are woven into the root cement; e – gingival margin with vessels of the gingival cuff; e – dentogingival junction; g – tooth enamel; h – dental pulp; and – root cement; j – root dentin.
Age-related changes in periodontium
In the periodontium, with age, there is a decrease in the number of collagen fibers and a decrease in their quality. The epithelial layer of the mucosa becomes thinner, and keratinization is disrupted.
The bone tissue of the alveoli becomes less dense, the cortical layer atrophies.
Periodontitis
In children, periodontitis is more common, localized in the area of 1–2 or groups of teeth in the frontal area of the jaws with crowded teeth or dental anomalies, with anomalies in the structure and attachment of the frenulum of the tongue, lips, and the small vestibule of the oral cavity. The following signs are characteristic of periodontitis:
- complaints of bleeding gums, sometimes pain in them during exacerbation, bad breath; with initial changes, complaints may be absent;
— symptomatic gingivitis (catarrhal, hypertrophic);
— deposition of supra- and subgingival soft plaque and tartar;
— destruction of the periodontal epithelial attachment;
- formation of periodontal pockets with serous or purulent contents;
— destruction (destruction) of the edge of the alveoli (interalveolar septa), determined on an x-ray;
- exposure of the necks and roots of the teeth;
- tooth mobility and traumatic occlusion.
In the initial form of periodontitis, there may be no complaints; mildly expressed symptoms of catarrhal gingivitis, plaque deposition, false periodontal pockets up to 2–2.5 mm are clinically determined, the teeth are stable, the necks of the teeth are not exposed. X-rays reveal vagueness or destruction of the cortical plate at the apexes of the interalveolar septa and slight osteoporosis of their spongy substance.
In mild forms of periodontitis, patients complain of bleeding gums when brushing their teeth; symptomatic catarrhal gingivitis, small amounts of plaque and tartar deposits, periodontal pockets up to 3.5 mm deep, and slightly or 1st degree tooth mobility are clinically determined. The radiograph reveals the absence of a cortical plate at the apexes and lateral sections of the interalveolar septa, expansion of the periodontal fissure in the cervical region, and subsequently destruction of the interalveolar septa up to 1/3 of the root length; foci of osteoporosis of the interalveolar septa. In the chronic course, osteoporosis is not clearly expressed, and during exacerbation it is diffuse in nature.
In the moderate form of periodontitis, complaints of bleeding gums appear during brushing teeth and eating, symptomatic gingivitis, deposition of tartar and plaque, periodontal pockets up to 5-6 mm with serous or purulent discharge are clinically determined; mobility of teeth of the 1st–2nd degree, exposure of the roots of the teeth occurs. The X-ray shows destruction of the interdental septa from 1/3 to 1/2 of the root length, expansion of the periodontal fissure, osteoporosis is insignificant in the chronic course, and diffuse in case of exacerbation.
Severe periodontitis is characterized by complaints of bleeding and sore gums when brushing teeth and eating. Clinically, symptoms of catarrhal or hypertrophic gingivitis are detected, significant deposits of supra- and subgingival calculus and soft plaque, pockets more than 5-6 mm deep, filled with granulations and purulent contents. The radiograph shows destruction of the interalveolar septa within 2/3 of the root length, diffuse osteoporosis of the remaining bone tissue of the septa, mobility of teeth of the 2nd–3rd degree, exposure of the roots, displacement of teeth and traumatic occlusion.
Diagnosis of periodontitis in children
Examination of a child with periodontitis begins with a study of complaints, medical history and life history. Anamnestic data includes information about the physical and intellectual development of the child, common and infectious diseases suffered and existing at the time of examination. When examining a child, pay attention to his posture, since it is a factor in the full development of the child and a risk factor for anomalies in the development of the dental system.
