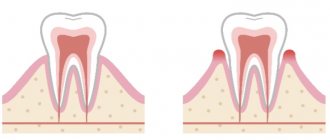
Concrete pulpitis is an inflammatory disease caused by the presence of denticles or petrification (calcifications) in the canals and pulp chamber.
The formation of these formations occurs practically asymptomatically; they can appear even in intact (not affected by diseases) teeth.
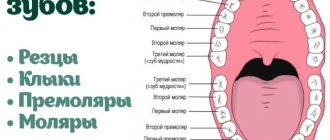
According to statistics, every tenth pulpitis is concremental, in most cases it develops in premolars and molars in people over 35-40 years of age.
Many foreign researchers combine the concepts of denticles and petrificates under the same name, concretions or pulp stones, although this is not true.
Causes of denticles
The exact reasons have not yet been established, since this dental phenomenon has not yet been fully studied. It is assumed that the appearance of denticles can be accompanied by various injuries to the dentition, functional inactivity of the tooth, and injuries received during its preparation.
The following factors can provoke the development of mineralized deposits:
- inflammatory processes in the pulp;
- poor quality dental treatment;
- impaired metabolism in the pulp and periodontal tissues;
- age-related changes in tooth and gum tissues;
- endocrine diseases.
Often, the development of denticles is promoted by hormonal disorders, diabetes mellitus, hypertension, severe infectious diseases and lack of minerals.
general information
Age-related changes occurring in the body affect the intensity of deposition of calcium salts in the pulp. Petrifications are detected in 9 out of 10 patients in the older group, but can also be diagnosed in younger or middle-aged patients. The local formation is concentrated mainly in the root region of the pulp chamber, has a round or curved shape, and reaches a size of up to 2-3 mm. Denticles can also be located in the structure of the crown, and in special cases - completely repeat the structure of the pulp.
The cause of ectopic dentin formation is a metabolic disorder, inflammatory foci, hypovitaminosis, as well as other factors. Compression of the pulp leads to a painful syndrome and disruption of the natural microcirculation within the unit. It is noted that the formation of denticles may be a consequence of the functioning of cellular odontoblasts.
In the normal state, the formations practically do not manifest themselves - such a structure is characterized as concremental pulpitis of a chronic nature. Painful symptoms occur when there is a sudden change in the spatial position of the body, leading to the displacement of a stone. Typical circumstances include flying on an airplane, riding in an elevator, skiing, as well as other situations in which provoking factors arise. Identification of denticles in a calm state is possible during an X-ray examination of the dentition.
Features of the disease
The denticles themselves do not cause discomfort unless they compress the nerve endings of the pulp. Due to their small size, they can be almost invisible. Sometimes, during development, denticles fuse with each other, then they can be detected on an x-ray. If left untreated, denticles grow uncontrollably and fill the entire pulp chamber, making further dental treatment impossible. Due to such fused formations, root canal treatment becomes problematic, and in such cases the patient is recommended to have the tooth removed.
Features of the course, diagnosis and treatment
The disease is characterized by long-term, sluggish development and the absence of clinical manifestations in the anamnesis. During a dental examination, a change in the coloration of the crown of the tooth may be observed. As the inflammatory process develops, paroxysmal pain appears, more pronounced at night. Mostly, the patient can accurately identify the causative tooth.
Clinical manifestations
In most cases, the formation of denticles is not accompanied by clinical manifestations; they are discovered accidentally during an X-ray examination of the teeth, which is carried out in connection with the treatment of other dental diseases. Painful sensations occur if the nerve bundle is compressed by denticles or petrification, when formations are displaced, as well as during the development of the inflammatory process.
Radiologically, the formations look like multiple or single dense shadows, having a round or irregular shape, located inside the cavity of the tooth and its canals.
