An abnormality such as bone spurs is often ignored until it actively progresses. Patients often come to the clinic late, which entails complex treatment, including surgery. Exostosis is a pathology in which hardened areas of cartilage tissue protrude above the jaw are formed. The causes of this phenomenon are mechanical damage, trauma, tooth extraction and other diseases. Chewing functions are preserved, and soft tissues are also not damaged. But as the protrusions grow, thinning of the mucous membrane and ruptures occur, causing injury to surrounding areas.
Main symptoms
Depending on the specific type, epulis can manifest itself in different ways:
- Fibrous. Doesn't hurt and grows very slowly. The shade of the neoplasm does not differ from the color of the gums. In the absence of therapy, it can reach large sizes.
- Angiomatous. Has a rich purple hue. Causes pain, for example, when chewing food. It is easy to damage during mechanical action (even when brushing your teeth). Sometimes it bleeds.
- Giant cell. The most dangerous type of epulis. Can degenerate into a cancerous tumor. Typical for adults. It has a bright red color, even the slightest palpation causes discomfort.
Based on the stage and age, the growth can be dense or soft, and can range in size from several millimeters to 10 centimeters in diameter.
Causes
Reasons for the formation of growths:
- inflammatory, infectious processes, purulent accumulations;
- mechanical impacts, injuries causing bone destruction, jaw displacement and other damage;
- deviations of row segments, formation of nodular hardenings;
- disorders of the endocrine system, hormonal levels.
One of the reasons for the development of pathology is complex tooth extraction. Often, when a wound heals, the tissue around it becomes overgrown with moving areas. If done incorrectly, compactions may appear and exostosis will gradually develop.
How to treat?
Gum treatment should begin as soon as you notice growth. In most cases, you have to resort to surgical intervention, since drug therapy in this case does not have a positive result. The growth is excised under general or local anesthesia. After removal of the epulis, it is recommended to send the biomaterial for histological examination to exclude the malignant nature of the neoplasm.
Next, the doctor prescribes antibiotics and anti-inflammatory drugs to avoid possible complications. For speedy healing, wound healing and antiseptic agents may be prescribed.
Why does exostosis occur on the gums after tooth extraction?
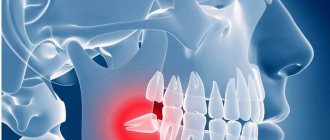
The cause of the growth is excessive growth of bone tissue. This mechanism is triggered when they are damaged, which occurs during the extraction of teeth or a jaw fracture. Usually bones are injured during complex operations to extract molars. After wisdom tooth removal, exostosis is diagnosed more often than other cases.
Factors that provoke pathological bone growth:
- hereditary predisposition;
- infections, inflammation in the oral cavity;
- injuries during dentofacial operations;
- endocrine disorders.
After tooth extraction, the patient may feel small nodules with his tongue. Over time, they increase in size and cause concern.
Preventive actions
You can prevent damage to the integrity of the gums in the following ways:
- Brush your teeth more carefully, without pressing too hard on the brush.
- Use solid foods with caution.
- Clean the seeds with your hands, not your teeth.
- If there are artificial structures in the mouth, make sure that they do not cause discomfort in the form of rubbing. This mainly applies to removable dentures.
- Use orthodontic wax when wearing braces.
- Carry out dental treatment in a timely manner.
- Do not consume too hot foods or drinks to avoid burns.
- Go to the dentist twice a year to have tartar removed.
Remember that this pathology has a predisposition to relapse. Most often, such cases occur in people who do not follow basic hygiene rules. Be more attentive to the condition of your oral cavity, brush your teeth daily and use additional hygiene products. Be careful not to cause mucosal damage.
Indications and contraindications
If the formation is large, leads to inflammation of the mucous membranes of the oral cavity, jaw deformation, or interferes with talking or chewing food, then it is removed. The operation is also prescribed before prosthetics, since even small bumps become an obstacle to the installation of implants.
The patient himself can contact the surgeon if the bone spike spoils the aesthetics of the face. In this case, it is located on the buccal side and the protruding part is visible externally. An aesthetic defect gives a person more psychological discomfort than physical discomfort.
Before the procedure, the surgeon excludes contraindications. The list of restrictions includes infections in the mouth, acute respiratory infections, diabetes mellitus in the stage of decompensation, poor blood clotting, exacerbation of chronic diseases, mental disorders, childhood, pregnancy and a number of other contraindications.
For children, surgery is delayed until they are 18 years old. This is due to the fact that the bones are still growing and the pathology can resolve on its own.
Wisdom tooth: inflammation of the hood and its symptoms
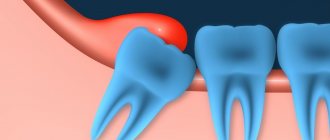
Patients who have inflamed gums near a wisdom tooth usually complain to the doctor that their wisdom tooth is growing, their gums are swollen, and there is also an odor from the wisdom tooth. The formation of an unpleasant odor is caused by the formation of pus, which is gradually released from under the hood. Patients also complain of pain in the area of the wisdom tooth. Such symptoms correspond to only a mild form of pericoronitis.
What do the symptoms of pericoronitis look like in the video? Please note that in the video below you can see the following symptoms: redness and swelling of the hood above the upper wisdom tooth, a small amount of purulent discharge (white) from under the hood. Such symptoms correspond to a mild form of inflammation.