Examination of the face in front and profile at rest and when closing teeth, during conversation and facial movements allows us to determine functional deviations in accordance with facial characteristics. Thus, the “thimble” symptom in the form of pinpoint retraction of the skin on the chin is a sign of impaired swallowing function. Pay attention to the state of tone of the facial and chewing muscles at rest and during function. The type of breathing (nasal, oral, mixed), the position of the lips (closed, open, tense or atonic), the state of the red border of the lips (color, volume, turgor, architectonics, etc.) are determined, which makes it possible to establish a violation of the basic functions of the dental system and bad habits. The condition of the temporomandibular joint and the lymphoid apparatus of the maxillofacial skeleton is assessed.
A study of the vestibule of the oral cavity allows us to judge its depth, severity and nature of attachment of the labial frenulum to the alveolar process, the state of the mucous membrane covering it, the degree of teething, their position in the dentition and the relationship of the jaws. The depth of the vestibule of the oral cavity is determined by horizontal abduction of the lower lip by the distance from the edge of the marginal gum to the level of the transition of the mucous membrane to the lip. The vestibule is considered shallow if the specified distance does not exceed 5 mm, medium with a depth of 5 to 10 mm, and deep over 10 mm. The area of the attached (alveolar) gum is measured in millimeters, as well as the depth of probing of periodontal pockets using a graduated blunt probe. In addition, the localization of the gingival margin relative to the enamel-cementum boundary (degree of root exposure) and the presence of bleeding upon light probing must be determined.
When examining the oral cavity, the condition of the salivary glands, the position, size of the tongue, the structure and nature of the attachment of the frenulum of the tongue, the shape and relationship of the dental arches, and the presence of crowding of teeth in the frontal area are assessed. The teeth are examined to identify carious lesions, and the quality of the applied fillings is assessed. The mobility of teeth and their occlusal and interdental relationships, the presence of plaque and tartar are determined.
To objectively identify the symptoms of gingivitis and its prevalence, the Schiller-Pisarev test is used, and the degree of gum inflammation is determined using the PMA index. The degree of destructive changes in the periodontium is determined by the periodontal index. Assessment of the hygienic state of the oral cavity is carried out using the Fedorov-Volodkina, Green and Wermillion hygienic indices. It is mandatory to determine the uniformity of the occlusal load using the fingerprint method (occlusiogram), as well as radiographic examination of the periodontium. If X-histiocytosis is suspected, an X-ray examination of the jaws and skull bones is performed.
In addition, a study of the child's developmental history is necessary; conducting clinical blood tests (general, for glucose levels to exclude diabetes), as well as determination of immunoglobulin levels to exclude immunoglobulinemia, a general urine test, and if X-histiocytosis is suspected, for neutral fat. According to indications, cytological and microbiological methods are used to examine periodontal pockets. The child must be examined by a pediatrician, hematologist, endocrinologist, immunologist, pediatric gynecologist, psychoneurologist, etc. in order to identify and treat systemic diseases that may affect the course and outcome of treatment of gingivitis and periodontitis.
Differential diagnosis
Periodontitis must be differentiated from chronic gingivitis and changes in the periodontium with X-histiocytosis, diabetes mellitus, constant and cyclic neutropenia, etc. Some difficulties arise in the differential diagnosis of the initial forms of periodontitis with gingivitis. X-ray data are decisive in this case. With chronic gingivitis, as a rule, there are no changes in the alveolar bone on the radiograph; only in rare cases, with long-term and untreated gingivitis, osteoporosis of the interalveolar septa is observed. When analyzing radiographs, it is necessary to take into account the variability of the shapes of the interalveolar septa in children, as well as the fact that the periodontal gap in the area of the necks of the teeth before the formation of the permanent dentition is wider than in other areas; during the period of teething, the interalveolar septa are not formed, the cortical plate at their apexes is not determined.
When differentially diagnosing periodontitis with changes in the periodontium with X-histiocytosis, one must keep in mind that with X-histiocytosis, along with changes in the alveolar bone, there are foci of bone tissue destruction in the body and branches of the lower jaw. In diabetes mellitus, vertical resorption of the interdental septa with funnel-shaped, crater-shaped pockets predominates, which does not extend to the body of the jaw. With constant and cyclic neutropenia, the process is limited to the interalveolar septa and has clear contours.