Diagnostic features
The clinical manifestations of concremental pulpitis are quite similar to the symptoms of trigeminal neuralgia, so the disease is differentiated from it. The table shows the main differences:
| № | Characteristic | Concrete pulpitis | Neuralgia |
| 1. | Pain | Increasing attack of dull pain | Sudden onset of acute pain |
| 2. | Time of attack | Mostly nocturnal | Any time of day |
| 3. | Novik's test | Pain occurs with sudden changes in position | Negative |
| 4. | Percussion | Sharp pain when tapping on the crown of a tooth | Absent |
| 5. | Causal tooth | Determined | Not determined |
| 6. | X-ray result | Dense formations in the tooth cavity are clearly visible | No tissue changes |
| 7. | Development | The disease develops slowly, in which the intensity and number of attacks constantly increases | Painful attacks are constant and do not change intensity. |
| 8. | Manifestations from the autonomic nervous system | No | Eat |
Treatment method
The main stages of treatment for concremental pulpitis are the same as for other types of inflammatory nerve diseases. Thanks to modern techniques and materials, all stages of therapy in most cases take one visit. The general treatment plan for pulpitis is as follows:
- anesthesia;
- preparation of carious cavity and canals;
- instrumental and medicinal treatment;
- obturation (filling with filling material);
- filling a carious cavity.
The differences lie in the complexity of preparing and filling obliterated (deposit-filled) canals with filling material. To pass them through, a special ultrasound device is usually used, but for large stones this does not always lead to a positive result.
The prognosis is favorable; in the absence of a tendency to excessive growth, denticles do not cause problems for the doctor and the patient. Treatment is most often carried out in full, and inflammatory symptoms completely disappear and do not recur.
To avoid the development of complications during treatment, it is necessary to promptly contact the dentist and conduct an examination of the dental system. There is no way to prevent the formation of denticles and petrification, but you can reduce the risk of their occurrence. To do this, it is necessary to treat inflammatory dental diseases in a timely manner, preventing the formation of foci of pulp necrosis, which subsequently mineralize.
Classification of denticles
Depending on their location, denticles are:
- Free (most often found directly in the pulp tissue, in isolation; if dentin is formed intensively, they grow together with the inner walls of the tooth, becoming parietal denticles);
- Adjacent, or interstitial (initially based at the inner walls of the tooth cavity).
Depending on the structure, denticles are divided into two groups:
True denticles are synthesized directly on the pulp tissue. The formations are similar in structure to dentin and have dentinal tubules. They are localized mainly at the top of the root canal. They are quite rare.
False denticles form independently as a result of necrosis of adjacent tissues. They do not have a dentin-like structure and tubules.
Regardless of the type of denticles, it is necessary to get rid of the problem as soon as it was discovered, since this can negatively affect the condition of the pulp of the diseased tooth.
What are denticles, the reasons for their formation
Dentin-like areas formed from root or coronal pulp tissue as a result of the development of replacement dentin are called denticles. The formations are round or irregular in shape and tend to merge into conglomerates, causing obliteration (blockage) of the entire lumen of the canal.
Structurally, the inclusion consists of a core, which is a fine petrificate, surrounded by tissue with dentinal tubules, and its chemical structure resembles natural tooth tissue. The development mechanism is as follows - pulp tissue cells are transformed into odontoblast-like and form dentin-like tissue.
Causes and mechanism of development
The true reasons for the development of denticles are not fully understood, but scientists believe that the factors provoking the development of these formations may be:
- injuries – dislocations and fractures of the roots of both permanent and baby teeth;
- dental manipulations - treatment for crowns, the presence of metal fillings, orthodontic structures;
- various health problems - metabolic disorders, development of thyrotoxicosis, excess vitamin D and lack of vitamins A and C in the body, long-term therapy with hormonal drugs;
- inflammatory and degenerative diseases of the periodontium (tissues surrounding the tooth);
- age-related changes in the dental system – increased wear of teeth, involution (reverse development) of soft tissues;
- hereditary imperfect formation of dentin is the most pronounced example of dysplasia that develops with Stanton-Capdepont syndrome.
Denticle occupying the entire pulp cavity
Treatment
- The first thing that is done is pain relief, because the slightest touch to the affected pulp tissue causes severe pain, which prevents any manipulation of the tooth. Sometimes, in addition to injections of analgesic into soft tissues, intrapulpal anesthesia is also given.
- Damaged and necrotic areas of the pulp are removed, mineralized deposits are cleaned off.
- A rubber dam is installed to isolate the exposed dental canal from saliva.
- The tooth cavity is treated with special antiseptics.
