Dental caries is usually classified according to different indicators. One of the most widespread is Vinogradova’s classification, according to which there are compensated, subcompensated and decompensated forms of dental caries. We will tell you more about the symptoms and treatment features of different forms of the disease in this article.
In this article
- How does dental caries occur?
- Three forms of dental caries
- Compensated form of caries
- How is compensated caries treated?
- What is subcompensated caries and what are its features?
- Features of decompensated caries
- How is decompensated caries treated?
- Pulpitis as a complication of decompensated caries
- Periodontitis with decompensated caries
- Is it possible to prevent tooth decay?
- Conclusion
How does dental caries occur?
During caries in hard dental tissues, under the influence of organic acids, first areas of enamel demineralization are formed, and then carious cavities. Acids that destroy teeth are produced by cariogenic bacteria. This occurs during the fermentation process of carbohydrates that we consume in food. According to statistics, caries is the most common dental disease; it affects the teeth of people of any age, including the development of baby teeth immediately after teething.
There are different classifications of caries, in particular the Vinogradova classification. According to this division, there are compensated, decompensated and subcompensated caries.
Bitter sweet truth
Of course, people have known for a long time that “sweets spoil teeth,” but it was possible to prove the role of diet in the occurrence of caries only when, in the course of numerous independent experiments, it was established that streptococci are present in dental plaque in people free from caries. The first step in proving the “guilt” of sugar was taken by Danish professor Frederik von der Fehr from the Royal Dental College in Aarhus. In 1970, von der Fehr conducted an experiment in which a group of volunteers with good tooth enamel completely eliminated oral hygiene - they did not brush or rinse their teeth after eating. Half of them also rinsed their mouths with a 50% sucrose solution several times a day. Lack of hygiene increased the number of bacteria in plaque, but when comparing the condition of the teeth of those who rinsed with a sweet solution with the control group, more obvious signs of caries were found - demineralization of the enamel and the appearance of stains on it.
If earlier, for example, in the not so distant 18th century, sugar was an expensive product and not everyone appeared in the diet, but now, according to dental surveys, most people in Russia and many other countries eat sweets every day. As Edith Kuzmina notes, it is not so much the amount of sweets eaten at a time that is important, but the frequency of its consumption.
Ideally, dentists advise eating sweets as little as possible and replacing fermentable sugars - glucose, sucrose and fructose - with sorbitol, mannitol and xylitol. These polyhydric alcohols have a sweet taste and are often used as sweeteners (for example, for diabetes), and carious streptococci simply cannot utilize them. Natural xylitol is found in strawberries and carrots. And if you still can’t give up sweets, then it’s better to eat them not “alone”, but together with other foods - this reduces cariogenicity. The same sour apples, for example, require copious amounts of saliva, and it dilutes and, having an alkaline reaction, partially neutralizes the acid formed in the mouth after the fermentation of sucrose and glucose.
Three forms of dental caries
Vinogradova’s classification is based on the degree of activity of dental caries:
- The compensated course of caries is characterized by the fact that the pathological process develops slowly, carious cavities are hidden under dense dentin, they are rare, and the disease progresses relatively slowly.
- The subcompensated form of the disease develops slightly faster than the compensated form. It is characterized by the appearance of dark areas on the enamel and horizontal spread without penetrating deep into the tooth.
- Decompensated caries is often multiple and spreads very quickly. With such caries, all teeth located near the cheeks are often affected.
The decompensated form is considered the most severe, in most cases accompanied by complications in the form of pulpitis or periodontitis.
Let's talk about all forms of caries in more detail.
Treatment of caries, is it painful to treat?
Caries is a slow-moving pathological process occurring in the hard tissues of teeth, which develops due to the influence of certain external and internal factors.
At the initial stage of development, caries is characterized by focal demineralization of the inorganic part of the tooth enamel and its gradual destruction, affecting the organic matrix, as a result of which this leads to a violation of the integrity of the hard tissues of the tooth with the formation of cavities in the dentin, and in the absence of timely treatment - to the occurrence of inflammatory complications with side of the pulp, leading to periodontitis.
Treatment of caries is completely painless, since all dental procedures are performed under complete anesthesia.