With cyclic neutropenia, exacerbation of the process occurs at strictly defined intervals, characteristic of a particular child (usually 21 days) and lasts 4-5 days.
Prepubertal periodontitis
Occurs in children under 11 years of age. The most common form is a generalized one. The disease begins during or shortly after the eruption of baby teeth and is manifested by a violation of the attachment of the gums to the teeth and severe destruction of the alveolar bone, leading to premature tooth loss in children from the age of three. The early and aggressive course is due to the fact that such patients have immune defects - there are few monocytes and polymorphonuclear leukocytes in the blood. All children from birth have decreased resistance to infections, furunculosis, pustular skin diseases, otitis, and pneumonia. The children are pale and have low nutrition. This disease is associated with microorganisms of the bacteroid type: Porphyromonas gingivalis, Actinobacylus actinomycetemcomintans. Infection occurs from parents, the window of infection is from 1 to 3 years. It begins with the primary destruction of the periodontium, while at first there are no symptoms of gum inflammation. Subsequently, the architectonics of the gingival margin changes, the gums seem to recede, the necks of the teeth are exposed, deep periodontal pockets form, and then inflammation develops. X-ray reveals vertical destruction of the alveolar bone. Subsequently, mobility, movement and loss of teeth occur. There are no symptoms of bleeding or pain. There is no tartar, the teeth are covered with a soft plaque. Children first lose their milk teeth, then the process spreads to the rudiments of permanent teeth, they erupt early, similar changes occur with them, and by the age of 14–15 all teeth fall out. However, the pathological process does not extend beyond the alveolar bone. With the loss of permanent teeth, the destructive process in the jaws stops.
The same changes in the periodontium, combined with palmoplantar hyper- or dyskeratosis in the form of cracks on the palms, feet, forearms, and increased sweating, are also observed in Papillon-Lefevre syndrome. There is evidence in the literature that taking tetracycline antibiotics for Papillon-Lefevre syndrome during the primary dentition period prevents the development of generalized periodontitis in the permanent dentition and the loss of permanent teeth.
Pubertal (teenage) periodontitis
There are 2 forms: localized and generalized. Localized pubertal periodontitis is observed in practically healthy children and adolescents without systemic diseases. It is characterized by rapid and severe destruction of the alveolar bone in the area of the first permanent molars, and sometimes the incisors. Clinically, mild inflammation (which may be absent) and a small amount of plaque or tartar are observed. Bone tissue destruction progresses 3–4 times faster than with periodontitis in adults. Currently, this disease is associated with a bacteroid of the Actinobacylus actinomycetemcomintans type. In most cases, it occurs in children whose parents are carriers of this microorganism. It enters the periodontal tissue soon after teeth erupt. The process occurs with minimal inflammatory reaction. The rapid spread of the process is due to the fact that specific microflora not only populates the groove and subsequently the periodontal pocket, but also penetrates deep into the periodontal tissues, including bone tissue, where it is quite persistently preserved. On the other hand, this microorganism has the ability to suppress the chemotaxis of leukocytes, and antibodies in such cases do not have time to form. The periodontium is rarely damaged after the eruption of permanent teeth, since by this time specific antibodies have time to form and exert their protective effect. Previously, this disease was described as local desmodontosis, local monoalveolysis according to Orban.
Generalized pubertal (teenage) periodontitis is rare. In this case, the process often involves the periodontium of both jaws. It is characterized by an aggressive course, rapid and severe destruction of the alveolar bone. It is commonly called aggressive, or rapidly progressive, periodontitis. According to foreign and domestic literature, a large number of facultative anaerobic gram-negative rods, mainly Porphyromonas gingivalis, accumulate in the area of the affected teeth. The most aggressive course is associated with the combination of this microorganism with Actinobacylus actinomycetemcomintans and Prevotella itermedia. It is with this combination that microorganisms exhibit a sharply positive mutual influence.
Classification of periodontal diseases.