- A hypoallergenic non-rejectable gasket is placed on the cleaned bottom of the cavity.
- An insulating layer is placed on top of the gasket.
- The tooth is filled with a temporary filling. Then, as the antiseptic works and the destructive processes are stopped, the temporary filling is replaced with a permanent one.
- Conservative treatment methods with oral administration of drugs will not give results, so it will not be possible to do without penetration into the dentin and pulp.
Symptoms
Acute pulpitis:
- Severe throbbing pain radiating to neighboring teeth, ear, throat, temple.
- Reaction to hot and cold, including cold weather.
- Painful attacks occur after certain periods of time and intensify in a supine position.
Fibrous pulpitis:
- The pain is aching in nature, worsening in the evening and at night.
- A feeling of “bursting” and heaviness in the affected tooth.
- A sharp temperature reaction that continues after removal of the irritant.
Gangrenous pulpitis with an open lesion cavity:
- Discomfort and heaviness in the area of the affected tooth.
- Pain when biting.
- Reaction to hot drinks and food with prolonged persistence of aching pain.
- The enamel is gray, the gums are red and swollen, there is a fistula.
- Putrid odor from the mouth.
Gangrenous pulpitis with a closed lesion cavity:
- Intense pain attacks.
- Vivid reaction to hot drinks and food with pain persisting for a long period of time.
These symptoms help you pre-diagnose the presence of pulpitis and consult a dentist as soon as possible.
Diseases of the pulp and periapical tissues of the tooth
Diseases of the pulp and periapical tissues of the tooth
Pulpitis is an inflammation of the dental pulp, the most common pathological process in it. Other pulp changes are called reactive.
Classification. By etiology, pulpitis is distinguished: sterile, caused by physical and chemical factors: traumatic, thermal (for example, when treating a tooth for an artificial crown), radiation, decompression, toxic (including iatrogenic, caused by medications and filling materials in violation of treatment technology) ; infectious (usually bacterial).
By localization in the pulp: coronal, total, root.
Clinical and morphological types of pulpitis: acute serous focal and diffuse; acute purulent focal (abscess) and diffuse (phlegmon); chronic granulating; chronic fibrous; gangrenous (pulp gangrene).
Depending on the response to treatment: reversible and irreversible (the transition point is often bacterial invasion of the pulp).
Acute serous pulpitis can be focal (often close to the carious cavity) and diffuse, often sterile and reversible (with complete repair - restitution of the damaged pulp), usually occurs within several hours. However, it can develop into acute purulent or chronic pulpitis.
Acute focal purulent pulpitis (pulp abscess) develops with bacterial invasion of the pulp (Fig. 1).
Rice. 1. Acute focal purulent pulpitis. In the coronal part of the dental pulp there is a focal accumulation of neutrophilic leukocytes (purulent exudate) with histolysis of the pulp tissue and colonies of microorganisms (abscess), inflammatory hyperemia, diapedetic hemorrhages and edema. Retrograde demineralization of hard dental tissues. Dentinal tubules are filled with basophilic colonies of bacteria (basophilic stripes - 1). Hematoxylin and eosin staining, x 100.
Acute diffuse purulent pulpitis (pulp phlegmon) spreads to the coronal and root pulp. It takes on a grayish color, and multiple abscesses in it look like small yellowish dots. Under the influence of purulent exudate, destruction of nerve fibers occurs, which explains the decrease in the characteristic intense pain in the later stages.
Chronic pulpitis, like acute pulpitis, is usually a consequence of the carious process. It can be an independent nosological form or be the outcome of acute pulpitis.
Granulating pulpitis is characterized by the replacement of the pulp with granulation tissue with petrificates and denticles, with chronic inflammatory infiltration, death of odontoblasts, lacunar resorption of dentin, and its replacement with osteodentin (Fig. 2).
Rice. 2. Chronic granulating pulpitis. Maturing granulation tissue with lymphomacrophage, with an admixture of leukocytes, infiltration, inflammatory hyperemia, balloon degeneration of odontoblasts. Hematoxylin and eosin staining, x 200.
