The treatment of “fluxes” is carried out by a dental surgeon.
Do you feel afraid of the dentist?
Flux is the common name for any swelling in the cheek area and partly the neck - periodontitis, periostitis, complications of pulpitis and other inflammations. If you have inflammation of any origin or form, localized on the gums and in the oral cavity in general, you should definitely see a dentist.
What is oral candidiasis?
Oral candidiasis (also called oral thrush) is an infection of the mouth caused by the yeast-like fungus Candida. These microorganisms are part of a healthy microflora, but under certain circumstances their reproduction disrupts the favorable environment and becomes a source of disease processes. Inflammation and plaque on the tongue, ulcers on the mucous membrane and discomfort in the mouth - this disease is called oral candidiasis.
Infants are most susceptible to this disease, but at this age it is treated faster and is tolerated almost painlessly. Oral thrush is often observed in adults after 50 years of age, when the immune system is already weakened. Oral candidiasis is less common in men than in women. Recently, the percentage of cases has increased significantly, which is associated with uncontrolled use of medications: weakening of cellular immunity increases the risk of oral candidiasis after antibiotics, or rather their improper use. Microbiology, the science of microorganisms, studies the essence of oral candidiasis. And she successfully copes with her task, at the moment this disease has been studied in detail, and doctors know all the methods of treating and preventing infection.
Causes of oral candidiasis
A healthy person is still a carrier of fungi of the genus Candida, since they are part of the microflora and calmly coexist with other microorganisms without causing harm. But any change in the balance in the body can lead to rapid proliferation of bacteria and the development of disease. A weakened state of immunity plays a key role in the etiology of oral candidiasis, but any of these reasons can be the starting point for the onset of the disease:
- pregnancy;
- immunodeficiency states;
- infectious processes;
- long-term treatment with antibiotics or improper use of medications;
- injuries and damage to the oral mucosa;
- insufficient oral hygiene;
- contact with an already sick person.
Diagnosis of oral candidiasis
Candidiasis (thrush) of the oral cavity can be detected during an examination by a dentist if the patient has characteristic complaints. The doctor examines the condition of the oral mucosa, examines scrapings, and carefully examines the hair and skin. If you have oral candidiasis, you also need a blood test to check your glucose levels and rule out diabetes. The sooner you detect the presence of this infection, the easier it will be to get rid of it, so you should not delay diagnosis just because the symptoms do not cause you discomfort.
Symptoms of oral candidiasis
- Infection is characterized by the appearance of swelling and a whitish coating on the mucous membranes of the cheeks, lips, and tongue. When the plaque is removed, the surface bleeds, and the patient experiences a burning sensation.
- With oral candidiasis, the tongue and throat become sensitive, and any contact is painful for the patient.
- Signs of oral candidiasis also include cracks in the corners of the lips and redness of the mucous membrane.
- Symptoms of oral thrush include severe dry mouth, a feeling of tightness of the mucous membrane, and roughness of the internal surfaces.
- Patients often complain of increased temperature due to oral candidiasis. Sometimes this disease is accompanied by the appearance of small ulcers on the inside of the lip and cheek mucosa, which are filled with pus and emit a characteristic odor of oral candidiasis.
Signs of oral candidiasis in HIV diseases are slightly different from traditional ones. In this case, the infection spreads quickly and immediately becomes acute, and plaques and plaque appear not only in the mouth, but also in the genital area. With HIV, thrush of the oral mucosa is difficult to treat, so even with minor symptoms it is better to visit a doctor and check your health.
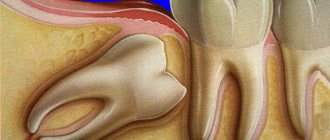
Flux symptoms
Clinical manifestations of acute periodontitis/periostitis are quite characteristic. Flux manifests itself as sharp pain in the tooth area, intensifying even with light pressure on it. Swelling and redness of the lips, cheeks, enlarged gums, and the tooth is often mobile.
There is an unpleasant odor from the mouth, and sometimes fistulas on the gums. A characteristic sign of gumboil is the appearance of independent pain, weak at first, then intensifying, becoming pulsating and tearing. Its difference from pain with pulpitis is that it is strictly localized and becomes sharp when pressing on the diseased tooth, especially in the form of tapping. The closing of teeth is so painful that many people refuse to eat even liquid food.
Clinical manifestations of acute periodontitis/periostitis are quite characteristic. Flux manifests itself as sharp pain in the tooth area, intensifying even with light pressure on it. Swelling and redness of the lips, cheeks, enlarged gums, and the tooth is often mobile.