Compensated form of caries
Among all the options for the course of caries, compensated is the most favorable. In this case, the pathological process is sluggish and destroys dental tissue slowly over several years. With compensated caries, remission is possible, which under certain circumstances can result in relapses. According to statistics, compensated caries develops more often than other forms.
It is characterized by smoothed symptoms:
- Acute pain is most often absent;
- the transition of carious lesions from one stage to another occurs smoothly and imperceptibly over several months or even years;
- with compensated caries, a white spot first forms on the enamel, which gradually darkens, becomes rough and less dense. At the dark spot stage, a painful reaction to temperature or taste stimuli is possible;
- The compensated form of caries is characterized by destruction of dentin while often maintaining the integrity of the tooth enamel. Therefore, the characteristic clinical picture is a carious cavity in a seemingly intact tooth crown.
Caries, statistics
Data from various studies indicate that in equatorial regions (Africa, Asia) caries is less common than in the northern and polar regions (Scandinavia, North America). People living in developing countries also have a higher incidence of dental caries, but in this case this is not due to genetic predisposition or the influence of external factors, but to a much lower availability of dental care than in developed northern countries.
Caries is of infectious origin associated with the activity of microorganisms such as veyonella, lactobacilli and other microbes. Streptococci play a leading role in the development of dental caries disease.
A decrease in resistance to caries is associated with a decrease in the calcium content of tooth enamel, with a decrease in the calcium/phosphorus ratio, as well as with immune disorders in general. Researchers associate the decrease in the body’s immunity mainly with a decrease in the content of secretory immunoglobulin type “A” in saliva, which prevents the attachment of microorganisms to the surface of tooth enamel and thereby prevents the formation of soft plaque, which, with insufficient hygiene, is susceptible to hardening and the formation of hard tartar.
How is compensated caries treated?
The method of treating compensated caries depends on the stage at which it is detected and, accordingly, on the degree of tooth destruction.
At the initial stage of a carious stain on the enamel, non-invasive methods that do not require drilling a dental crown can be effective.
- Remotherapy (remineralization).
Using special pastes, gels, and solutions, tooth enamel is saturated with calcium and fluoride ions - the main components of its mineral composition. They normalize the structure of the enamel, increase its protective properties and resistance to the corrosive effects of acid.
- Deep fluoridation.
It is similar to the remineralization procedure with the difference that the composition of medicinal preparations necessarily includes fluoride. It penetrates deep into the enamel, makes it stronger, has an antiseptic effect, and prevents the teeth from losing calcium and other minerals.
- Fissure sealing.
Fissures are natural grooves on the surface of chewing teeth. They can be of different shapes and depths, and due to their anatomical features, food debris easily accumulates in them. In addition, the enamel in the fissure area is thinner compared to other areas of the dental crown. The sealing method is often used to prevent caries in the chewing teeth of children and adults with deep grooves on their teeth. The essence of the method is that the dentist seals the natural recesses of the dental crown with a special sealant, so that food debris no longer accumulates in them and bacteria cannot multiply.
- Filling.
This method treats a compensated form of caries in the later stages, when cavities have formed in the dentin of the tooth. Most often, the dentin treatment process is painful, so the procedure is performed under local anesthesia. After the anesthetic injection takes effect, the doctor prepares the affected tooth with a drill, removes carious tissue, and then covers the cured tooth with high-quality filling material. The best treatment option is without drilling or filling. Methods of remineralization and deep fluoridation are safe, painless, and do not cause discomfort in the patient. But they are effective only at the initial stages of the carious process.
Therefore, it is important to regularly check the condition of your teeth with a dentist (for compensated forms of caries, a visit once a year is recommended) in order to notice the beginning of caries as early as possible.
Mechanism of destruction
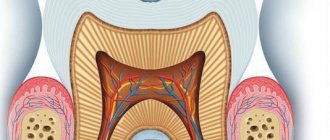
To understand how caries occurs, you first need to know that tooth enamel is approximately 95% composed of the mineral calcium hydroxyapatite Ca10 (PO4)6 (OH)2. Its hexagonal crystals combine into prisms and provide strength to bones and teeth. The enamel of just one incisor contains about 5 million mineral prisms.