Its special form is chronic hypertrophic pulpitis (pulp polyp). It occurs mainly in children and young people with carious destruction of the tooth crown. Excess granulation tissue protrudes beyond the pulp cavity in the form of a kind of mushroom-shaped growth (polyp) with an ulcerated surface. The surface of the polyp can be represented by multilayered squamous epithelium, “creeping” from the adjacent parts of the gum.
Chronic fibrous pulpitis is formed as a result of granulating pulpitis during the maturation of granulation tissue. The tooth cavity is filled with whitish dense scar tissue with foci of stromal hyalinosis, petrificates and denticles. Gangrenous pulpitis (pulp gangrene) is rare. Its inclusion in the group of chronic pulpitis is conditional, because it represents necrosis of the pulp when the tooth cavity is opened. Subsequently, the resulting grayish-black tissue detritus becomes compacted and encapsulated. Part of the pulp may remain viable.
Complications and outcomes. Typically, the duration of acute purulent pulpitis is 3-5 days. Purulent pulpitis, especially diffuse, without treatment usually ends in the death of the pulp, the formation of chronic pulpitis or fibrosis and pulp atrophy. Chronic pulpitis leads to atrophy and functional failure of the pulp. A complication of acute pulpitis or exacerbation of chronic pulpitis is acute apical (apical) periodontitis.
Reactive changes in the pulp are divided into alterative, discirculatory and adaptive.
Alternative changes include, first of all, reversible (to a certain extent) intracellular accumulations in odontoblasts: hydropic (vacuolar) and fatty degenerations, which usually develop with pulpitis, mucoid and fibrinoid swelling of connective tissue and the walls of pulp vessels (for example, in rheumatic diseases ), as well as necrosis (gangrene) of the pulp.
Hyalinosis of the stroma and walls of pulp vessels in chronic pulpitis is local in nature, but it can be, especially in vessels, a manifestation of general diseases (arterial hypertension, diabetes mellitus, rheumatic diseases, etc.).
Necrosis is the death of pulp tissue when the tooth cavity is closed, and gangrene is called when it is opened. Pulp necrosis can be partial or total.
Dyscirculatory changes. Disorders of blood and lymph circulation in the pulp tissue can be local in nature (trauma, inflammation) or be a manifestation of general discirculatory disorders.
Adaptive processes. Pulp atrophy makes its connective tissue stroma prominent (reticular pulp atrophy), while its trophic ability to provide dentin production decreases.
Pulp sclerosis can be focal or total when it spreads to the entire pulp chamber, which is often observed as the outcome of chronic fibrous pulpitis.
Petrification of the pulp is one of its frequent reactive changes. In the pulp there are: necrocalcinosis - calcification of necrotic masses); fibrocalcinosis - deposition of calcium salts in areas of pulp sclerosis, i.e. in scar tissue; thrombocalcinosis - calcification of thrombotic masses.
Denticles are isolated inclusions of dentin in the pulp or dentin layer of a tooth. They are formed by odontoblasts and consist of reparative dentin. According to their location, denticles are intrapulpal (free), surrounded by pulp; parietal (parietal) - at the border of the dentin layer and pulp tissue; interstitial (intradental) - in the thickness of the dentin layer. By structure, denticles are highly differentiated (represented by mature dentin, similar to the replacement irregular dentin of a carious cavity) and low-differentiated (consisting of areas represented by dentin and calcifications).
Adaptive processes also include the formation of secondary, replacement or irregular dentin, which is, in particular, characteristic of late stages of caries.
Intrapulpal cysts (pseudocysts) are cavities in the pulp tissue that are not found normally; they can be solitary (single) or multiple. The reasons for their occurrence are different, from inflammatory to reactive processes.
Apical (apical) periodontitis is an inflammation of the periapical tissues, which has its own nosological significance. There is also marginal periodontitis (inflammation of the marginal periodontium) - a manifestation of periodontitis.
Classification. According to etiology, infectious and non-infectious (traumatic, toxic, including iatrogenic) apical periodontitis is distinguished. The causative agents of infectious periodontitis are mainly streptococci and staphylococci. Non-infectious periodontitis is associated with the ingestion of drugs and injuries (dentures, bad habits, occupational diseases).
