What are blockades
Therapeutic blockades are the relief of acute or chronic pain and spasms. It is performed by injection into the area where the nerve trunks and plexuses pass. Severe pain causes physical and psychological suffering, incapacitates the patient and can cause disability. Depression that occurs against this background often leads to suicide attempts.
Therapeutic blockades quickly relieve acute pain. After some time, swelling, inflammation, spasm of muscles and blood vessels decrease. This leads to a lasting improvement in the condition. At the 100med medical center, blockades are performed by neurologists and anesthesiologists. Several groups of drugs are used for the procedure:
- local anesthetics;
- corticosteroid hormones;
- chondroprotectors.
The effect of drug administration lasts from several days to several weeks. After the medicine stops working, the pain may return. However, its severity will be less by about 50%.
During the procedure, the patient may feel some discomfort associated with the injection. However, the discomfort quickly passes. There is no need to be afraid of blockades, as this method is one of the safest. Our specialists strictly follow all the rules for performing the procedure, as well as asepsis and antiseptics. This guarantees the effectiveness and safety of blockades in our clinic.
Neuropathy of the superior alveolar nerve.
The causes of the disease may be chronic pulpitis and periodontitis, nerve damage in case of complex tooth extraction, sinusitis, and surgical intervention for sinusitis.
It manifests itself as pain and a feeling of numbness in the teeth of the upper jaw. Objectively, there is a decrease or absence of sensitivity in the gum area of the upper jaw, as well as the adjacent area of the buccal mucosa. The electrical excitability of the pulp in the corresponding teeth of the upper jaw is reduced or absent.
If the cause of the disease is stenosis of the infraorbital canal, then patients will complain of pain and numbness of the skin in the area of innervation of the infraorbital nerve (wing of the nose, area above the canine fossa, upper lip).
Nerve block
A nerve block is a treatment in which a local anesthetic is injected into the soft tissue where the peripheral nerve passes. The procedure allows you to relieve pain, spasm of muscles and blood vessels, swelling and inflammation. Indications for manipulation:
- neuritis;
- neuralgia;
- tunnel syndrome;
- muscular-tonic syndrome;
- diseases of the spine;
- pain after injury or surgery;
- chronic pain syndrome;
- oncological diseases.
Nerve blocks do not require special preparation. After a thorough examination and examination of the patient, the doctor determines the injection site and treats the skin with an antiseptic. An injection of pain medication is given into the soft tissue. After a few minutes, numbness, warmth and a feeling of heaviness appear in this place. The course of injections (up to 3 sessions) can be repeated every year.
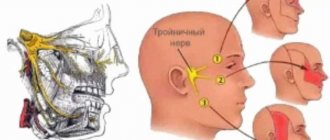
Iatrogenic trigeminal neuropathy.
This nosological entity arose due to the fact that treatment of trigeminal neuralgia in most cases began with neurodestructive operations (alcohol-lidocaine blockades, neuroexeresis, destruction of the trigeminal ganglion). As a result, a significant number of patients experienced iatrogenic traumatic or toxic-traumatic neuropathies of the trigeminal nerve. The maxillary and mandibular nerves were most often affected.
In many textbooks on neurology, in case of trigeminal neuralgia, it is proposed to carry out alcohol-novocaine and alcohol-lidocaine blockades of its peripheral branches or node - the so-called alcoholization . The analgesic effect in this case is achieved on average after the second or third procedure, but it is explained by the fact that numbness occurs due to the development of destructive changes in the nerve trunk. Over time, toxic-traumatic neuropathy develops, practically resistant to treatment, so the patient must continue to undergo blockades, the effectiveness of which decreases in proportion to their number.
Thus, neurodestructive operations that are performed in the treatment of neuralgia lead to the development of toxic-traumatic neuropathy. This determines the nature of the pain syndrome.
Clinic.
The clinical picture is usually represented by the presence of constant aching, burning or dull neuropathic pain in the area of innervation of the affected nerve, against the background of which neuralgic paroxysms occur with irradiation of pain, respectively, to the segmental areas of the face (Zelder segments). Patients experience various types of paresthesia (numbness, crawling, burning) and sensitivity disorders (hypesthesia with symptoms of hyperpathia or hyperesthesia), which sometimes spread beyond the innervation of one of the branches of the trigeminal nerve.
In many cases, vegetative fibers are drawn into the process, which leads to trophic changes in the oral mucosa (gingivitis), the dental system (progressive periodontitis) and facial skin (pigmentation or depigmentation, dryness, peeling, soft tissue atrophy). In such cases, the pain becomes unbearably burning, tearing, boring, and is accompanied by vegetative reactions (redness and swelling of the facial skin, local increase in body temperature, lacrimation, salivation).
During neurodestructive manipulations on the mandibular nerve, painful contraction of the teeth may occur (patients are forced to eat through a straw and cannot speak or open their mouth). With each subsequent alcoholization, the nature of the pain syndrome changes: neuralgic paroxysms become longer, more frequent, a neuralgic status can form, and slightly pronounced trigger areas appear on the skin of the face. Pain is provoked by weather conditions (cold or heat), exacerbation of somatic pathology, food consumption, and physical activity. The exit points of the trigeminal ditch are painful during palpation in approximately 2/3 of patients.