Like all hydroxyl (“alkaline”) minerals, hydroxyapatite is destroyed by acids. This happens due to a violation of the notorious acid-base balance, known to everyone from chewing gum advertising. When acid enters the mouth, for example with a sip of wine, our body tries to neutralize it, and calcium from the enamel migrates into saliva. And without calcium, mineral prisms collapse like houses of cards. If the process is repeated, the acids attack the dentin located under the enamel. Then a carious cavity appears in the tooth - a cavity.
Particularly scary are simple organic acids, such as acetic, lactic and citric. Therefore, when we drink wine or eat an orange, the enamel of our teeth is doomed to partial destruction. But acids appear in the mouth even without oranges. Plaque streptococci feed on the carbohydrates we eat, and the by-product of their fermentation is aggressive acids. The simpler the carbohydrate, the faster acid is formed from it. This means that the more often we eat simple carbohydrates (glucose, fructose, sucrose), the more caries progresses.
The enamel that forms the crown of a tooth is the hardest substance in the human body. However, it cannot withstand the chemical attack of the waste products of S.mutans streptococci.
The approximately mechanism of development of this disease was described by the American dental scientist Willoughby Miller at the end of the 19th century, calling it the chemical-parasitic theory. This means that, on the one hand, the appearance of caries is a chemical process, but without parasitic microbes it would not be so large-scale or would be completely neutralized. According to the head of the Department of Caries Prevention at Moscow State University, Edith Kuzmina, three reasons are to blame for the appearance of caries: plaque with bacteria, carbohydrate foods and weak resistance of tooth enamel. This means that there can only be three ways to combat caries: eat as little simple sugars (easily fermentable carbohydrates) as possible, make tooth enamel more resistant to decay, and, finally, rid your teeth of plaque in which streptococci are hidden.
What is subcompensated caries and what are its features?
Subcompensated caries occurs in approximately 25% of children with dental caries. This form is characterized by an average rate of spread of the pathological process. Characteristic features are dull enamel and superficial lesions without deep tissue involvement. Most often, subcompensated caries does not cause discomfort or pain, so it can only be detected during an examination by a dentist.
People with this form of caries are recommended to have scheduled visits to the dentist two to three times a year, as well as oral sanitation and preventive measures.
Features of decompensated caries
The decompensated form of caries is the most intensive type of development of dental disease. Decompensated caries is considered the most severe and dangerous. The first signs of the disease are rough matte enamel, darkening of the fissures; when opening the dental crown, a large carious cavity is most often discovered, and severe pain is noted when probing with a dental probe.
This form of caries develops very quickly and in most cases is accompanied by complications (tooth chipping, inflammation of adjacent tissues, complete loss), because the body cannot independently compensate for the pathological process. Against the background of the carious process, inflammation quickly penetrates into the pulp, then into the tissue surrounding the tooth. As a result, pulpitis and periodontitis occur.
Manifestations of caries in children
The appearance of light or dark spots on tooth enamel
The first sign of caries in children is white spots on the enamel, resulting from calcium loss. At this stage, treatment may be minimal; often the doctor prefers minimally invasive methods, for example the ICON technique. The dentist applies a special preparation to the affected tooth tissue, thereby blocking the proliferation of bacteria and the development of the infectious process - caries is “preserved.”
If the white areas darken, dentin, the deep tissue of the tooth, is involved in the pathological process.
Cavity formation
In a child, the caries process develops very quickly, and the next stage is the formation of cavities. Most often they are visible upon examination even with the naked eye, and the child complains of pain while eating.
Reaction to food temperature
With the further development of the carious process, the affected tooth begins to react to hot, cold and sweet foods and drinks.
Pain
Pain occurs while eating - when food gets on a carious tooth. If the infectious process has spread to the pulp, the child will complain of pain constantly. Often unpleasant sensations occur during night sleep.
5.Bad breath
Food particles accumulate in carious cavities, bacteria cause rotting, so parents often complain about bad breath.
How is decompensated caries treated?
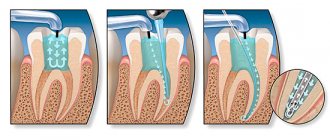
If a hole has already formed in the tooth, treatment will consist of preparing the dental tissue, opening it, cleaning the carious cavity, removing the nerve if necessary, and then filling it.