Clinical and morphological forms: acute (serous and purulent); chronic - granulating, granulomatous (simple granuloma; complex or epithelial granuloma; cystogranuloma), fibrous.
Pathogenesis. The most common route of spread of infection into the periapical tissues through the opening of the tooth apex is descending from the inflamed pulp; contact is less common - from neighboring tissues (bone alveolus, marginal periodontium, cement) with periodontitis, osteomyelitis, cement caries, even less often - ascending (hematogenous or lymphogenous ).
In acute serous apical periodontitis, acute serous inflammation is observed in the periapical tissues, and in acute purulent apical periodontitis, an abscess or phlegmon develops. Purulent periodontitis is accompanied by perifocal serous inflammation of the surrounding soft tissues with severe swelling (flux, lat. - parulis) and periostitis. A pronounced pain syndrome is characteristic, tooth mobility appears, and the patient also has the feeling of an “overgrown tooth.” The duration of the disease is from 2-3 days to 2 weeks.
Acute purulent apical periodontitis. In the tissue of the dental ligament in the area of the apex of the tooth root there is an abundant accumulation of neutrophilic leukocytes (purulent exudate) with histolysis of periapical tissues (apical periodontal abscess - 1), 2 - dentin, 3 - alveolar bone. Hematoxylin and eosin staining, x 100.
The inflammatory process can spread under the periosteum or into the jawbone with the development of acute purulent osteomyelitis, and in the upper jaw - odontogenic sinusitis (sinusitis). Subsequently, the inflammatory process progressing in the bone marrow spaces can reach the periosteum and cause the formation of a subperiosteal (subperiosteal) abscess. Subsequently, a submucosal abscess may develop. Further progression of the suppurative process or resorption of exudate and scar formation, or transition of the pathological process to chronic apical periodontitis is possible.
Chronic apical granulating periodontitis is characterized by the growth of granulation tissue in the peri-apical region of the tooth with a delay in its maturation, with focal or diffuse inflammatory infiltration. Resorption of the bone tissue of the dental alveoli occurs, destruction of the compact substance of the bone and periosteum, as well as hard tissues of the tooth root (cementum and dentin). Lacunar resorption of dentin areas by macrophages with its replacement by osteodentin is observed (B.I. Migunov, 1963). Granulation and inflammatory infiltration can spread to the perimaxillary soft tissue. During exacerbation, the inflammatory process often takes on a purulent character and abscesses form. In such cases, sometimes a gingival fistula opens in the area of the apex of the tooth root, through which pus is released. A fistula tract that opens on the skin (external fistula) may also occur, and the location of the fistula with a high degree of probability can be used to judge the localization of chronic granulating periodontitis.
Chronic apical granulomatous periodontitis is characterized by the development of a periapical “granuloma”. This formation has nothing to do with granuloma in the modern understanding of this term from the standpoint of general pathology. Periapical granuloma is a spherical or oval formation tightly attached to the apex of the tooth root. It is located inside the resorbed bone of the dental alveolus and on radiographs has the appearance of a clearly limited focus of enlightenment. As the periapical granuloma grows, bone destruction progresses. Granuloma consists of granulation tissue with chronic inflammatory infiltration, surrounded by a dense capsule of mature connective tissue (simple granuloma). You can find Roussel's bodies, cholesterol crystals, giant cells of foreign bodies (Fig. 3)
Rice. 3. Chronic apical granulomatous periodontitis (simple granuloma). In the area of the apex of the tooth root there is granulation tissue with inflammatory infiltration, surrounded by a fibrous capsule. The bone tissue in the area of the granuloma is destroyed. Hematoxylin and eosin staining, x 60.
Among the granulation tissue, strands of multilayered squamous epithelium can grow of different sizes and shapes, differentiating from the remains of odontogenic epithelium in the periodontium - Malasse islands (epithelial granuloma). The volume of epithelial inclusions and the shape of such complexes can be different (Fig. 4).
Rice. 4. Chronic apical granulomatous periodontitis (epithelial granuloma). Strands of non-keratinizing squamous epithelium from the islets of Malasse penetrating granulation tissue with inflammatory infiltration. Hematoxylin and eosin staining, x 200.