Gingivitis
Gingivitis is an inflammatory superficial disease of the gum tissue.
With gingivitis, there is no disruption of the periodontal junction and bone. Based on the form of manifestation of periodontal disease, the following are distinguished:
- catarrhal gingivitis,
- hypertrophic gingivitis,
- ulcerative gingivitis.
According to the type of course, gingivitis is divided into acute, chronic, aggravated and remission. According to the distribution, gingivitis can be localized and generalized. Without active treatment, gingivitis progresses to periodontitis.
Periodontitis.
Periodontitis is a deep inflammatory disease of the periodontium with destruction of the periodontal junction and bone tissue of the alveoli.
There are acute, chronic course of periodontitis, exacerbation of the disease and remission. Periodontitis can be mild, moderate or severe.
According to the prevalence, this gum disease is divided into generalized and localized periodontitis.
Photo 1. X-ray picture of severe periodontitis. The roots of the teeth are exposed by two-thirds.
2. 1.
Additionally, there is a condition known as
an aggressive form of periodontitis.
This diagnosis can be made by a doctor based on the presence of a set of signs of gum disease. In this case, periodontal destruction is generalized and rapid.
Such periodontitis is typical for ages from adolescence to 35 years. Often the aggressive form of periodontitis is accompanied by gum growth and granulation. During the period of remission, inflammatory manifestations may subside and even disappear.
Periodontal disease
Periodontal disease is a chronic degenerative periodontal disease.
In European and American classification as a separate gum disease
doesn't stand out. Periodontal disease is characterized by a long-term, benign course and almost does not lead to loosening and loss of teeth.
Periodontal diseases - as symptoms of other diseases
There are idiopathic periodontal diseases with progressive destruction of periodontal tissue (periodontal syndrome).
Such conditions can occur when exposed to physical factors (radiation), poisoning, immunodeficiency, diabetes mellitus, eosinophilic granuloma, Papillon-Lefevre syndrome, neutropenia, etc.
Periodontomas. Epulis (epulid) and gingival fibromatosis
Periodontomas are tumors and tumor-like conditions of the gums. The most common of them are epulis (epulid) and gingival fibromatosis.
Gingival fibromatosis is characterized by the proliferation of periodontal tissues, which causes tumor-like damage to the gum tissue. Gingival fibromatosis is most common in adults, but is sometimes diagnosed in children.
The diagnosis of gingival fibromatosis is made by a specialist based on the patient’s complaints, examination data, radiography, and histological examination.
The main reason for the growth of gum tissue, as a rule, is a violation of metabolic processes; drug-induced fibromatosis of the gums is also identified. Treatment of the disease is surgical and consists of excision of the overgrown gum to the periosteum.
Photo 2. Gingival fibromatosis
Gingivitis
Acute catarrhal gingivitis is an inflammatory process with a predominance of exudation. This disease is characterized by complaints of pain, itching, bleeding gums, and refusal to eat. Upon examination, hyperemia and swelling of the papillae, gingival margin, and sometimes the alveolar gum are determined, which leads to an increase in size and a change in the shape of the gingival papillae (not sharp, but rounded). When the alveolar gum is involved, its granularity (symptom of lemon peel), characteristic of healthy gums, disappears. Bleeding gums are detected when you touch them slightly. This form of gingivitis is observed relatively rarely, mainly during teething, as a result of acute trauma (mechanical, chemical, thermal), in acute childhood infectious diseases, and also as a manifestation of allergies, a symptom of acute herpetic stomatitis.
Chronic catarrhal gingivitis is the most common periodontal pathology in children. There may be no complaints; sometimes children notice bleeding gums when brushing their teeth. Upon examination, congestive hyperemia, pastosity, bleeding of the papillae and gingival margin are determined. The marginal gum is thickened like a roller (stretches like a rubber balloon), the surface becomes shiny. The granularity of the alveolar gum disappears.