The decompensated form of caries is characterized by large-scale damage to the dentition, so it is often necessary to treat several teeth at once. Or several visits are scheduled for alternate treatment. This depends on the age of the patient, the extent of the carious lesion, the need for anesthesia and a number of other factors.
After treating all teeth affected by caries, the patient is scheduled for scheduled visits to the dentist at least 3-4 times a year. Also mandatory measures for decompensated caries are recommendations on proper nutrition and oral hygiene, consultation with a doctor, ingestion of anti-caries medications, sanitation of the oral cavity, and local prevention.
Classification according to the depth of the carious process
For a dental therapist involved in the treatment of caries, a topographic classification is more convenient:
- spot stage caries;
- uncomplicated simple caries;
Stain stage caries is the first stage of caries, in which the tooth enamel changes its color due to the formation of a so-called chalky stain on it. At the same time, the tooth remains smooth, since the enamel is still only in the initial stages of destruction. When diagnosing this stage, the most important task of the dentist is to stop the further development of the disease and its transition to the next stages of development.
In the earliest stages of caries, its therapy is considered a fairly simple task, is practically painless, takes a minimum of time (only one visit to the dentist is possible) and, accordingly, the least expensive. At the initial stage of caries, the dentist begins treatment of the tooth with the procedure of removing the stain, after which the enamel is remineralized, while the following preparations are applied to the neck of the tooth: sodium fluoride solution, calcium gluconate and others. Dentists can also use techniques such as infiltration-impregnation.
Superficial caries in the initial stage
At the stage of superficial caries, the surface of a timely undetected and unremoved chalk stain becomes rough due to demineralization of the enamel. In this case, the enamel-dentin junction of the tooth is not yet affected. The tooth at the site of superficial caries begins to hurt from cold food or hot food and may become sensitive to sweet or sour foods.
Treatment for this stage of caries will usually involve grinding down the area of the tooth. After grinding, just as in the case of the treatment of the previous, very first stage of caries, remineralizing therapy is performed.
But, in cases of caries localization in the fissures or on the contact surfaces of the teeth (these areas are the most susceptible to caries, since there are good conditions for food sticking and they are difficult to access for cleansing), then rem therapy becomes ineffective, so the dentist needs to prepare the affected area according to the classical method followed by filling. Superficial caries must be distinguished from such non-carious diseases as erosion of hard tissues and wedge-shaped defects.
Average caries
At the stage of average caries, the lesion begins to penetrate deeper. The enamel-dentin junction is affected, and the dentist can easily determine the deep pathology of the tooth. With average caries, the patient often feels pain, which becomes longer and more intense; pain, as a rule, occurs in the evening and at night, as a result of which the patient’s quality of life suffers greatly. Treatment of caries that has developed to a moderate form consists of removing the damaged part of the tooth and treating it with medications, followed by installing a filling of the desired type.
Deep caries
When, with advanced untreated caries, damage reaches the peripulpal dentin, the stage of deep caries begins. Therapy for deep caries consists of complete removal of the carious part of the tooth, followed by treatment of the damage with medications, the use of remineralizing drugs and filling. In the absence of treatment or inadequate therapy for this pathology, after the destruction of dentin, damage to the pulp occurs - pulpitis, which turns into periodontitis.
Complicated caries (pulpitis, periodontitis)
This classification takes into account the depth of the lesion, which is a determining factor for the choice of treatment method.
Caries in the initial stage (spot stage), superficial caries, medium caries with small defects are not detected on an x-ray. At the same time, it is very important to differentiate caries from other dental pathologies; for example, caries in the spot stage must be separated from such non-carious lesions as hypoplasia and fluorosis.
What these pathologies have in common is the formation of stains on the teeth, EOM (electroodontometry) readings are normal, and the absence of any discomfort. What are the differences: caries, unlike these two pathologies, can be detected when stained with special dyes, fluorosis and hypoplasia occur before teething, and caries always occurs after; caries is found in caries-susceptible areas, and non-carious pathologies in atypical (caries-resistant) areas.