Epithelial granuloma, due to the development of inflammatory, dystrophic and necrobiotic processes in granulation tissue, over time transforms into cystogranuloma, which is distinguished by a cavity lined with multilayered squamous non-keratinizing epithelium of odontogenic origin. Cystogranuloma can reach a diameter of 0.5 - 1 cm (Fig. 5, 6). Later, it can transform into a radicular (root) cyst of the jaw bone (see section on jaw bone cysts).
Rice. 5. Cystogranuloma (arrow). X-ray.
Rice. 6. Cystogranuloma. Detritus with cholesterol crystals in the forming cavity of the cystogranuloma, the walls of which are represented by maturing granulation tissue with inflammatory infiltration and in places covered with stratified squamous epithelium. Hematoxylin and eosin staining, x 60.
Chronic fibrous apical periodontitis is characterized by the proliferation of coarse fibrous connective tissue in the peri-apical region. This form of periodontitis is inactive and the most favorable.
Complications and outcomes. In favorable cases, the outcome of apical periodontitis with adequate and timely treatment may result in the restoration of previously resorbed bone tissue of the dental alveoli and the formation of fibrous periodontitis. With any type of chronic apical periodontitis, exacerbations of the inflammatory process with the formation of abscesses can be observed. Complications of chronic, less often acute apical periodontitis are abscesses and phlegmons in the slit-like spaces of the soft tissues of the face and neck with the risk of developing septic thrombosis of the cavernous sinus, brain abscess or purulent meningitis, as well as purulent mediastenitis. In addition, swelling of the larynx is dangerous, which can lead to death as a result of asphyxia. Also among the most serious, often fatal complications of apical periodontitis are osteomyelitis of the jaw bones, odontogenic sepsis, Ludwig's angina (caused by group A streptococci, putrefactive-necrotic phlegmon of the tissue of the floor of the mouth, peripharyngeal and pterygo-maxillary space and neck).
Purulent-inflammatory processes in which the entrance gate of infection is a tooth are called odontogenic infections. They are characterized by a predominantly contact route of spread. The most common sources of odontogenic infection are chronic forms of apical periodontitis with exacerbation, suppurating radicular cysts, alveolitis (inflammation of the bone alveolus after tooth extraction).
When the inflammatory process spreads into the tissue of the jaw bones in conditions of sensitization to infection, osteomyelitis of the jaw develops (see section on diseases of the jaw bones), which can later become a source of odontogenic sepsis. Ontogenic sepsis is sepsis in which the entrance gate and septic focus is caries and its complications: apical periodontitis, periostitis, osteomyelitis, abscesses and phlegmons of the soft tissues of the face, neck, floor of the mouth, etc.
Age-related changes in the pulp –
Even after the complete formation of a tooth, with age there is a gradual reduction in the size of the pulp chamber. This occurs as a result of continuous deposition of secondary dentin as well as intermittent deposition of tertiary dentin. Consequently, at a more mature age, the pulp will occupy a significantly smaller volume than at a young age. In addition, the shape of the pulp chamber itself changes (as a result, the pulp horns are smoothed out).
All this also has clinical significance, for example, deep preparation of dentin in the area of the pulp horns in old age will be less dangerous. In addition, with age there is a decrease in the number of cellular elements in all layers of the pulp (up to 50% of the initial level), but at the same time the content of collagen fibers increases 3 times. The blood supply to the pulp deteriorates due to the reduction of a large number of capillaries (especially those located in the capillary plexus in the Weil layer). Loss of nerve fibers also occurs, and in particular, this is associated with an age-related decrease in the sensitivity of the pulp to irritants.
With age, the frequency of formation of calcifications in the pulp also increases. Although, if calcification occurs not locally, but diffusely, then this process is called petrification. Petrifications most often form in the root part of the pulp (along the periphery of vessels, nerves, and also inside the vascular wall), sometimes causing disturbances in the blood supply to the pulp and pain. We hope that our article was useful to you!
Sources:
1. Higher professional education of the author in dentistry, 2. The European Academy of Paediatric Dentistry (EU), 3. “Anatomy of human teeth” (Gayvoronsky, Petrova). 4. “Periodontology” (Danilevsky N.F.), 5. “Pulpitis of temporary and permanent immature teeth” (Mamedova).