There is an unpleasant odor from the mouth, and sometimes fistulas on the gums. A characteristic sign of gumboil is the appearance of independent pain, weak at first, then intensifying, becoming pulsating and tearing. Its difference from pain with pulpitis is that it is strictly localized and becomes sharp when pressing on the diseased tooth, especially in the form of tapping. The closing of teeth is so painful that many people refuse to eat even liquid food.
It is also possible to increase body temperature to 37.5-38.0°C. Severe pain and difficulty eating food force the patient to see a dentist within the next few hours from the moment of illness.
Chronic form of periodontitis
In chronic forms of periodontitis, a different picture is observed. The most formidable and insidious in its course and possible complications is chronic granulating periodontitis and exacerbation of its course. The pain reaction is mild, but often in the vestibule of the oral cavity, in the projection of the apex of the root of the affected tooth, a fistula periodically opens with small purulent discharge.
When the fistula is closed during periostitis, swelling and hyperemia of the mucous membrane in the area of the flux and pain when pressing on the diseased tooth are possible. Chronic granulating periodontitis is diagnosed based on a comparison of clinical manifestations with X-ray data, which shows destruction of the periodontal gap and changes in the jaw bone in the form of “tongues of flame” in the area of the apex of the tooth root. The purulent process in the medullary spaces of the jaw adjacent to the periodontium leads to the spread of infection over a considerable distance.
The vital activity of pathogenic microflora during the long-term existence of a chronic pathogenic focus ultimately leads to odontogenic chronic sepsis. This provokes the emergence, formation or exacerbation of chronic infectious diseases of the heart, liver, kidneys and other organs.
The presence of such infectious foci can dangerously affect the course of pregnancy at any stage; complications such as infection of the female genital area, miscarriage, and disruption of the formation of fetal tissue occur.
Classification of oral candidiasis
This disease is usually divided into several types, each of which has its own characteristic features. Experts distinguish between acute and chronic oral candidiasis.
Acute pseudomembranous candidiasis
Characteristic of infants with weakened immunity. Oral candidiasis, or oral candidiasis, can be triggered by a previous infectious disease or gastrointestinal disorder. The disease is transmitted through a pacifier or dishes; the disease manifests itself in the form of a light or grayish coating on the mucous membrane. At the initial stage, plaque is painlessly removed; with the development of candidiasis of the oral mucosa and pharynx, it thickens and spreads in the oral cavity. It is almost impossible to remove plaque on the tongue without causing bleeding.
Acute atrophic candidal stomatitis
Accompanied by peeling of the integument, dryness and burning of the mucous membrane, it is painful for the patient to eat and touch the infected area. With this form of oral candidiasis, the infection can spread further - to the larynx, pharynx and even the esophagus.
Chronic hyperplastic candidiasis of the oral cavity
It is characterized by a change from a whitish coating to a grayish-yellow one, after removal of which slight bleeding occurs. Along with plaque, plaques and thickenings appear that cannot be cleaned off or removed; they go away on their own during the treatment process.
Chronic atrophic candidiasis of the oral cavity
It is diagnosed when inflammation spreads to the skin and cracks appear in the corners of the mouth. In this case, the tongue becomes a shiny, rich pink color, and the vessels are clearly visible on it. Then the infection spreads to the internal organs. This type of oral candidiasis can occur due to improper installation of dentures, plates and crowns, which rub and injure the mucous membrane.