Pulpitis as a complication of decompensated caries
The course of caries in a decompensated form can be complicated by inflammation of the neurovascular bundle - the pulp. The inflammatory process in this area is called pulpitis. It occurs when the infection spreads beyond the tooth
The pulp contains blood vessels, nerves, and nourishes dental tissue. If it becomes inflamed, there is a risk of tooth loss due to loss of vitality. With pulpitis, the patient complains of severe, prolonged pain, which is often pulsating in nature and radiates to the temples and ears. Painful attacks are repeated with a certain frequency, last for five minutes, intensify in a supine position.
Depending on the severity and neglect of the process, pulpitis is treated with a conservative or surgical method. At an early stage, the doctor, if possible, preserves the pulp and root of the tooth, eliminating the inflammatory process with the help of medications. If the inflammation is too strong, there is a risk of it going beyond the pulp, and it is not possible to stop the pathological process with medications, in this case the doctor chooses a surgical treatment tactic, partially or completely removing the pulp. This option is less preferable, because without a neurovascular bundle, the tooth becomes virtually “dead” and serves much less time.
The complications of caries should be taken seriously and at the first symptoms, contact your dentist. If you neglect timely diagnosis and treatment, the infection can spread to other organs and tissues, which can lead to serious disruptions in the functioning of the entire body. In particular, untreated pulpitis is dangerous for the development of gumboil, periodontitis, pulp necrosis and even sepsis.
Two-faced fluoride
If the first way to combat caries - giving up sweets - is not suitable for everyone, then making tooth enamel more resistant to acids is much easier. Today, the only internationally recognized and most effective way to strengthen enamel is still fluoridation.
For the first time, fluoride was added en masse to milk to prevent caries in schools and kindergartens in Switzerland in 1953. After 60 years, 95% of the world's toothpastes contain fluoride. If you read the ingredients in your toothpaste, you will most likely find sodium fluoride, monofluorophosphate, or aminofluoride in it. Or maybe there will be several fluorides. The mechanism by which all these substances help protect teeth from caries is very simple. Fluoride ions are introduced into the crystal lattice of mineral prisms of enamel, after which its solubility in acids decreases.
Periodontitis with decompensated caries
In addition to pulpitis, with decompensated caries another serious complication often develops - inflammation of the tissues surrounding the tooth root. This disease is called periodontitis.
The periodontium is a ligamentous apparatus that holds the tooth in the jaw and provides shock absorption. If an inflammatory process develops in the periodontal tissues, this can lead to loosening and tooth loss. Against the background of periodontitis, ulcers can form, the removal of which will require surgical opening of the gums.
Periodontal inflammation can be acute or chronic. In the first case, inflammation develops rapidly, accompanied by darkening of the tooth, acute pain, swelling of the affected tissues, and inflammation of the cheek. Chronic periodontitis is characterized by more smoothed symptoms, pain syndrome may be absent. Treatment for the chronic form is long and difficult and can take several months.
Periodontitis greatly weakens the immune system and creates a source of chronic infection in the body.
Is it possible to prevent tooth decay?
The development of any form of caries process is facilitated by a number of factors: poor diet with a large amount of carbohydrates, poor oral hygiene, insufficient intake of vitamins and minerals, rare visits to the dentist for the purposes of prevention and early diagnosis.
Addressing these risk factors helps reduce the risk of developing tooth decay or detect it at an early stage, when treatment can be as simple and effective as possible.
These preventive measures reduce the likelihood of developing any form of caries:
- Reducing the amount of carbohydrate and sweet foods in the diet, rare snacks, avoiding feeding the child at night and before bedtime. This recommendation is due to the fact that cariogenic bacteria feed primarily on carbohydrates. The longer food remains remain in the mouth, the more acid that is destructive to teeth will have time for microorganisms to produce.
- A balanced diet containing plenty of calcium, phosphorus and fluorine-containing foods. These minerals form a healthy and strong enamel structure that can resist the negative effects of cariogenic bacteria.
- Regular proper brushing of teeth using a brush, paste, floss, irrigator. Twice a year, professional teeth cleaning at the dental clinic. These measures help to get rid of dental plaque consisting of bacteria in a timely manner, and thereby reduce their negative impact on the teeth.