If pericoronitis occurs, treatment is only possible with a dental surgeon. But at the initial stage, patients try to relieve the symptoms on their own using available means: antiseptic rinses, dental drops, painkillers. In most cases, this is ineffective and the inflammation only increases. The following symptoms increase (in various combinations):
increasing pain- severe swelling and redness of the gums,
- swelling of the cheek (Fig. 4),
- purulent discharge from under the hood,
- painful swallowing
- difficulty opening the mouth,
- increase in body temperature,
- weakness,
- swelling and tenderness of the submandibular lymph nodes.
Important: if at this stage the wisdom tooth hood has not yet been removed (see below), then you should be prepared for the next development of events. Firstly, because inflammation occurs in the area of the masticatory muscles - their spasm can lead to almost complete closure of the mouth. If at this moment you decide to go to the dentist, then he will not be able to do anything for you if your mouth is not opening enough, except to refer you to the hospital.
Secondly, pus may begin to spread not into the oral cavity, but rather deep into the bone and soft tissues, which will cause the formation of an abscess or phlegmon (peripharyngeal or submandibular). The latter complications will also mean inevitable treatment in a hospital, and therefore it is better not to bring the inflammation of the wisdom tooth to a critical level.
Pericoronitis: treatment
If you have inflammation of the gums near the wisdom tooth, the treatment most often consists of a dental surgeon removing the hood over the wisdom tooth. However, if severe purulent inflammation is observed, then complete excision of the hood is undesirable immediately, because this can lead to various inflammatory complications.
In case of severe purulent inflammation, the hood is first only dissected to facilitate the outflow of purulent discharge, and anti-inflammatory therapy is prescribed. And the doctor will prescribe you for its complete removal after the active inflammation has subsided. Also, in some cases, the doctor may recommend immediately removing the wisdom tooth (24stoma.ru).
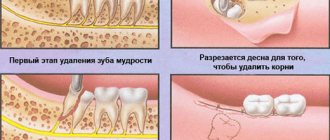
Excision of the hood over the wisdom tooth –
Removing the hood of a wisdom tooth involves excision of the overhanging mucous membrane over the erupting eighth tooth. Excision of the hood over the wisdom tooth leads to the elimination of conditions for the proliferation of pathogenic bacteria. This minor surgical procedure is usually less traumatic, but in some cases a large amount of gum tissue must be excised.
Excision of the hood over the wisdom tooth is performed by a dental surgeon under local anesthesia. The procedure is completely painless if you see a good specialist, if the anesthesia is administered correctly and a good anesthetic is used, and not something like novocaine. Pain will appear only after anesthesia has passed (after 30 minutes), so it is worth taking an analgesic even before the pain appears.
- Hood removal: price for 2021 in an economy class clinic in Moscow, a similar service costs about 2,500 rubles. In the regions, the cost of the procedure may be 2 times lower. By the way, in the clinic at your place of residence (if you have an insurance policy and a passport), you should undergo this intervention completely free of charge.
Stages of excision of the hood –
- Conducting local anesthesia,
- Using a scalpel and surgical scissors (less commonly, a surgical laser), the dental surgeon excises the gum overhanging the tooth.
- Treating the wound with antiseptics.
- An iodoform turunda is usually placed in place of the excised hood.
- The doctor gives recommendations and schedules a re-examination.
Removing a wisdom tooth hood: video
Please note that both hood excision operations are performed with a surgical laser and not with a scalpel. Using a laser avoids bleeding, swelling and severe pain. In Russian dental clinics, lasers are practically not used (due to their absence), and only a few clinics can boast of their presence.
After the intervention, the following are prescribed:
- Antiseptic baths with chlorhexidine solution 0.05% (3-4 times a day);
- Antibiotics are not prescribed in every case;
- for pain - good tablet analgesics.
Usually this is enough for you to completely forget what wisdom tooth pericoronitis is after 4-5 days.
However, if the doctor performed the operation traumatically, the pain may last for 7-10 days. If you want to remove inflammation as quickly as possible, then after antiseptic rinses, you can additionally apply CholisalGel to the hood 2 times a day in the morning and evening (it has a pronounced analgesic and anti-inflammatory effect). Remember that if you put gauze soaked in iodoform on the wound surface, you need to remove it yourself no later than the next day. Then it itself will become a breeding ground for infection. After you take out this turunda, it may cover a little. Then it is advisable to treat the wound with a gauze swab soaked in 3% hydrogen peroxide.
Important: in some cases, the hood may form again, in which case either a repeat operation may be required, or the issue of tooth extraction will be decided. Often these teeth are in an incorrect position. An experienced doctor can quickly determine the chances of the eighth tooth taking the correct position using an x-ray and external examination of the tooth.
In what cases is it better to immediately remove a tooth with a hood -
If your gums near your wisdom tooth are inflamed, the most radical treatment method will be the removal of the 8th tooth, above which the ill-fated hood appears.
This will solve the problem permanently, but you must be prepared for the fact that the eighth teeth may have curved roots (this can be checked by taking a photo) and then removal may be difficult. Situations where deletion is the best solution to the problem -
- Firstly , when the lower jaw is insufficiently long, which means there is not enough space for the eruption of a wisdom tooth. Removal in this case will prevent the remaining teeth from being displaced by the erupting tooth, and will prevent the development of crowding of teeth in the anterior part of the lower jaw.
- Secondly , if the 8th tooth has a strong inclination towards the cheek or the seventh tooth, then it will still have to be removed sooner or later, because it will injure either the buccal mucosa or the root of the 7th tooth, respectively.
For more information about the difficult eruption of wisdom teeth, read the article: → “Features of the growth and eruption of eighth teeth”