The data presented convincingly indicate that neurodestructive manipulations are not the method of choice for the treatment of trigeminal neuralgia, since in most cases a short-term effect is achieved. However, such therapy leads to the development of toxic neuropathy, disease progression and the development of resistance to conservative treatment methods. Only when all the methods used to treat neuralgia are not effective, and the intensity of the pain syndrome remains severe, can neurodestructive operations recently developed by neurosurgeons be used.
Joint blockade
Joint blockade is a method of introducing a drug into the joint cavity or adjacent soft tissues (articular capsule). The method not only relieves pain, but eliminates inflammation, relieves muscle and vascular spasm, and restores range of motion in the joint. The procedure is indicated for the following diseases:
- arthritis of joints of various sizes;
- arthrosis;
- arthralgia;
- synovitis;
- bursitis;
- tendovaginitis;
- periarthritis;
- facet syndrome;
- Reiter's disease;
- Bekhterev's disease.
The injection is performed without additional preparation after a thorough examination. The patient is seated or laid on a couch and the skin over the joint is treated. The injection is made into the cavity of the joint capsule, into the area of the periarticular ligaments or bursa. The effect occurs within a few minutes and lasts up to 3 weeks. The duration of the course depends on the severity of the lesion and can be up to 15 procedures.
Traumatic neuropathy. Etiology.
Traumatic neuropathy most often occurs in the case of surgical interventions on teeth (traumatic extraction of teeth, removal of filling material beyond the apex of the tooth root, anesthesia with injury to the nerve trunks, removal of bone or tumor of the jaws), as well as in cases of surgical interventions on the paranasal sinuses and infraorbital canal.
Damage to the first branch of the trigeminal nerve, as a rule, is practically not observed. Most often, the third branch of the trigeminal nerve is affected, which is apparently due to the anatomical location of the inferior alveolar nerve, which makes it easily accessible during a variety of traumatic dental procedures. This is especially true for dental interventions on third molars. The cause of traumatic neuropathy of the inferior alveolar nerve can also be filling the mental canal during the treatment of pulpitis of the 4th and 5th teeth of the lower jaw.
Combined damage to the I and II branches of the trigeminal nerve can occur after inflammatory diseases of the brain with the development of adhesions or in the case of sinusitis, when the maxillary and frontal sinuses are simultaneously involved in the inflammatory process.
Clinic.
Patients complain of constant aching, sometimes pulsating pain in the area of innervation of the injured nerve, a feeling of numbness and “crawling goosebumps”. In case of injury to the mandibular nerve, tooth alignment occurs, which is associated with damage to the motor part of the nerve; patients cannot eat or talk. Trigger zones on the face and in the oral cavity are not identified.
During an objective examination, hypoesthesia or anesthesia (hyperpathy is also possible) of the skin and mucous membrane in the area of nerve innervation is detected. On palpation, pain is noted at the exit points of the II and III branches of the trigeminal nerve, as well as in the case of vertical percussion of the teeth and deep palpation of the lower jaw.
Diagnostics.
The main diagnostic criterion is the occurrence of pain after interventions on the dental system. The disease is characterized by clinical polymorphism and significant duration. During weather changes, stressful situations and in the presence of somatic diseases, exacerbation of the pain syndrome may occur.
In the event of scar changes in the nerves or retraction of the nerve into the scar of soft tissues (after gunshot wounds, in the case of defects of soft and bone tissues after resection of the jaws), constant aching pain of unexpressed intensity with persistent sensory disturbances is observed.
Celiac plexus block
With this type of blockade, the medicine is injected into the solar plexus area. The injection is done under the control of an X-ray machine or ultrasound.
The procedure is effective for:
- chronic pancreatitis, pancreatic necrosis;
- abdominal adhesions;
- Crohn's disease;
- tumors of the abdominal organs;
- ineffectiveness of painkillers.
You should prepare for the blockade in advance. A few days before the procedure, the doctor at our clinic recommends stopping taking anticoagulants and diuretics and adjusting the dose of glucose-lowering medications. The patient is placed on his stomach with a bolster or pillow. First, the doctor anesthetizes the soft tissue at the injection site. Then, under X-ray control, a special long needle is inserted. Through it, a local anesthetic or a drug that destroys nerve cells is supplied to the solar plexus. The patient feels warmth in the abdomen and a decrease in pain. After the procedure, observation is required in our hospital for 24 hours.
Paravertebral blockade
Paravertebral blockade is performed to reduce pain in the spine. The effect is achieved by blocking the ganglia or spinal nerves on one or both sides. Indications for this are:
- osteochondrosis;
- radiculitis, lumbago;
- neuralgia;
- myositis;
- hernias and protrusions of intervertebral discs;
- spinal injuries.
To carry out the manipulation, the patient is placed on a flat couch. Local soft tissue anesthesia is first performed. The medicine is injected into the segment of the spine where the pain is felt the most. The injection is given on one or both sides depending on the patient’s condition.
Epidural block
An epidural block is the injection of medication into the space between the dura mater and the periosteum of the spinal canal. Depending on the injection site, caudal, translumbar, and transforaminal blockades are distinguished. A good effect of blockades is observed when:
- damage to the radicular nerves;
- periduritis;
- intervertebral hernias;
- spondylolisthesis;
- narrowing of the spinal canal;
- back pain after injury or surgery.
The procedure must be carried out on an empty stomach. The patient is placed on a couch, and the doctor applies local anesthesia to the desired area. Then, under the control of an X-ray machine, a needle is inserted through which the medicine is administered. When performed correctly, the patient feels a slight burst in the back.