- Routine visit to the dentist even in the absence of complaints. With a compensated form of caries, it is recommended to visit a doctor once a year, with a subcompensated form - 2-3 times a year, with a decompensated form - 3-4 times a year. This recommendation is due to the fact that early caries often does not manifest itself with pronounced symptoms. For example, at the spot stage, the only sign of a carious lesion is whitish spots and lines on the enamel. It is quite difficult to notice them with the naked eye, but an experienced dentist will easily detect the beginning of the carious process.
If you miss the onset of the disease, a cavity forms in the tooth and complications develop. The later treatment is started, the more complex and painful it will be.
Indices used in dental examination
The prevalence of caries is expressed as a percentage. To do this, the number of people who were found to have certain manifestations of dental caries (except for focal demineralization) is divided by the total number of people examined in this group and multiplied by 100.
In order to assess the prevalence of dental caries in a particular region or compare the value of this indicator in different regions, the following assessment criteria for the level of prevalence among 12-year-old children are used:
Intensity level
LOW - 0-30% MEDIUM - 31 - 80% HIGH - 81 - 100%
To assess the intensity of dental caries, the following indices are used:
a) intensity of caries of temporary (baby) teeth: index kp (z) - the sum of teeth affected by untreated caries and filled in one individual;
index kp (n) - the sum of surfaces affected by untreated caries and filled in one individual;
In order to calculate the average value of the indices kp(z) and kp(p) in a group of subjects, one should determine the index for each person examined, add up all the values and divide the resulting amount by the number of people in the group.
b) intensity of caries of permanent teeth:
index KPU(z) - the sum of carious, filled and extracted teeth in one individual;
index KPU (n) - the sum of all surfaces of the teeth on which caries or a filling is diagnosed in one individual. (If a tooth is removed, then in this index it is considered 5 surfaces).
When determining these indices, early forms of dental caries in the form of white and pigmented spots are not taken into account. In order to calculate the average value of indices for a group, you should find the sum of individual indices and divide it by the number of people examined in this group.
c) assessment of the intensity of dental caries among the population. To compare the intensity of dental caries between different regions or countries, the average values of the KPU index are used.
WHO distinguishes 5 levels of intensity of dental caries:
Periodontal indices. CPITN Index
To assess the prevalence and intensity of periodontal diseases, almost all countries use the index of need for the treatment of periodontal diseases - CPITN . This index was proposed by specialists of the WHO working group to assess the condition of periodontal tissues during epidemiological surveys of the population. Currently, the scope of the index has expanded, and it is used to plan and evaluate the effectiveness of prevention programs, as well as calculate the required number of dental personnel. In addition, the CPITN index is currently used in clinical practice to examine and monitor the periodontal condition of individual patients. In this regard, the CPITN index can be considered a screening test at both the population and individual levels. This index registers only those clinical signs that may undergo reverse development: inflammatory changes in the gums, which are judged by bleeding, tartar. The index does not record irreversible changes (gingival recession, tooth mobility, loss of epithelial attachment), does not indicate the activity of the process and cannot be used to plan specific clinical treatment in patients with developed periodontitis. The main advantages of the CPITN index are the simplicity and speed of its determination, information content and the ability to compare results. To determine the CPITN index, the dentition is conventionally divided into 6 parts (sextants), including the following teeth: 17/14 13/23 24/27 34/37 43/33 47/44.
The periodontium is examined in each sextant, and for epidemiological purposes only in the area of the so-called “index” teeth. When using the index for clinical practice, the periodontium is examined in the area of all teeth and the most severe lesion is identified. It should be remembered that a sextant is examined if it contains two or more teeth that cannot be removed. If only one tooth remains in the sextant, it is included in the adjacent sextant, and this sextant is excluded from the examination. In the adult population, starting from 20 years of age and older, 10 index teeth are examined, which are identified as the most informative: 17/16 11 26/27 47/46 31 36/37.