Ulcers as local manifestations of general diseases on the oral mucosa
- Oral tuberculosis
is usually a secondary manifestation of pulmonary tuberculosis. It occurs as a result of penetration of tuberculosis bacteria into the oral mucosa through damaged epithelium. The membranes of the cheeks, tongue, and floor of the mouth are affected. First, typical tuberculous tubercles are formed, and then, after their disintegration, small ulcers are formed, which increase in size over time. The ulcer itself is not deep, with a loose bottom, which is covered with easily bleeding granulations (young tissue), uneven edges are observed, soft to the touch. With this disease, there is a sharp pain in the ulcer. In addition to the local manifestation in the form of an ulcer, there is a general deterioration in the well-being of patients: emaciation is noted, the amount of plaque on the tongue increases, sweating and body temperature increase. General treatment of tuberculosis of the oral mucosa is carried out in specialized anti-tuberculosis institutions. As for local treatment, in this case, sanitation of the oral cavity is carried out during the period of remission (weakening of the disease), treatment of the mucous membrane with antiseptic and anti-inflammatory agents. - Syphilis
is a chronic infectious disease caused by the so-called Treponema pallidum. All periods of development of this disease (in addition to the incubation period, which lasts 21 - 24 days) are characterized by the presence of ulcers in the oral cavity. At the initial stage of development of the disease, the presence of a painless ulcer is observed, which has a round or oval shape with raised, smooth edges and a cartilage-like specific infiltrate. The bottom of the ulcer is bright red, shiny or covered with a grayish-dark coating. The ulcers heal in 3 to 12 weeks with or without scar formation. Even with tertiary syphilis, there is no sharp pain, as, for example, with a tuberculous ulcer. The ulcer is surrounded by a powerful infiltrate, which is a dense bluish-red ridge that rises above the level of the mucosa. Its edges are smooth, bright red, covered with granulations, and bleed easily. After the ulcer heals, a retracted star-shaped scar forms. This process lasts 3 - 4 months. After the ulcers heal, scars remain, which are a sign of previous syphilis. General treatment of syphilis is carried out in a venereology hospital, local treatment is carried out during the period of remission or recovery (sanitation of the oral cavity, elimination of local traumatic factors). - Acute necrotizing gingivostomatitis
is a viral infectious disease. Most often, ulcers are localized on the mucous membranes of the gums, cheeks, soft palate, arches and tonsils. Favorable factors for the development of this disease are a decrease in the overall resistance of the body, a violation of the integrity of the oral mucosa, and a deficiency of vitamins in the body. There are also cases of this disease occurring against the background of cooling or overwork. It can also be a complication of viral infections, as well as allergic stomatitis. Usually young people (under 30 years of age) are affected, more often men.
Among the symptoms it is necessary to highlight: pain when eating; extremely unpleasant odor from the mouth; increased salivation; elevated body temperature. The gum mucosa becomes swollen, painful, and bleeds when touched. The epithelium of the gingival margin and gingival papillae becomes cloudy. The surface of the gingival margin is covered with a grayish-yellow coating, which is easily removed. The ulcers have soft, uneven edges and are covered with a dirty green coating (with a foul odor), which is easily removed. In this case, a loose bleeding bottom is detected. The surrounding tissues are swollen.
Treatment of necrotizing gingivostomatitis is carried out in accordance with the general condition of the body, taking into account its location and severity of the lesion. In moderate and severe stages of the disease, broad-spectrum antibiotics are prescribed, as well as drugs that prevent or reduce the manifestation of allergies. At any stage of development of the disease, vitamins C and P, high-calorie foods, juices are prescribed, and in some cases, according to indications, taking cardiac medications.
Local treatment is carried out under anesthesia (removal of necrotic tissue). The oral cavity is treated with warm solutions of antiseptics and anti-inflammatory drugs. The ulcer is also sprinkled with white clay powder. After acute inflammation has been relieved, professional oral hygiene is carried out.
Mouth ulcers can also form due to HIV (gum ulceration occurs in approximately 30% of people infected with HIV). How to cure mouth ulcers in this case? Treatment is specific and carried out by infectious disease doctors. Dental care is provided in all dental institutions with careful adherence to safety precautions.
Prevention of all of the above oral diseases consists of eliminating the causes of their occurrence. For example, to prevent infectious diseases that manifest themselves on the oral mucosa, such as syphilis, measures are necessary that prevent infection from entering the body. In other cases, wellness measures are very important, which include systematic independent and professional oral hygiene, which is offered by almost all dental clinics in Moscow.
Treatment of oral thrush
The treatment of this disease is carried out by the dentist, although he may seek advice from a therapist, immunologist or endocrinologist. To get rid of this disease, there are many medications, from which a specialist will choose the one that is right for you. Do not forget that different medications are used to treat oral candidiasis in adults and children. Also, to speed up recovery, you should follow a special diet that your doctor will prescribe; it is important for restoring the mucous membranes after candidiasis of the mouth and throat. Many patients neglect visiting a specialist and prefer advice from those who have already encountered this infection, as well as traditional methods. Such behavior is extremely dangerous; oral candidiasis cannot be treated based on reviews on forums or recommendations from friends. This can provoke unforeseen complications and cause serious harm to health. The doctor will accurately determine the cause of your disease and prescribe a drug that is suitable for your physiological characteristics. Read more about the treatment of oral candidiasis in the article.
What to do if your cheek is swollen
To reduce swelling, you can use one of the following tips:
- Rinse your mouth with a solution of salt and soda.
This remedy has an antiseptic effect and helps destroy pathogens. You can enhance the effect by adding a couple of drops of iodine to the solution.
- Use chamomile infusion to rinse
, sage or other medicinal herbs that have anti-inflammatory properties.