With catarrhal gingivitis (both acute and chronic), with significant swelling of the gums, a gingival pocket, that is, a false periodontal pocket, can occur. The radiograph shows no changes in the alveolar bone.
Hypertrophic gingivitis is a chronic inflammatory process characterized by an increase in gingival papillae and marginal gums due to the proliferation of fibrous connective tissue and the basal layer of the epithelium. Most often, hypertrophic gingivitis is observed with close position of the teeth, open bite, small vestibule of the oral cavity, short frenulum of the lips, with improper orthodontic treatment, as well as during puberty (in girls with a late onset of menstruation or a long menstrual cycle, when the effect of estrogens predominates) , when taking antiepileptic drugs and blood diseases.
Hypertrophic gingivitis, caused by local factors (crowding of teeth, dental anomalies), is limited in nature, located mainly in the frontal area. Hypertrophic gingivitis, caused by endogenous causes (endocrine pathology, gastrointestinal diseases, etc.), is generalized, characterized by rapid development, a tendency to relapse and resistance to local treatment.
There are inflammatory (granulating) and fibrous forms of hypertrophic gingivitis. The inflammatory form is characterized by: hyperplasia of the gingival papillae, which are covered with granulations; their hyperemia with pronounced cyanosis and swelling; loose tissue and severe bleeding; pain on palpation; thickening of the gingival margin, its separation from the necks of the teeth, chronic catarrhal inflammation of the alveolar gum. False periodontal pockets are identified due to swelling and hyperplasia of the gums. There is a deposition of plaque and tartar. Hypertrophied marginal gum covers one or another part of the tooth crowns.
In the fibrous form, the gingival papillae are enlarged, dense, pale, do not bleed, and are painless.
According to the intensity of productive inflammation, there are 3 degrees of hypertrophic gingivitis:
— 1st degree — hypertrophy of gingival papillae;
— 2nd degree — hypertrophy of the gingival papillae and marginal gums;
— 3rd degree — hypertrophy of the marginal and alveolar gums.
Desquamative gingivitis is clinically characterized by swelling of the marginal gum, sometimes extending to the attached gum, pronounced hyperemia, severe bleeding and pain. A feature of this form of gingivitis is the constant desquamation of the surface layers of the gum epithelium, not only marginal, but also alveolar, as a result of which almost the entire mucous membrane becomes eroded and easily vulnerable. May occur against the background of hypertrophic gingivitis. Children complain of pain when brushing their teeth and eating, the presence of blood in saliva, the specific smell and taste of blood.
Desquamative gingivitis in children develops rarely, mainly during puberty (in girls, usually during a short menstrual cycle, when the action of progesterone predominates).
Etiology and pathogenesis (causes and development) of periodontal diseases
Calculus
The main point in the development of gum diseases such as gingivitis and periodontitis is dental plaque (plaque), which turns into tartar (calculus).
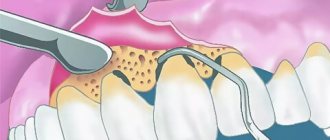
Photo 3. Soft plaque (plaque). Marginal periodontitis.
It is believed that organic soft dental plaque, which is formed from food debris due to poor hygiene, is gradually saturated with calcium from saliva and serum exudate of the gum pockets and is converted into hard tartar.
The latter can be of different hardness and color, which is determined by its composition. It consists of 18-25% organic matter (microbes and dead cells) and 75-82% inorganic matter (calcium, phosphorus, metal salts).
Tartar causes traumatic compression of the gums and prevents the cleaning of the periodontal pocket, promoting the development of microbial agents.
Microorganisms diffuse deep into periodontal tissues, lingering on the surface of the basement membrane and further into the bone tissue of the alveolar process.
Traumatic closure of teeth
In the absence of part of the teeth, in case of violation of the position of the teeth, in case of partial destruction of teeth and other traumatic factors, the remaining teeth are subjected to excessive and inadequate load. The latter, in turn, destroys the periodontium of the teeth.
Improper functioning of the temporomandibular joint (TMJ).
The ANS may be a significant factor in the development of gum disease.