When examining each pair of molars, only one code characterizing the worst condition is taken into account and recorded. For persons under 20 years of age, 6 index teeth are examined during an epidemiological survey: 16, 11, 26, 36, 31, 46
CODE 1 : bleeding observed during or after probing. Note: bleeding may appear immediately or after 10-30 seconds. after probing. CODE 2 : tartar or other plaque-retaining factors (overhanging edges of fillings, etc.) are visible or felt during probing. CODE 3 : pathological pocket 4 or 5 mm (the edge of the gum is in the black area of the probe or the 3.5 mm mark is hidden). CODE 4 : pathological pocket 6 mm deep or more (with the 5.5 mm mark or black area of the probe hidden in the pocket). CODE X : When only one or no teeth are present in the sextant (third molars are excluded unless they are in place of second molars).
To determine the need for periodontal disease treatment, population groups or individual patients can be categorized based on the following criteria. 0: CODE 0 (healthy) or X (excluded) for all 6 sextants means that there is no need for treatment for this patient. 1: A CODE of 1 or higher indicates that this patient needs to improve his oral hygiene status. 2: a) CODE 2 or higher indicates the need for professional hygiene and the elimination of factors that contribute to plaque retention. In addition, the patient needs training in oral hygiene. b) CODE 3 indicates the need for oral hygiene and curettage, which usually reduces inflammation and reduces pocket depth to values equal to or less than 3 mm. 3: Sextant with CODE 4 can sometimes be successfully treated with deep curettage and adequate oral hygiene. In other cases, this treatment does not help, and then complex treatment is required, which includes deep curettage. The prevalence and intensity of periodontal disease in the population is assessed based on the results of a survey of 15-year-old adolescents.
Gingivitis Index (GIA)
To assess the severity of gingivitis (and subsequently record the dynamics of the process), the papillary-marginal-alveolar index (PMA) . Various modifications of this index have been proposed, but in practice the PMA index as modified by Parma (1960) is more often used.
The RMA index is assessed using the following codes and criteria:
0—no inflammation; 1 - inflammation of only the gingival papilla (P); 2 - inflammation of the marginal gum (M); 3 - inflammation of the alveolar gum (A).
The PMA index is calculated using the formula: sum of PMA = ———————- x 100% 3 x number of teeth The number of teeth (while maintaining the integrity of the dentition) is taken into account depending on age: 6 – 11 years – 24 teeth, 12 – 14 years - 28 teeth, 15 years and older - 30 teeth.
Note: if there are missing teeth, then divide by the number of teeth present in the oral cavity. Normally, the PMA index is 0. The higher the digital value of the index, the higher the intensity of gingivitis.
Evaluation criteria for the RMA index:
30% or less - mild gingivitis; 31-60% - moderate severity; 61% and above—severe degree.
Oral hygiene assessment
Fedorov-Volodkina hygienic index (1971)
The index is recommended to be used to assess the hygienic state of the oral cavity in children under 5-6 years of age. To determine the index, the labial surface of six teeth is examined: 43, 42, 41, 31, 32, 33. These teeth are stained using special solutions (Schiller-Pisarev, fuchsin, erythrosine) and the presence of plaque is assessed using the following codes: 1 - plaque not identified; 2 - staining one quarter of the surface of the tooth crown; 3 - staining half the surface of the tooth crown; 4 - staining three quarters of the surface of the tooth crown; 5 - staining the entire surface of the tooth crown. Determination of supra- and subgingival tartar is carried out using a dental probe.
Codes and criteria for assessing dental calculus
O —tartar is not detected; 1 - supragingival tartar, covering no more than 1/3 of the tooth surface; 2 - supragingival tartar, covering more than 1/3, but less than 2/3 of the tooth surface, or the presence of individual deposits of subgingival tartar in the cervical area of the tooth; 3 - supragingival calculus covering more than 2/3 of the tooth surface, or significant deposits of subgingival calculus around the cervical area of the tooth.
The calculation of the index consists of the values obtained for each component of the index, divided by the number of surfaces surveyed, followed by the summation of both values.
Formula for calculation:
IGR-U stone values = ———————————- + ——————————— quantity. number of surfaces surfaces
Evaluation criteria
a) IGR-U values: Level of oral hygiene 0, 0 - 1, 2 good 1, 3 - 3, 0 satisfactory 3, 1 - 6, 0 poor
b) Values of plaque or tartar indicators: 0.0 - 0.6 good 0.7 - 1.8 satisfactory 1.9 - 3.0 bad
Oral Hygiene Performance Index (OHP) Podshadley, Haley, (1968)
To quantitatively assess dental plaque, 6 teeth are stained: 16, 26, 11, 31—vestibular surfaces; 36, 46 - lingual surfaces.