- Apply a cold compress to the swollen cheek
if the swelling is caused by a bite or mechanical injury. This method is contraindicated in patients who have an elevated body temperature or a tumor that develops due to inflammatory processes. Warming compresses are not recommended.
- Lotions with aloe or Kalanchoe juice.
A cotton wool soaked in the juice of the plant is applied to the inside of the affected cheek.
If the described methods do not eliminate the problem, you should seek help from a doctor. The day before, you should not take painkillers and anti-inflammatory drugs, so as not to complicate the diagnosis.
Prevention of oral candidiasis
The occurrence of this disease is a very unpleasant and painful phenomenon, fortunately, it is quite easy to avoid by following the recommendations. One of the main causes of infection is weakened immunity, so the basic rule for preventing the disease is to treat any disease at the right time and take medications strictly as prescribed by the doctor. To avoid candidiasis of the oral cavity, pharynx and larynx, hygiene, visiting a good dentist, professional ultrasonic cleaning and other preventive measures will help. Oral candidiasis in women is often due to hormonal imbalance; if you have symptoms of the disease, you should pay attention not only to the affected area, but also to the condition of the body as a whole.
The dangers of flux and the dentist's tasks
It is the identification of such foci and their elimination, especially in persons suffering from inflammatory processes of internal organs and in pregnant women, that is one of the essential tasks of a dentist. Untimely sanitation of the oral cavity or its absence in the presence of teeth affected by chronic periodontitis can lead to the development of a number of more severe inflammatory processes, the first of which is acute purulent periostitis.
Purulent periostitis
This disease is an acute purulent inflammation of the periosteum of the alveolar process of the jaw and accounts for up to 40% of complications of odontogenic infection, mainly chronic periodontitis. The cause of the development of this disease is most often large molars, which are primarily affected by the carious process.
The clinical picture of acute purulent periostitis is diverse and depends on the nature of the microflora, localization and extent of the inflammatory process. When the upper jaw is affected, the external manifestations of acute inflammation, in particular hyperemia, infiltration and swelling of soft tissues, are usually more pronounced than when the flux is localized in the lower jaw. However, the phenomena of general intoxication are more pronounced when the alveolar process of the lower jaw is affected, which is due to the difference in the anatomical and topographic relationships of soft tissues and jaw bones.
When examining the oral cavity, smoothness or swelling of the transitional fold of the mucous membrane of the vestibule of the oral cavity, its hyperemia, and sharp pain when touched by the dentist’s hands or instruments are noticeable.
It should be borne in mind that the pain in the “causal” tooth due to the release of exudate (liquid released into the tissue or cavity of the body from small blood vessels during inflammation) beyond the periodontal gap subsides to a certain extent, but slight mobility of the tooth appears. This circumstance sometimes serves as a justification for delaying visiting a doctor and as a cause of aggravated course of the inflammatory process in the future.
The diagnosis of “acute purulent periostitis” is an absolute indication for surgical intervention in the form of opening and drainage of the periosteal purulent focus and removal of the “causal” tooth.
Options for non-drug treatment (physiotherapy) depend on the patient’s general condition, age, and concomitant chronic diseases. In the latter case, the volume and nature of drug treatment is determined by the dentist of the appropriate profile. It is especially important to carry out adequate treatment in patients suffering from rheumomyocarditis, diabetes mellitus, nephritis and some other chronic diseases.
Another complication of chronic granulating periodontitis is the development of acute odontogenic osteomyelitis , accompanied by the formation of phlegmons and abscesses of the cellular spaces of the face and neck.
These complications of flux are the most severe and dangerous result of the progression of odontogenic infection, and depending on the location and nature of the microflora, they can lead to severe complications including the development of sinus thrombosis and mediastinitis.
It is their timely diagnosis in somatic patients that largely determines the outcome of the disease.
The clinical manifestations of phlegmon are different and depend on the location of the flux (deep, superficial), the nature of the pathogen (aerobic, anaerobic flora), body resistance, concomitant diseases, age, etc.
Today, persistent, sluggish chronic necrotic processes in the bone and soft tissues of the face often occur against the background of drug addiction.
Deep phlegmons of the pterygomaxillary, infratemporal, peripharyngeal spaces are manifested by sharp pain of the corresponding localization, severe manifestations of general intoxication up to acute intoxication psychosis, severe inflammatory contracture of the masticatory muscles, pain when swallowing, with an almost complete absence of external manifestations: hyperemia, infiltration, fluctuations, etc. .
Underestimation of certain symptoms of gumboil can lead to a delay in seeking dental care, ineffective therapy and progression of the inflammatory process.