1 - medial 2 - distal 3 - mid-cervical 4 - central 5 - mid-occlusal
Codes and criteria for assessing dental plaque
O - no staining 1 - staining detected
The index is calculated by determining the code for each tooth by adding the codes for each section. Then the codes for all examined teeth are summed up and the resulting sum is divided by the number of teeth:
The index is calculated using the following formula:
sum of codes of all teeth RNR = —————————————————— number of teeth examined
Evaluation criteria
Index value Hygiene level 0 excellent 0.1 - 0.6 good 0.7 - 1.6 satisfactory 1.7 or more unsatisfactory
Dental aesthetic index NC Cons et al., (1986)
A special dental aesthetic index is used to assess the condition of the bite. In the clinic, the index is used at the individual level and when conducting epidemiological surveys of the population. This index determines the position of the teeth and the state of the bite in the sagittal, vertical and transversal directions. Recommended for use from 12 years of age in key age groups. The examination is carried out visually and using a button probe. The index includes the definition of the following components: • lack of teeth; • crowding in the incisal segments; • gap in the incisal segments; • diastema; • deviations in the anterior part of the upper jaw; • deviations in the anterior region of the lower jaw; • anterior maxillary overlap; • anterior mandibular overlap; • vertical front gap; • anteroposterior relationship of molars. Lack of teeth. The number of incisors, canines and premolars on the upper and lower jaws is counted (from 15 to 25 and from 35 to 45) and the number of missing teeth in this group is determined.
Teeth are not considered removed if: 1. with a missing tooth, the space is closed; 2. the baby tooth is in the dentition, but the permanent tooth has not yet erupted; 3. The space is restored with a bridge. Crowding in the incisal segments. Each segment consists of 4 incisors. Crowding is a condition of the dental arches when the space between the right and left canines is not enough to accommodate all 4 incisors in a normal position. The teeth may be rotated or out of line with the arch.
Codes and evaluation criteria
O - no crowding 1 - crowding of one segment 2 - crowding of two segments
Spacing in incisal segments. Gap is a condition where the space located between the right and left canine teeth is greater than the space required to accommodate all 4 incisors in their normal position. If one of the incisors has proximal surfaces without interproximal contact, the segment is considered to have a spacing. If the bite is mixed, you should not consider the space from a recently fallen temporary tooth to be empty if it is obvious that the permanent tooth will erupt soon.
Codes and criteria:
O - no gap in segment 1 - one segment with a gap 2 - two segments with a gap. If in doubt, evaluate to a lower score. Diastema is the space between the two permanent upper central incisors. Measurements are taken with a button probe at any level between the mesial surfaces of the teeth and expressed in mm.
The largest deviation between adjacent teeth is measured. To do this, the tip of a button probe is placed on the labial surface of the tooth most deviated in the lingual direction or rotated around its axis at an angle of 90° to the normal line of the dental arch. Registered in mm. Anterior maxillary overlap. The measurement is carried out in central occlusion. The working part of the periodontal probe is placed parallel to the occlusal plane and the distance (in mm) from the labial-incisal edge of the most protruding upper incisor in relation to the labial surface of the lower incisor projected onto it is assessed. This index component is not taken into account if all the upper incisors are missing and/or in a lingual position (crossbite). If the incisors close to the edge, then you can put code 0. Anterior mandibular overlap. This sign is assessed when either lower incisor is advanced anteriorly or vestibular to the opposing upper incisor. The greatest forward movement of the tooth (in mm) is recorded. Measurements are carried out in the same way as on the upper jaw.
If there is no occlusion on the first molars due to the absence of one or two teeth, incomplete eruption or disruption of their shape due to caries or filling, then the relationship of the canines or premolars is determined.
Codes and criteria:
O - norm 1 - displacement by 1/2 of the tuberosity mesially or distally in relation to the norm 2 - displacement by the size of the tuberosity mesially or distally in relation to the norm.
The dental aesthetic index allows you to analyze each of the components of the index or group them by anomalies of the dentition and bite.